Medical expert of the article
New publications
Key cells in a smear in women and men: reasons for detection
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Many human diseases are hidden from view and have no obvious external manifestations. But they can easily cause the development of other diseases that have obvious symptoms and unpleasant consequences. A bacterial infection caused by the proliferation of opportunistic microflora can manifest itself in this way. But only a laboratory study of the biomaterial can detect and recognize such an infection. When it comes to female diseases, the doctor always takes a smear in the area of the vagina or uterus where the infection is suspected. Sometimes the doctor finds key cells in the smear, and such an analysis can seriously alarm the woman. In fact, we are usually talking about such a common violation of the vaginal microflora as dysbacteriosis, although more dangerous pathologies should not be excluded.
What do key cells mean in a smear?
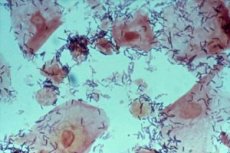
This is the question women ask, most often suspecting that we are talking about oncological pathology, sexually transmitted diseases, dangerous viruses, etc. These suspicions are groundless in most cases, because doctors call the key cells in the smear flat epithelium with bacteria concentrated on its surface from the category of pathogenic or opportunistic microflora. The presence of key cells in a vaginal smear in most cases indicates the development of bacterial vaginosis (gardnerellosis), caused by opportunistic bacteria with the strange name of gardnerella. If epithelial cells with microflora glued (adhered) to them, other than gardnerella, are found in the biomaterial, they are called false key cells in the smear.
Vaginosis pathogens are detected by bacterioscopy. First, the patient is examined by a gynecologist on the chair and a smear is immediately taken for microflora. Then, in the laboratory, the collected biomaterial is examined under a microscope. This is a traditional method for diagnosing most diseases of the genitourinary system, which has become widespread in gynecology.
Gardnerella under the microscope look like small rods dotting the surface of the flat epithelium taken during a smear. Ideally, an insignificant amount of such bacteria is found on the vaginal mucosa, and they do not pose a danger to either the woman or her sexual partner. The main inhabitants of the internal environment of the vagina are lactobacilli (95%) and some other types of beneficial bacteria that are accustomed to living in an acidic environment. But it is lactic acid bacteria that maintain the pH of the vagina. It is with their help that the woman's body takes care of the health of the genital area.
For pathogenic and opportunistic bacteria, the acidic environment of the vagina is not particularly suitable for life, since it reduces their activity and prevents reproduction. They can only wait for the acidity of the internal environment to shift towards alkalization. And this can only happen if the number of lactobacilli decreases compared to the norm.
A change in microflora towards a decrease in beneficial bacteria is called dysbacteriosis. In this case, the place of lactobacilli is occupied by actively multiplying cocci and rod-shaped bacteria, which are present in the vagina in minimal quantities, but are not found in smears of a healthy woman. The presence of key cells in a smear indicates a bacterial gynecological pathology.
Such elements most often indicate bacterial vaginosis (dysbacteriosis of the vagina), but in some cases they can also be detected with erosion of the uterus, as well as with dysplasia (precancerous condition). Even more rarely, they can be detected at an early stage of oncological pathology, with polyposis of the uterus and other neoplasms of an inflammatory nature.
Depending on the detected microflora, we can talk about the pathology that has affected the woman: gardnerella (gardnerellosis), fungi (candidiasis), gonococci (gonorrhea), chlamydia (chlamydia), mycoplasma (mycoplasmosis), trichomonas (trichomoniasis). But most often, mixed microflora is detected, and the diagnosis sounds vague - vaginal dysbacteriosis.
If you look closely, you can see that all the above-mentioned bacterial pathologies can be transmitted sexually, and this speaks in favor of the fact that dysbacteriosis can be diagnosed not only in women, but also in men. Although it is worth mentioning here, because opportunistic microflora are the "native inhabitants" of any human body, so the decisive role in the development of the disease is still not the transmission of bacteria from person to person, which we just mentioned, but the immune status of the body. With strong immunity, infection does not actually occur, because the pathogens received from the sexual partner will be absorbed by phagocytes or will again become inactive.
The result of long-term research in this area was the theory that gardnerella itself is not a causative agent of any serious disease. Moreover, in most cases of diagnosed gardnerellosis, active trichomonads and chlamydia are found in smears. And the reason for the adhesion of the activated pathogenic microflora to the rejected epithelial cell is a sluggish infection called chlamydia, which a person might not even suspect.
The tests of a patient with acute chlamydial infection do not show a significant increase in leukocytes, the presence of trichomonads and other activated bacteria, only the beneficial microflora of the body and epithelial cells that are affected by chlamydia suffer. If the infection subsides and chlamydia die or reduce their activity, for example, when it becomes chronic, its place is taken by other bacteria: gardnerella, trichomonads, cocci, etc. (a holy place is never empty, because a decrease in the amount of beneficial microflora leads to a decrease in immunity and the active development of opportunistic and pathogenic organisms that have penetrated inside).
With chlamydial and some other infections affecting epithelial cells, their active destruction and detachment is observed. It is to these cells that the activated pathogens of dysbacteriosis and other pathologies attach. When taking a smear, the doctor removes mucus from the inner lining of the vagina, and gardnerella and other harmful microflora are found in this mucus. By detecting such modified epithelial cells under a microscope, the doctor speaks of the presence of "key cells in the smear."
Today, both theories exist in parallel. Some scientists are sure that gardnerellosis is not really a disease and does not require conventional treatment, focusing on the therapy of the cause of the activation of opportunistic and pathogenic microflora. In other words, it is necessary to increase immunity and treat chlamydia, and then, as needed, fight other activated microflora.
But most doctors consider gardnerellosis (let's remember that such a disease does not actually exist in the international classification of diseases) as an independent disease, in the treatment of which antibiotics come to the fore. That is, first we destroy all the microflora found in the vagina, and then we begin to restore the beneficial ones in order to prevent relapses of the disease.
Time will tell which theory's supporters are right, and who is following the line of least resistance and greatest profit. But in any case, the infection must be treated without hoping that it will subside on its own. If the immune system cannot cope with the excessively multiplied bacterial microflora, antibiotics are needed.
Reasons for the appearance of key cells in a smear
As we have already figured out, key cells in the smear do not appear by chance. This is facilitated by a decrease in vaginal acidity, which allows pathogenic bacteria that have entered the woman's body to successfully multiply. But for what reason can the balance of the internal microflora of the body be disturbed? When can we expect the appearance of key cells in the smear?
First of all, they talk about reduced immunity. Lactobacilli living in the small intestine and vagina actively participate in the synthesis of immunoglobulins, which in turn form immunity. A weakened immune system is not able to protect the body from the dominance of pathogenic bacteria and cannot slow down the growth of opportunistic microflora, which, excessively multiplying, causes no less harm.
Low immunity is not the only reason for the appearance of clue cells in a smear, but the effect of any of the below-mentioned reasons will be tied to the weakening of the body's defenses, i.e. to a decrease in immunity. Thus, clue cells can appear against the background of hormonal disruptions that occur during pregnancy, during puberty, and at the onset of menopause. Hormonal disruptions outside of these periods may be indicated by problems with conceiving a child, hair growth on a woman's body, and various menstrual cycle disorders.
Inflammatory processes, especially those that are chronic, play an important role in disrupting the body's microflora. Chronic inflammations always lead to weakening of the immune system, regardless of their location. And if these are also inflammations of the internal genital organs or pelvic organs, maintaining bacterial balance will be extremely difficult.
What else can lead to an imbalance of vaginal microflora in women? Excessive passion for intimate hygiene, which is no less dangerous than not observing it. If hygiene standards are not observed, there is a risk of introducing pathogenic bacteria and fungi into the body, but with a strong immune system, lactobacilli can cope with them on their own. But frequent use of such a therapeutic and hygienic procedure as douching contributes to the washing out of beneficial microflora along with pathogenic.
It takes time to restore the normal lactobacilli levels, during which the vaginal acidity will be disrupted and the ubiquitous opportunistic microflora will be able to multiply with impunity, causing various pathologies accompanied by itching, profuse vaginal discharge, and sometimes an unpleasant odor.
Some medical procedures can also be considered risk factors for the development of dysbacteriosis. Antiseptic and antibiotic therapy can have a negative effect on the body's microflora. But if antiseptics act more or less selectively and do not completely destroy the main composition of the bacterial microflora of the vagina (if we are not talking about douching), then antibiotic therapy can destroy it completely. Antibiotics do not care who is in front of them: the causative agent of the disease or the body's defender, it is important for them that this is a foreign substance related to bacteria.
Antibiotic therapy should be accompanied by taking medications that replenish the body's supply of beneficial lacto- and bifidobacteria, otherwise it is very difficult to avoid dysbacteriosis, especially with long-term treatment with antibiotics.
Taking antibiotics without a doctor's prescription is even more dangerous, because it contributes to the emergence of resistant strains of bacteria. When the need for antibiotic therapy actually arises, it may turn out that the prescribed antibiotic no longer copes with the causative agent of the disease, and an additional course of treatment with another drug (and sometimes more than one) will be prescribed. Lactobacilli are not able to produce protective components against antibiotics, and it turns out that the first drug will have a detrimental effect only on beneficial microflora, giving even greater freedom to pathogenic microbes. Antibacterial agents prescribed later will finally destroy the beneficial microflora and destroy the causative agent of the disease. But other dangerous bacteria, fungi and other harmful microorganisms can get into the fertile (insufficiently acidic) soil, which will lead to new problems associated with dysbacteriosis.
It is not only antibiotics and chronic inflammatory processes that cause weakening of the body's defenses. Regular excessive physical activity, acute inflammation of the genitourinary system, stress and depression, infectious systemic diseases, especially viral ones, poor nutrition (for example, limiting or refusing to eat dairy products), etc. can also play a role.
If we adhere to the second theory of vaginal dysbacteriosis development, then its cause should be considered a cured chlamydial infection, which as a result of incorrect treatment has turned into a sluggish form without pronounced symptoms. There is only one conclusion - chlamydia should be treated, even if the inflammation does not particularly bother you, and this should be approached seriously so that the bacteria are completely destroyed.
But let's get back to hormonal imbalance. It can be caused not only by internal but also by external reasons. For example, oral contraceptives contribute to changes in the hormonal balance, which is what their contraceptive effect is associated with. And barrier contraception itself quite often becomes the cause of vaginal infection or the development of an inflammatory process. If you also resort to the help of spermicidals, which have some bactericidal effect, on a daily basis, there is a risk of destroying the beneficial microflora in the vagina.
A separate conversation can be held about underwear. The passion for synthetics, which are easy to wash and wear well, does not contribute to the health of the internal microflora. By limiting the access of air to the body's tissues and creating the so-called greenhouse effect, they provide all the conditions for the reproduction of pathogenic bacteria and fungi, which are very pleased with warmth and moisture. It is not surprising that women who prefer underwear made of synthetic fabrics more often than others consult a doctor with complaints of itching and discharge from the genitals.
As for the methods of transmitting infections, the situation is as follows. A violation of the microflora in one of the partners leads to the proliferation of pathogenic microorganisms, which are easily transmitted to the other partner during sexual intercourse. If his immunity is weakened (and a rare person can boast of strong immunity), the newly arrived bacteria will quickly correct the situation, pulling the lot in their favor. Now the second partner also has dysbacteriosis or another infectious and inflammatory pathology of the reproductive system (chlamydia, candidiasis, gonorrhea, etc.). It must be said that promiscuous sexual relations only increase the risk of key cells appearing in a smear, which is not surprising when you do not know what kind of "disease" may be hidden in the depths of a little-known partner.
Symptoms of pathologies with key cells in a smear
It is believed that smears from the genitals of a healthy person should not contain clue cells at all. As soon as they appear, there is reason to suspect a violation of the vaginal microflora, when the balance shifts towards pathogenic and opportunistic microflora. Single clue cells in a smear may indicate that the disease has been caught at the very beginning and will be easy to defeat, sometimes just by normalizing the vaginal microflora. If there are many clue cells in the smears, this indicates an advanced form of the disease, indicating active reproduction of harmful bacteria, and here you can not do without antibiotics.
But as we already know, key cells in the biomaterial are not discovered by chance. This is not a blood test, which we take several times a year and not only for diagnostic, but even for preventive purposes. Taking a smear is justified in the case when a person comes to see a specialist with certain complaints.
True, gynecologists prefer to play it safe and take smears for microflora even during preventive examinations. This is due to the fact that in our lives there are many negative factors that can affect the health of the internal environment of the body. Unfavorable environmental conditions, stress, fatigue significantly undermine women's health and too often become the cause of vaginal dysbacteriosis. The sooner such a disorder is detected and treatment of the problem is started, the fewer negative consequences it will have.
Key cells in a smear in women are not at all uncommon in the practice of a female doctor, so diagnostics usually do not cause any particular difficulties when women come with habitual complaints. It is clear that depending on the type of bacterial microflora, the clinical picture of the disease may change somewhat, but still, such diseases have common features.
The first signs of most genitourinary diseases, in which there is a shift in the balance of vaginal microflora, are itching and burning in the genital area, discomfort during or after intercourse caused by irritation of the mucous membrane, the appearance of copious discharge with an unusual odor (normally, vaginal discharge has a sour odor). A change in the color of the discharge to yellowish and greenish indicates the active reproduction of a pathogenic bacterial infection. Such discharge is called purulent, and it rather indicates an advanced process.
Key cells in a smear during pregnancy are usually associated with gardnerellosis. Expectant mothers are usually selective in sexual relations, giving preference to one man, usually the father of the child. And if he, in turn, was just as careful in sexual terms and remained faithful to his wife, the likelihood of catching a serious bacterial infection remains extremely low. Another thing is that during pregnancy, a woman's body undergoes hormonal changes, which can negatively affect the state of the vaginal microflora.
And since not only lactobacilli and some types of beneficial microorganisms, but also gardnerella (in limited quantities and inactive state) are considered permanent residents of the mucous membrane of the genitals, hormonal imbalance can cause the activation of the latter, which will lead to vaginal dysbacteriosis with the appearance of itching and suspicious discharge. It is with these problems that expectant mothers rush to the doctor, who are jealous of their health and the future of their baby.
As for future fathers and other men, they can catch the infection through sexual contact with a woman who has bacterial vaginosis. And the more sexual contacts with different women, the higher the risk of infection.
Readers may have a fair question: where can key cells be found in men, since they do not have a vagina with its characteristic microflora? There is no vagina, but there is a penis with its well-known folds. And although it does not have its own epithelial cells, when it gets inside the vagina during intercourse, it can easily take key cells with it from there.
The head of the penis and under the foreskin covering it have their own microflora. Affected cells from the vagina mix with it, bacteria actively multiply and cause inflammatory processes in the tissues of the head, which doctors call bacterial balanoposthitis. In this case, taking a biomaterial sample will show single key cells in the smear, because the penis does not have its own epithelial cells on the surface.
Characteristic signs of the disease are: redness of the head of the penis, the appearance of pimples and whitish plaque on it, the occurrence of an unpleasant odor even after performing hygienic procedures. All this indicates the development of pathogenic microflora and the need for urgent treatment.
But again, as in the case of the female type of the disease, inflammation can also have internal causes. These include chronic inflammatory pathologies of the genitourinary system (cystitis, urethritis, prostatitis, etc.). For men, this is especially relevant, given the structural features of the urethra, which is also the penis. Internal bacterial infection reduces immunity and promotes the proliferation of opportunistic microflora (usually gardnerella, less often streptococci, staphylococci, etc.) not only in the urethra, but also beyond it.
If a man neglects intimate hygiene, bacteria multiply especially actively, hiding behind the foreskin and causing severe inflammation of the tissues of the head of the penis. Hygiene is no less important for a man than for a woman. If after intercourse with a woman who has been diagnosed with bacterial vaginosis, a man thoroughly washed his penis and all its folds, the probability of subsequently finding in him the key cells from the vagina that led to the development of balanoposthitis would be close to zero.
It is important to understand that dysbacteriosis is not an infectious disease transmitted sexually, although there is a possibility of such infection during sexual contact. But this probability is not as great as it seems. For the disease to develop, internal and external factors are needed that negatively affect a person's immunity. In other words, the disease affects only people with reduced immunity.
What cells can be found in a smear?
As we have already said, it is not in vain that gynecologists try to take a smear every time a woman comes to an appointment, even if it is a preventive examination. After all, the results of the smear can reveal pathologies that the woman does not even suspect. After all, the key cells in the smear, which are associated primarily with gardnerella, are considered only one of the indicators of a violation of the microflora. In fact, the pathogenic microflora of the vagina can be much richer, it is just that at the beginning of the disease, the symptoms of the pathology are absent.
Yes, 95% of the vaginal microflora are our helpers lactobacilli, and the remaining 5% should be other microflora, among which you can find various types of bacteria and viruses: round (cocci, among which Staphylococcus aureus comes to the fore) and rod-shaped (bacilli, including gardnerella), corynebacteria, aerobic and anaerobic microorganisms. In total, about 40 species, which should normally occupy from 2 to 5%, no more. If this percentage is higher, we are talking about an imbalance, i.e. lactobacilli can no longer restrain the growth of pathogenic microflora, and every day there will be more and more pests.
The key cells of gardnerella in a smear are modified flat epithelium with a granular structure. In principle, a small amount of flat epithelium is also found in the internal flora of a healthy woman. This is normal, because its absence may indicate a violation of the production of sex hormones. But cocci, which have a round shape, and rod-shaped gardnerella change the surface of the epithelium, and the doctor diagnoses key cells in the smear. The detection of cocci in a smear is already an alarming signal, which indicates the proliferation of harmful bacteria and a decrease in the number of lactobacilli.
Biomicroscopy and cytological analysis are based on the detection of pathogenic microorganisms. They are recognized by the structural features of the cells when examining the biomaterial under a microscope. If there is a suspicion of microflora that should not normally be in the vagina at all (for example, chlamydia, gonococci, etc.), other laboratory research methods may be prescribed (for example, PCR analysis, microflora culture, etc.), which allow identifying the pathogen and assessing the degree of development of the infectious process.
Any bacteria, even opportunistic ones, when they multiply excessively, cause irritation and inflammation of the vaginal tissues. Leukocytes, the main defenders that react sharply to infectious processes, have always been considered an indicator of the inflammatory process. If key cells are found in the smear and the leukocytes are increased, this indicates the development of an inflammatory process caused by gardnerella or other bacteria detected in large quantities during laboratory tests.
Normally, in the decoding of a smear from the vagina there should be no more than 10 leukocytes, in the biomaterial from the cervical canal - no more than 20. In inflammatory processes, this figure increases to 30 or more, which indicates the activation of the immune system to fight the infection. But a decrease in the number of lactobacilli weakens the immune system, which means that outside help will be needed to fight the infection.
A healthy person's immune system should work perfectly. Phagocytes are responsible for this - a special type of leukocytes capable of absorbing foreign cells. Neutrophils, macrophages, monocytes and some other cells have such properties. In principle, they should absorb any active pathogenic bacteria that enter the body, finding it with the help of special receptors. If phagocytes are normal, and key cells are found in large quantities in the smear, this indicates a violation of phagocytosis, i.e. malfunctions in the immune system.
The extent of the pathological process can be judged by the number of key cells, pathogenic microorganisms, and leukocytes. In bacterial vaginosis, although they talk about the presence of active gardnerella, in fact, we are most often talking about mixed microflora, the amount of which exceeds the required 5%.
But to accurately assess the vaginal colonization with bacteria, viruses and fungi, a smear must be taken and examined in accordance with certain requirements. Firstly, these are the requirements for patients to prepare for a gynecological examination, which the doctor should regularly remind overly clean patients about. Secondly, the requirements for conducting the analysis.
Proper preparation for a gynecological examination followed by taking a smear for microflora involves:
- refrain from using local hormonal agents, vaginal lubricants, spermicidal ointments several days before the examination (at least 3 days), since all of them can distort the real picture of the vaginal microflora,
- You should abstain from sexual intercourse for 1-2 days before visiting a gynecologist.
- the evening before the gynecological examination, a woman should perform an intimate hygiene procedure, but neither douching nor using various detergents is allowed; in the morning on the day of the appointment, hygiene procedures are undesirable,
- Many women in line to see a gynecologist try to empty their bladder to reduce discomfort during the examination. In fact, you need to go to the toilet no later than 2 hours before the appointment.
A smear for microflora is taken from the walls of the vagina, cervical canal of the uterus, urethra. It will be most informative in the first days after menstruation. And it will be better if the analysis is carried out within the first 3 hours after taking the smear.
Consequences and complications
Single epithelial cells, a small number of leukocytes, mucus and even yeast fungi found in a smear are not considered an alarming symptom. All of this can be present in the vaginal microflora in moderate quantities. A small number of cocci, restrained by the acidic environment created by lactobacilli, is also not a cause for concern.
However, the doctor may order a follow-up examination after a while to make sure that pathogenic bacteria have not started to multiply. Why is this so important? Because women's health depends on it. Bacteria, fungi, viruses and other parasites lead to the development of an inflammatory process on the mucous membrane of the internal genital organs of a woman.
Not only does the patient begin to experience constant itching in the genital area, irritations and wounds appear on the mucous membrane, but against this background, problems in sexual life also appear. The woman begins to avoid sexual intercourse, because during intercourse she experiences pain and discomfort. This provokes quarrels and scandals in the family, caused by dissatisfaction of both partners with sexual life.
Again, inflammatory processes do not go away on their own. Gradually, they spread to an ever larger area, capturing nearby internal organs. If nothing is done, the inflammation will become chronic. Against the background of inflammation, polyps can form on the vaginal mucosa, erosions appear. Over time, the uterine tissues themselves begin to grow uncontrollably at the site of severe inflammation (dysplasia) and there is a risk that, under the influence of predisposing factors, the cells will begin to mutate and turn malignant. It would seem to be a simple inflammation, but without treatment it can eventually develop into a terrible disease - cancer.
The problem of vaginal microflora disturbance can also cause another problem for young women - problems with conceiving a child, and the key cells in a smear during pregnancy are dangerous due to the risk of premature birth and miscarriage, infection of the child with a bacterial infection during passage through the birth canal, and various postpartum complications.
What else is dangerous about gardnerellosis for women? If the disease is not treated, there is a chance of getting inflammation of the ovaries and urethra, accompanied by pain in the lower abdomen, and in the latter case, in the genital area. In addition, women often begin to suffer from frequent urges to urinate.
Gardnerellosis in men is usually limited to inflammatory processes in the head of the penis and rarely causes other complications. However, in the presence of certain factors, there is a risk of developing pathologies such as urethritis, prostatitis, cystitis, vesiculitis, pyelonephritis, etc. against the background of activation of opportunistic microflora, if the multiplied bacteria continue to travel throughout the body.
If the smear shows only key cells and a small number of cocci, and the doctor diagnoses vaginal dysbacteriosis, this is not a reason to give up sexual activity. Bacterial vaginosis, as scary as it may sound, is not a contagious disease. The only requirement is strict hygiene of the penis after sex.
But the shift in the balance of vaginal microflora and the alkalization of its internal environment attracts not only opportunistic microflora. Over time, sexually transmitted pathogens may also be detected in the mixed flora (especially if there is more than one sexual partner). For them, an insufficiently acidic environment is also fertile ground for reproduction. It will take very little time for chlamydia, mycoplasmosis, gonorrhea, etc. to join vaginal dysbacteriosis, because the woman's immune system, weakened by a decrease in the number of lactobacilli, will no longer be able to resist the growth and reproduction of pathogens.
Now the patient will be a danger to her sexual partners. But STDs are a separate topic for discussion.
Can a man with an infectious and inflammatory non-venereal disease of the penis infect his partner? There is such a risk, because any, even opportunistic microorganisms that live on our skin and mucous membranes, can be dangerous if they begin to multiply rapidly. But they will begin to multiply if the woman's immune system is noticeably weakened by existing diseases. Thus, the probability that balanoposthitis or another infectious and inflammatory disease of the penis in a man can cause the development of bacterial vaginosis in women is relatively low (no more than 8%). However, this is not a reason for men not to treat their male diseases, because the risk still remains.
Prevention
The fact that the disease is not classified as serious does not mean that you should be careless about the possibility of acquiring it. Almost any disease is easier to prevent than to cure. Moreover, preventive measures usually do not require something impossible or extremely difficult from a person. In most cases, it all comes down to maintaining personal hygiene and a healthy lifestyle.
But what preventive measures will help to avoid such an unpleasant disease as bacterial vaginosis:
- Since we are talking about the genitals that come into contact with physiological secretions containing bacterial cells, the requirement of hygiene remains very relevant. Daily intimate hygiene using specialized products, if it does not become a guarantee of good health, will help prevent dangerous infectious diseases. It is believed that ordinary bath or baby soap, shower gels and creams are not suitable for cleansing procedures in intimate areas due to the inappropriate pH. But special products for intimate hygiene with the required acidity level can also cause harm if they are simply not suitable for a woman. So the choice of products for genital care must be taken responsibly.
- Intimate hygiene is important not only for women, but also for men, which is the main preventive factor for them. Daily water procedures with natural detergents plus genital hygiene after intercourse will help the stronger sex avoid unpleasant surprises. Additional protection against STIs will be the well-known latex product with the sonorous name "condom".
- Bacteria, viruses, fungi – these are microorganisms that are very attracted to the warm and moist internal environment of the vagina. There is no need to make it even more attractive with underwear made of synthetic materials that create a “greenhouse effect”. The same applies to panties that are too tight. Underwear should be loose enough and made of natural fabrics.
- Gynecologists also have a negative opinion about thongs. This model of underwear for women is considered a provoking factor for irritation of the tissues of the genitals and the introduction of an infection lurking in the anal area into the vagina.
- All women of childbearing age, who are most often found to have key cells in a smear, have such an unpleasant but very important phenomenon as menstruation. During this period, modern women use sanitary pads, which they buy in pharmacies and stores. But not all pads have a good effect on the state of women's microflora. A synthetic surface and a base made of air-impermeable material are not the best choice for a woman who cares about her sexual health. The material of the pads should be as natural, "breathable" and soft as possible. If the pads cause irritation of the tissues of the genitals, itching and other unpleasant sensations, it is better to refuse them. The same applies to hygienic tampons.
- Doctors also have an ambiguous attitude towards the so-called "daily pads". Gynecologists recommend wearing daily pads only on the first and last days of menstruation, while there is scanty dark discharge. They will also be useful for those women who, due to pathological reasons, have abundant light discharge that heavily stains underwear and creates a feeling of dampness. But even in this case, it is not recommended to use pads constantly. It is better to change panties more often. The fact is that "daily pads" have a dense base that does not allow air to pass through well, which does not allow the body to "breathe", but promotes the proliferation of anaerobic bacteria.
- Now, regarding sexual life. For a woman, a source of bacterial infection can be a man who is a carrier of this very infection. Frequent change of partners is fraught not only with the risk of developing vaginal dysbacteriosis, but also with infection with venereal diseases. So it is better to look for different ways to get sexual satisfaction with one partner than on the side with unverified men. By the way, this point is also relevant for representatives of the stronger sex.
- If a couple practices anal sex and alternates it with vaginal sex, the woman should be prepared for the fact that at some point the gynecologist will find "foreigners" in her vagina. The anus and rectum contain such a rich composition of various microflora, unsuitable for a woman's vagina, that dysbacteriosis will not be something unexpected.
But all of the above will not help a woman protect herself from infection as well as the well-coordinated work of the immune system. And for it to be so, it is necessary:
- Reconsider your attitude to nutrition. It should be regular and complete. Products should be natural and, if possible, without harmful additives. Preference should be given to vegetables and fruits containing a rich complex of vitamins and minerals that will help strengthen the immune system. Lemon, honey, ginger, chicory, apples, garlic, almonds and other natural products are considered useful for the immune system.
Strengthening the immune system and maintaining normal microflora in the body, and the vagina in particular, is facilitated by dairy and fermented milk products, which must be present in a woman’s diet.
- Hardening is a well-known health procedure that helps strengthen the immune system. The main thing is to do it correctly, because the female reproductive system is very sensitive to hypothermia, so reducing the water temperature and increasing the duration of walks in the cold air should be done gradually.
- It is clear that such bad habits as drinking alcohol and smoking do not have the best effect on the body's protective functions. But giving up such unnecessary habits in favor of a healthy and active lifestyle only helps strengthen the immune system.
- Stress and overwork are the things that have the worst effect on human health. You need to learn to cope with stressful situations, use relaxation practices, and regulate physical and mental stress. This will help the body not to waste its energy in vain, but to use it to fight uninvited guests.
- What else will help maintain microflora and strong immunity?
- Timely treatment of infectious diseases of various etiologies and localizations.
- Regular preventive examinations with a therapist and gynecologist. Women of reproductive age are recommended to visit their "favorite" doctor once every six months.
- A sensible approach to antibiotic treatment. They should only be taken if the doctor sees the need for it. Prescribing strong drugs to yourself is a risk of worsening the situation and adding a couple of new diseases to the list of existing ones. Taking antibiotics should always be combined with restoring the microflora with probiotics.
It would seem that there is nothing complicated in preventing microflora disturbance in your body. However, key cells in a smear are found daily in women of different ages and statuses. And the reason for this is the careless attitude of women to a popular disease that is not considered dangerous, but can still bring quite a lot of trouble. Probably, girls should be taught to monitor their female health and value it from early childhood. And then we can hope that the situation will change for the better over time.
Forecast
Vaginal dysbacteriosis is a fairly common disease, which, however, is not considered life-threatening. If the process is not neglected, the treatment of the disease does not present any particular difficulties. The prognosis of the disease with a serious approach to its treatment is always favorable. Complications can be expected if no treatment measures are taken, as well as in the case of antibiotic treatment without restoring the destroyed beneficial microflora with the help of special probiotic preparations.


 [
[