Medical expert of the article
New publications
Bacteria in urine: what does it mean?
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Various pathologies of internal organs, especially kidneys and urinary tract, are accompanied by the fact that bacteria in the urine of women and men begin to multiply intensively. As a result, the bacteriological analysis of urine becomes positive, which is considered a negative sign, since urine should normally remain a sterile biological fluid.
Normal levels of bacteria in urine in women and men
Women should not normally have any bacteria in their urine, as urine is a sterile biological fluid that does not contain microflora. The presence of microorganisms indicates the development of an infectious and inflammatory process and requires mandatory treatment. Some studies show that urine contains communities of living bacteria that make up the resident microbiota of female urine. [ 1 ]
Men should not normally have bacteria in their urine, as urine is a sterile environment and should not contain microflora. The presence of bacteria indicates the development of a bacterial infection, a high risk of developing bacteremia and sepsis. [ 2 ]
Epidemiology
Asymptomatic bacteriuria is the presence of bacteria in a properly collected urine sample from a patient who has no signs or symptoms of a urinary tract infection. Asymptomatic bacteriuria is very common in clinical practice, and its incidence increases with age. The incidence is 15 percent or more in women and men aged 65 to 80 years, and reaches 40 to 50 percent after age 80. Most patients with asymptomatic bacteriuria will never develop symptomatic urinary tract infections, and asymptomatic bacteriuria will have no adverse effects.[ 3 ],[ 4 ]
Causes bacteria in the urine
There is quite a wide variety of reasons that can lead to the development of bacteria in the urine. But all these reasons can be divided into two large groups: autoinfection and infection from external sources. Thus, autoinfection implies that there is a source of infection in the body, a certain inflammatory and infectious process develops.
The primary source of infection can be localized anywhere: lungs, gastrointestinal tract, bronchi, liver. Gradually, the infection can spread throughout the body, forming secondary sources of infection. From there, the infection gets into the kidneys, urinary tract, ureters, and, accordingly, can cause inflammation in them. In this case, a urine test shows the presence of bacteria in the urine. In this case, it is appropriate to talk about the descending path of infection, in which the infection goes down from the kidneys to the urinary tract and external genitalia. [ 5 ]
As for the external source of infection, this means that the infection enters the body from the outside. The main route of infection is considered to be the ascending route, in which the infection rises from the external genitalia, colonizing the mucous membranes, urinary tract, ureters, and finally penetrates the kidneys, where the main source of infection subsequently develops. [ 6 ]
Most often, it is a chronic infection of the urinary tract, kidneys, and reproductive system. Less often, it is a hidden genitourinary infection or a sexually transmitted disease. Sometimes the lesion is not connected with the genitourinary system and is located, for example, in the oral cavity (old caries, or in the area of the tonsils, inflamed lymph nodes, or adenoids). Sometimes, dysbacteriosis and disruption of the normal microflora of the stomach, intestines, and rectum lead to the development of an infection lesion and the entry of bacteria into the urine. In rare cases, the infection enters the body from the kidneys, liver, or other organs during a severe general infectious process, for example, if a person has chickenpox, measles, plague, malaria, and other severe diseases.
It is important to understand that the primary source of infection can be anywhere: it can be the lungs, bronchi, gastrointestinal tract, liver, and even human skin. Gradually, the infection can spread throughout the body, forming secondary sources of infection. It is from them that the infection enters the urinary tract, which is detected during a urine test (a urine test for sterility shows the presence of bacteria in the urine).
If we are talking about an external source of infection, then in this case we should mean that the infection enters the body from the external, environmental environment. There are various ways of infection, and most often it is sexual contact, or swimming pools, dirty laundry, failure to observe hygiene rules. In women, the cause of infection is often the use of tampons, since they can serve as a source of infection, especially in hot weather or at night. In this case, we are talking about the ascending path of infection, in which the infection rises from the external genitalia, directly to the genitourinary system, where the main source of infection subsequently develops.
Cystitis
Cystitis is an inflammatory process in the genitourinary tract, which manifests a whole range of symptoms. One of the main symptoms is pain and stinging in the area of the external genitals, pain during urination, burning, frequent urge to urinate, and the presence of false urges. The frequency of urination increases, especially at night. Cystitis is often accompanied by severe attacks of stinging, pain that affect the entire lower abdomen and urinary system.
An inflammatory process develops, which is accompanied by an infection, the appearance of bacteria in the urine. It is also worth noting the presence of edema, strong foci of inflammation, infiltrates, and a purulent-septic process. A complication of cystitis develops quite quickly, which is an inflammatory process affecting the kidneys. As a rule, cystitis is accompanied by severe pain, attacks, intoxication, and an increase in temperature. At the same time, the inflammatory process spreads to other organs quite quickly. It is worth noting that many people diagnosed with cystitis require urgent hospitalization. The therapy is based on stopping the inflammatory process, relieving pain and eliminating the infection.
Bacteria in urine in diabetes
Diabetes mellitus is a complex somatic disease, the leading link in the pathogenesis of which is a violation of metabolic processes and basic biochemical parameters in the body. In this case, first of all, carbohydrate metabolism in the body is disrupted, the level of glucose in the blood, as the end product of carbohydrate breakdown, changes sharply. Disruption of metabolic processes entails a whole range of pathological reactions, ranging from disruption of the normal state of the mucous membranes, decreased immunity, disruption of hormonal levels, and ending with a violation of the colonization resistance of the mucous membranes, their natural protective properties, and the system of non-specific resistance. As a result, dysbiosis, or dysbacteriosis, develops, uncontrolled development of a bacterial infection may begin, activation of viruses persistent in the blood. As a result, bacteria are found in the urine with diabetes. Treatment, as a rule, is complex and depends on the person's status for the underlying disease (diabetes). It is impossible to cure a bacterial infection without taking into account the specifics of the body's condition with diabetes. Therefore, a mandatory consultation with an endocrinologist is required.
Bacteria in urine after antibiotics
As a rule, after taking antibiotics, dysbacteriosis is detected, since antibiotics do not have a selective effect exclusively on pathogenic microflora. By killing representatives of pathogenic microflora, pathogens of infectious diseases, antibiotics also kill normal microflora, which leads to the development of dysbacteriosis. As a result of taking antibiotics, the risk of developing a fungal infection increases significantly, since nothing is found in the place where normal microflora should normally be. Accordingly, this place is colonized by other microorganisms. It is the fungal microflora that has the highest growth rate, which in such cases colonizes free niches. Therefore, people with reduced immunity are recommended to take antifungal drugs in combination with antibiotics to prevent fungal infections.
There is also another nuance that you need to know and take into account - after antibiotics, you cannot take a sterility test or a bacteriological culture, since the results will not be reliable. The result will most likely be false negative, since both pathogenic and normal microflora will be killed. It takes an average of 10-14 days for the microflora to recover in a certain way, after which you can judge its condition, draw conclusions about the effectiveness of antibiotic therapy. Otherwise, if you need to get quantitative and qualitative characteristics of the microflora, you need to take tests before starting antibiotic therapy.
Risk factors
The risk group includes people who have recently suffered from acute infectious diseases, as well as people with a history of chronic diseases. People with acute and chronic kidney diseases, urinary tract diseases, people who have recently undergone antibiotic therapy, chemotherapy are at significant risk, since they experience a sharp decrease in immunity, which entails various violations of the microbiocenosis.
It is worth noting that risk factors also include hormonal imbalance, decreased immunity, immune tension, high viral load, latent infections or persistent infection in the blood, since all of this directly or indirectly affects the condition of the mucous membranes. The factors listed above cause a decrease in colonization resistance, a violation of the normocenosis, and, accordingly, an increase in the proportion of pathogenic and opportunistic microorganisms, which contributes to the development of inflammatory and infectious processes, the appearance of bacteria in the urine. [ 7 ]
Alcohol
Alcohol in general significantly changes the results of laboratory tests. About 2-3 days before the test, you should refrain from drinking alcohol. Also, you should not take tests immediately after a party where you drank alcohol. You should wait 2-3 days. Not only the main biochemical indicators change, but also the level of bacteria. This is due to the fact that ethyl alcohol contained in alcoholic beverages has an inhibitory effect on microorganisms. Accordingly, you can get underestimated or false negative results of laboratory tests.
Pathogenesis
Normally, urine is a sterile biological fluid that does not contain microorganisms. Bacteria penetrate into urine if there is an infection in the body, as well as a focus of an infectious or inflammatory process. In this case, there are three possible scenarios. There are cases when bacteria are not viable and accidentally got into the urine from the external genitalia, for example, with thrush or other infections of the genitourinary tract. This is the so-called "transient microflora", that is, those microorganisms that accidentally ended up in the urine. There should be few of them - a few units in the field of vision. It is worth thinking about an infection of the external genitalia, undergo appropriate treatment, consult a doctor. This also indicates that the analysis was collected incorrectly. It is necessary to more carefully observe hygiene and toilet of the external genitalia before taking the test.
The second option indicates bacteremia. In this case, single colonies of microorganisms are found in the urine. This indicates the development of a fairly strong inflammatory-infectious process in the kidneys, urinary system, and reproductive organs. It is necessary to undergo treatment as soon as possible. Hospitalization may be required, since in this case we are talking about a significant excess of all possible indicators of the norm, as well as the progression of the infectious process, the formation of new foci of infection. The risk of sepsis is high.
The third option is when not single but multiple colonies of microorganisms of various sizes and shapes are found in the urine. In this case, we are talking about sepsis - infection of biological sterile fluids. Emergency hospitalization and emergency care are required. There is a severe infectious process, with a tendency to a purulent-necrotic pathological process, progression and uncontrolled spread of infection, infection of biological sterile fluids, including blood. If appropriate measures are not taken, a fatal outcome may occur.
Symptoms bacteria in the urine
The pathology can develop both with symptoms and asymptomatically. In the first case, a person usually has all the signs of inflammatory processes in the kidneys and genitourinary organs, in particular, in the ureters, urinary tract, bladder, and kidneys themselves. [ 8 ]
There may be a violation of the urination process, frequent or false urge to urinate, pain both during urination and at other times. Often there is pain in the lower back, during movements, pain in the kidney area. As for the asymptomatic course of the pathology, a person does not feel any discomfort or problems, only when taking a test, the presence of an infection in the urine is accidentally detected. This is also quite common and requires a comprehensive examination, since it can be a sign of a serious pathology that is hidden. [ 9 ]
Mucus and bacteria in urine in women and men
Mucus indicates the presence of an inflammatory process. The presence of bacteria in the urine indicates the development of a urinary tract infection. In women, the infection develops much faster than in men, so special attention should be paid to this. The severity of the pathological process depends on the quantitative indicators of microorganisms. In any case, a mandatory consultation with a doctor is required, since it is necessary to accurately determine the source of the infection. These can be infectious and inflammatory processes in the kidneys - nephritis, pyelonephritis, glomerulonephritis, and other kidney pathologies. These can also be extrarenal pathologies, for example, cystitis, gynecological diseases. Treatment depends on which microflora predominates, as well as on the source of the infection and its quantitative indicators. Additional tests will be required, in particular, a bacteriological study of urine, urinary sediment. [ 10 ]
Mucus is the main sign of an inflammatory process, the presence of bacteria indicates an infectious nature of the inflammation. In men, this may be a sign of kidney disease or extrarenal apparatus. It may develop against the background of inflammatory and infectious diseases: nephritis, pyelonephritis, cystitis, urethritis. Less often, it may indicate prostatitis, adenoma, and other pathologies of the male reproductive system. The risk of developing sepsis and bacteremia is quite high, so mandatory treatment is required. The sooner it is started, the more effective and faster the result will be.
Lots of bacteria in urine in women and men
Laboratory and clinical diagnostics is a fairly precise science that does not tolerate such conditional concepts as "many". Of course, the more bacteria are found in a woman's urine, the more severe the pathological process. It is necessary to know the exact quantitative indicator that allows us to judge the severity of the pathological process. Normally, there should be no bacteria in the urine, so any appearance of them indicates pathology.
Speaking very conditionally, we can say that “few” bacteria are an indicator of 101-105 CFU/ml. Accordingly, any indicators over 105 CFU/ml can be considered as “many” bacteria in the urine. Regardless of how many bacteria are found in a woman’s urine, treatment is mandatory, since self-healing, unfortunately, does not occur. The disease can only progress, and the number of microorganisms without appropriate therapy will only grow.
In bacteriology and laboratory science, there are no such concepts as “many” and “few”. It is necessary to know the exact number of bacteria found in a man’s urine in order to be able to judge the severity of the pathological process. Any appearance of bacteria in the urine indicates a deviation from the norm. The higher the quantitative indicators, the more severe the pathological process. Conventionally, the concept of “many” can include indicators over 105 CFU/ml, which is quite dangerous and requires immediate treatment. [ 11 ]
Leukocytes and bacteria in urine
The presence of leukocytes and bacteria in the urine almost certainly indicates the presence of an inflammatory process. The presence of bacteria in the urine is a sign of the development of an infectious process in the urinary organs. The severity of the pathological process depends on how many microorganisms are detected in quantitative terms. These can be various infectious and inflammatory processes, but most often - pathological processes in the kidneys - nephritis, pyelonephritis, glomerulonephritis, and other pathological conditions.
Normally, there should be no bacteria in urine, since it is a biologically sterile liquid. The appearance of bacteria accompanies the inflammatory process, since aseptic inflammation, which would develop without the presence of a bacterial (infectious) process, is practically not encountered.
Leukocytes in urine without bacteria
Leukocytes without bacteria may be found in urine. This phenomenon is most often observed in women, and it develops in most cases in connection with gynecological diseases. Sometimes the presence of leukocytes in urine indicates the development of cystitis. A similar phenomenon occurs in pregnant women. Most often, this is a sign of increased stress on the kidneys. Or a similar condition is observed in pregnancy pathology, so a mandatory consultation with the attending physician is required, and prenatal hospitalization may be required.
A comprehensive diagnosis is carried out, based on the results of which the appropriate treatment is usually prescribed. The specifics of treatment depend on the predominant microflora, as well as the source of infection. To select the optimal dosage of the drug, it is necessary to know the quantitative indicators of the microflora. Therefore, in most cases, additional tests are required. The most informative methods are such methods as bacteriological examination of urine, microscopy of urinary sediment. The first method allows you to exclude a bacterial infection, the second method clarifies and expands the clinical picture of the pathology.
Mucus and bacteria in urine
Mucus in urine together with bacteria is the main sign of an inflammatory process. Mucus indicates a small formation of exudate, increased work of the mucous membranes, which, as a rule, provide immune protection of the body. The presence of bacteria indicates the development of inflammation of infectious genesis. This may be a sign of diseases of the kidneys, urinary tract, ureter, bladder, or extrarenal apparatus. That is, only on the basis of the detection of mucus and bacteria in the urine it is impossible to make an accurate conclusion about the causes, it is impossible to make a diagnosis. Therefore, differential diagnostics is required, which will allow differentiating the signs of various, clinically similar manifestations of various diseases. Knowing the exact diagnosis and the exact cause of the pathology, we can talk about the selection of adequate treatment.
Protein and bacteria in urine
The presence of bacteria, and especially protein in the urine, is always an unfavorable sign. Bacteria accompany infectious and inflammatory processes. It can develop against the background of inflammatory and infectious diseases: nephritis, pyelonephritis, glomerulonephritis, cystitis, urethritis.
Protein can also be a sign of these processes. The presence of bacteria and protein can indicate the development of a tumor, both malignant and benign.
The presence of protein is often found in patients with atherosclerosis, diabetes, and may indicate excessive strain on the kidneys. Protein in the urine always indicates that the kidneys cannot cope with the filtration function. This can be observed in severe infectious processes in the body, for example, plague, anthrax, malaria, measles, mumps, rubella. Currently, vaccinations are given against these diseases. During pregnancy, the presence of protein is an unfavorable sign that can indicate a number of pathologies. Starting from a violation of the pregnant woman's diet, consumption of large amounts of carbohydrates, proteins with food. And ending with serious renal pathologies that can lead to severe edema, gestosis, pregnancy pathologies, can cause complications during childbirth, and even lead to renal failure.
A similar picture is observed in cases of poisoning, chronic intoxication, and during treatment with certain pharmaceuticals that have an adverse effect on the kidneys. This may be a complication after intensive antibiotic therapy, chemotherapy, radiation therapy, or during tumor irradiation. In oncological processes, this is also an unfavorable sign that may indicate the disintegration of a tumor, tissue, severe intoxication, kidney failure, or kidney metastases. The appearance of protein in the urine may be observed in the postoperative period, after transplantation, in the failure of one kidney, in renal cirrhosis, or in renal failure. This may be a sign of the development of congestion in seriously ill, bedridden patients, and indicates increased edema and fluid retention in the body. Protein is often found in the urine of newborns, which indicates functional immaturity of the kidneys and increased stress on them. In elderly people, as well as in people with immunodeficiencies and autoimmune aggression, protein and bacteria may appear in the urine.
If left untreated, there is a fairly high risk of developing sepsis and bacteremia, as well as kidney failure due to renal insufficiency. Therefore, mandatory treatment is required, often even hospitalization in a specialized department. The sooner it is started, the more effective and faster the result will be.
Red blood cells and bacteria in urine
The presence of red blood cells in urine primarily indicates bleeding or rupture of blood vessels, decreased tone and permeability of small capillaries. Sometimes the presence of red blood cells is a sign of anemia. In general, if we assume that red blood cells are blood cells, it is easy to conclude that any ingress of red blood cells into urine is associated with the ingress of blood into urine, or with the development of bleeding, vascular bleeding. It is worth noting that a similar picture can be detected in the development of ulcers, erosions, tumor processes.
In women, it is important to clearly differentiate the source of blood. It is necessary to exclude accidental blood in the urine, since the anatomical proximity of the reproductive organs and the urinary system can contribute to accidental blood in uterine and ectopic bleeding, gynecological diseases, miscarriages, aortas, surgical and microinvasive interventions in the pelvic area. Also, the penetration of erythrocytes is possible during menstruation.
Bacteria, fungi in urine
Bacteria and fungi found in urine indicate severe dysbacteriosis and even dysbiosis in the body. This is often observed after intensive antibiotic therapy, after chemotherapy, radiation therapy, during the treatment of severe infectious diseases, including tuberculosis, cholera, dysentery. The appearance of fungus is possible only if a person has a disrupted normal microflora in the body, that is, all representatives of the normal microflora are killed. Then the pathogenic microflora, primarily fungal microflora, begins to grow rapidly, colonizes the urinary tract and other systems. Bacteria are found mainly pathogenic. This is due to the fact that with a normal state of microflora, it has colonization resistance, that is, it prevents the growth of pathogenic bacteria and fungi. It is also worth noting that such a condition can develop only under the condition of reduced immunity. Therefore, in this case, it is advisable to restore the normal microflora, which will allow the body to independently resist the infection in the future. In case of severe colonization, antibiotic therapy and antifungal therapy (in combination) are first administered, then measures aimed at restoring microflora (probiotics, prebiotics) are applied. Also, in parallel, a consultation with an immunologist is required, who will prescribe the appropriate immunomodulatory therapy.
Salts in urine bacteria
The presence of any salts in the urine indicates the development of an inflammatory and infectious process in the kidneys or urinary organs. It can also be a sign of congestion, insufficient filtration capacity of the kidneys, which can be both congenital and acquired pathology. In women, this can also be a sign of gynecological diseases. In men, salts can indirectly indicate the presence of prostatitis, prostate adenoma, and other similar phenomena. Salts are formed when the digestive function is impaired, including against the background of gallstone disease, pancreatitis. Sometimes this can be a sign of the development of neoplasms in the urinary or reproductive system: it indicates the development of both benign and malignant tumors. It can be a sign of improper nutrition, in which the diet contains an excess of salts, minerals, heavy metals, minerals.
Bacteria and epithelium in urine
Normally, there should be no epithelium or bacteria in the urine. Conditionally acceptable is the presence of 0-3 single epithelial cells in the urine in the field of view of the drug. But such a condition is already considered borderline and is the basis for taking note of such a patient, monitoring the patient's condition in dynamics, since he falls into the risk group for the development of inflammatory processes. It is also worth noting that bacteria in the urine should not be under any circumstances. Their appearance in the urine indicates the development of an inflammatory, infectious process. In order to confirm or refute the presence of epithelium and bacteria in the urine, you need to retake the test. Repeated detection is a tendency and is considered the basis for classifying the patient as a risk group, ensuring control over his condition.
Epithelium in urine can be detected in the presence of acute and chronic kidney damage in the body. These can be acute and chronic nephritis, pyelonephritis, amyloidosis. Epithelium can be detected in feverish conditions, infectious diseases, intoxication, increased load on the kidneys.
The type of epithelium found in the preparation can also tell a lot. Thus, the presence of flat cells can be a sign of urethritis, prostatitis, and is observed mainly in inflammatory processes in men. Transitional epithelial cells appear in cystitis, pyelitis, and neoplasms of the urinary tract. These are cells that normally line the mucous membranes of the urogenital tract and appear in the urine when they are damaged, or inflammatory processes develop. The appearance of renal epithelial cells indicates kidney pathology.
Oxalates and bacteria in urine
Bacteria in urine develop during an inflammatory process and are also a sign of bacteremia or sepsis. Oxalates are calcium oxalate salts and are observed after a person has consumed foods containing oxalic acid. As a rule, oxalates and bacteria in urine are found after recent inflammatory processes that develop with increased load on the kidneys. They can also appear after eating sorrel, spinach, asparagus, beets, tomatoes, apples, oranges, citrus fruits, cucumbers, grapes. These products are difficult for the kidneys to process, especially in a person with kidney pathology. Therefore, it is so important to adhere to a balanced diet. If oxalates form in the urine some time after urination, this may indicate that the person eats exclusively meat, or it predominates in his diet. It can also be a sign of diabetes, calcium metabolism disorder, and is found in severe chronic renal pathologies. It is worth noting that the persistent multiple appearance of oxalates and bacteria in the urine is the basis for the diagnosis of oxaluria.
Nitrites, leukocytes and bacteria in urine
The combined detection of nitrites, leukocytes and bacteria in urine indicates the development of an inflammatory process in the kidneys or urinary organs. Such pathology can be equally often detected in both men and women. In women, this can also be a sign of gynecological diseases. In men, it is a sign of adenoma, prostate carcinoma or prostatitis.
The presence of nitrites in urine indicates the development of an inflammatory and infectious process in the kidneys. At the same time, the presence of nitrites directly correlates with the presence of gram-negative microflora, which actively uses nitrites in its metabolism.
The presence of nitrites and leukocytes may be a sign of the development of neoplasms in the urinary or reproductive system, since nitrites can also form during the decay of a tumor. The presence of nitrites indicates the development of both benign and malignant tumors. Nitrites are products of the breakdown of nitrates. Therefore, the appearance of nitrites in urine can also be caused by eating foods containing nitrates.
Thus, we can conclude that bacteria in urine is always an unfavorable sign indicating pathology, since urine should normally be sterile.
Nitrites and bacteria in urine in women and men
Indicates the development of an inflammatory process in the kidneys or urinary organs. In women, this may also be a sign of gynecological diseases. Nitrites also indicate the development of an inflammatory and infectious process in the kidneys, and most often indicate the presence of gram-negative microflora. Sometimes this may be a sign of the development of neoplasms in the urinary or reproductive system: indicates the development of both benign and malignant tumors.
Nitrites and bacteria are closely related. Thus, nitrites found in a man's urine are products of nitrate breakdown. In the presence of dysbacteriosis with a predominance of gram-negative microflora, nitrates, under the influence of specific enzymes of these bacteria, are not excreted, but enter the urine in a modified form (in the form of nitrites). But there are a number of other factors that can lead to such a phenomenon. Therefore, a consultation with a competent specialist is required.
Complications and consequences
The most dangerous consequences of the appearance of bacteria in urine are the progression of the infectious process, the spread and increase in the amount of infection, its penetration into the kidneys and other organs, the formation of new (secondary) foci of infection. The most dangerous complications should be considered bacteremia and sepsis, which can end in death. [ 12 ]
Diagnostics bacteria in the urine
Diagnostics consists of accurately identifying the qualitative and quantitative characteristics of the detected bacteria. That is, it is necessary to determine which microorganisms are present in the urine (their genus and generic affiliation), and also to determine their quantity. Additionally, an antibiotic sensitivity test can be performed. That is, it is possible to select a drug that will be effective in treating a bacterial infection. Laboratory methods are used for this. Instrumental methods may also be required that will allow you to track the characteristics of pathological changes in the body, identify the source of inflammation and infection. [ 13 ]
Tests
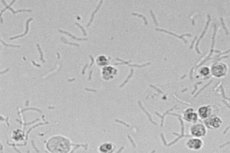
The main analysis is a bacteriological urine culture. The most commonly used culture method is Gould's (but it all depends on the equipment and capabilities of the laboratory where the analysis is performed). After the culture has been produced on the medium, the Petri dish is placed in a thermostat under optimal conditions, the culture is incubated for 3 to 5 days, then transferred to selective nutrient media and a pure culture is isolated. The pure culture is identified in accordance with Bergey's identifier.
Based on the growth characteristics on a selective medium, the growth rate and other significant parameters are determined, and biochemical and serological tests are carried out, which ultimately make it possible to determine the exact quantitative and qualitative characteristics of the identified microorganism.
Quite often, an additional analysis of the antibiotic sensitivity of the isolated microorganism is carried out. For this, the disk diffusion method or the serial dilution method is used. The essence is that the antibiotic that is most effective against the identified microorganism is determined, and its optimal concentration is also determined, which will allow getting rid of the infection.
Conventional clinical studies of blood, urine and feces are also prescribed according to the protocol. They can be quite informative and can be a source of valuable information, allowing to consider a more extensive picture of the pathology, to determine the features of the course of the pathological process and its localization. But the main method that allows to make a final diagnosis is sowing.
Additional tests that are prescribed according to indications may include an immunogram, virological studies, rheumatic tests. Tests for interferon levels, immunoglobulins, and sometimes allergy tests. Microbiological screening and dysbacteriosis testing may also be required.
Instrumental diagnostics
The main diagnostic method is laboratory diagnostics (bacteriological examination). Instrumental methods are used as additional, clarifying methods. For example, rheography may be required, which allows examining the functional state of the kidneys, urodynamics. Ultrasound, X-ray examination of the urinary tract, abdominal organs and pelvis are prescribed if necessary. Computer or magnetic resonance imaging may be required. In case of combined pathology of the digestive tract, gastroscopy, colonoscopy, irrigoscopy, gastroduodenoscopy, endoscopy, and other methods are used.
Differential diagnosis
With the help of differential diagnostics, it is possible to differentiate the signs of one disease from the signs of another disease. For example, it is important to differentiate kidney diseases from cystitis, since both pathologies are accompanied by the presence of bacteria in the urine, but the treatment is fundamentally different. It is also important to differentiate the bacteria that are found in the urine. For this, a bacteriological study is carried out, which allows you to clearly isolate and identify the type of bacteria and determine their quantity.
Other diseases with which bacteria in urine must be differentiated:
- Acute pyelonephritis.
- Bladder cancer.
- Chlamydia (chlamydial urogenital infections).
- Cystitis (non-bacterial).
- Herpes simplex.
- Interstitial cystitis.
- Inflammatory diseases of the pelvic organs.
- Renal and perirenal abscess.
- Urethritis.
- Vaginitis.
Who to contact?
Treatment bacteria in the urine
Bacteria in urine, both in men and women, can only be eliminated using antibiotic therapy. What exactly to treat - the doctor will tell you. The choice of one or another antibiotic depends on a number of factors, including the type of bacteria found in the urine and their quantity. Also, in many ways, therapy is determined by the individual characteristics of the body, the state of its immune system, local and systemic immunity.
Treatment should be guided by urine culture and susceptibility results. Amoxicillin, amoxicillin/clavulanate, cefuroxime, cephalexin, and nitrofurantoin are considered safe for use during pregnancy.[ 14 ],[ 15 ] Duration of treatment should be 3 to 7 days, and at least one urine culture should be performed.
The most universal antibiotics that are prescribed for the treatment of many infections, including combined infections, are broad-spectrum antibiotics. They can have both bacteriostatic and bactericidal effects, that is, antibiotics can either partially suppress the growth of microorganisms or kill them completely. There are also special uroseptics that are used to treat infectious diseases of the urogenital tract. They have a targeted effect on those pathogens that contribute to the development of diseases of the urinary system.
When using some medications, additional drugs may be required, for example, probiotics, aimed at normalizing normal microflora. This is due to the fact that antibiotics, along with pathogenic microflora, can simultaneously kill representatives of normal microflora. Their deficiency must be replenished, otherwise a fungal infection will occur.
Hepatoprotectors may also be required, since some antibiotics can have a toxic effect on the liver. Complex therapy is often represented by both antifungal agents and antibiotics. Sometimes immunomodulators are additionally included in the treatment regimen. But such prescriptions should be made strictly by a doctor, since self-medication can be fraught with serious consequences, including immune disorders.
Medicines
Medicines should be prescribed only by a doctor, based on the results of studies. This is the main precaution. This is due to the fact that otherwise numerous side effects may develop. It is necessary to strictly follow the treatment regimen. The main side effects are the development of dysbacteriosis, disorders of the immune system, disruption of the normal state of the mucous membranes, and the development of a fungal infection.
To eliminate bacteria (treat bacterial infections), antibiotic therapy is used.
A broad-spectrum antibiotic, amoxiclav, has proven itself well. It belongs to the penicillin series of antibiotics. It is active against both gram-positive and gram-negative microorganisms. One tablet is taken per day (500 mg of the active substance). The course of treatment is designed for three days. There are three tablets in the package.
More powerful is ciprofloxacin, which is a macrolide. It is also taken at 500 mg (one tablet) per day. Usually, the course of treatment ranges from 3 to 5 days, depending on the severity of the bacterial infection and the number of microorganisms detected in the urine. You can divide the daily dosage into 2 parts - take half a tablet (250 mg) twice a day.
Azitrox (azithromycin) is also prescribed at 500 mg per day for three days.
Among uroseptics, Urolesan has proven itself well, which is prescribed on average 10-25 drops, depending on the age and body weight of the patient. It is recommended to wash it down with a small amount of water, or drip it onto a small piece of sugar and eat it with sugar. This enhances its effect. [ 16 ], [ 17 ]
Vitamins
It is not recommended to take vitamins for bacterial infections, as they act as growth factors for microorganisms, as a result of which their growth and reproduction increases, and the bacterial process becomes more severe. Vitamin C is an exception. On the contrary, it suppresses the growth of pathogenic microflora, stimulates the immune system, human defense mechanisms, which helps to increase endurance, resistance of the body to infectious and inflammatory agents. Vitamin C is prescribed in double dosage - 1000 mg per day.
Physiotherapy treatment
The main means of physiotherapy are electrophoresis, light and heat treatment, UHF, laser treatment (for example, when removing stones, sand from the kidneys). Sometimes, halotherapy, balneotherapy, mud therapy, massage are prescribed. Physiotherapy is effective as part of complex therapy. Physiotherapy alone is ineffective.
Folk remedies
As folk remedies, various balms, which include plant components, alcohol, have proven themselves well. Plant components have a therapeutic effect, alcohol has an antiseptic effect. Let's consider the most effective recipes used to eliminate bacterial infections.
- Recipe No. 1.
To prepare, take a tablespoon of calendula flowers, comfrey, lovage, and thistle, pour in about 500 ml of red wine (for example, Cahors), then add half a teaspoon of ground ginger and ground calamus roots. Leave it all for at least 3-4 days, drink 50 ml per day. The course of treatment is at least 28 days (a full biochemical cycle).
- Recipe No. 2.
Take equal parts of wild pansy flowers, smoke tree flowers, rowan berries, gooseberry leaves, and rose hips. Take about 2-3 tablespoons of each component, add about 2-3 tablespoons of honey, 500 ml of alcohol, leave for at least 5 days, drink in small quantities twice a day for 28 days.
- Recipe No. 3.
Vodka or pure alcohol is used as a base. Then approximately one tablespoon of the following components is added: ginseng, celery, peony, calamus. A tablespoon of honey is added. Stir and infused for at least a day.
- Recipe No. 4.
Add a tablespoon of Germander, yellow water lily, sainfoin, Norway maple, rosemary, and asparagus to cognac or cognac spirit (500 ml). Then add 2-3 drops of thuja or juniper essential oil. Drink a tablespoon twice a day.
Herbal treatment
Sage has an anti-inflammatory effect. Plantain has an antiseptic effect, reduces the number of bacteria in any biotopes and biological fluids. Stevia increases immunity, has an antiviral effect, normalizes the state of normal microflora.
All these herbs are recommended to be taken in the form of a decoction. To prepare the decoction, take about a tablespoon of each remedy, pour a glass of boiling water. Infuse for at least 30-40 minutes. Drink a glass per day. You can prepare these herbs both separately and in a complex, in the form of a herbal collection.
Homeopathy
Homeopathic remedies require mandatory compliance with precautions. Thus, when taking homeopathy, you must consult a doctor. He will help to effectively include the remedies in the complex therapy, select the optimal scheme, depending on the characteristics of the course of the pathology, the severity of the condition, the number of bacteria in the urine. Compliance with these basic measures will help to avoid complications. Failure to comply often entails complications such as deterioration of the condition, progression of infection, inflammatory processes. The most dangerous complication is bacteremia and sepsis.
If a large number of bacteria appear in the urine, it is recommended to take a course of therapeutic baths. They are especially effective in case of concomitant kidney diseases, urolithiasis. Baths can be taken only if the body temperature is normal. Baths also promote relaxation, relieve muscle tension, spasm, which significantly reduces pain syndrome, if any.
- Recipe No. 1.
To prepare the bath composition, take honey, cocoa butter and butter in equal parts as a base, melt it all in a water bath or over low heat until dissolved, stirring constantly. Add 2 tablespoons of hop cones, European dodder, forest anemone, small periwinkle and Chinese magnolia vine to the resulting mass. Mix everything until a uniform consistency is formed. Remove from heat and allow to harden. Add to the bath (at a rate of about 3 tablespoons per full bath - 300 liters of water). Store in the refrigerator (on the bottom shelf).
- Recipe No. 2.
As a base for preparing the bath gel, take about 100 ml of kombucha (chaga), diluted with hydrogen peroxide in a ratio of 1:2. Prepare a mixture of the following plant components in advance in a fireproof dish: parsnip, Voronov's snowdrop, rose rhodiola, fragrant rue, medicinal lungwort, garlic tincture (at the rate of about 2 tablespoons of each herb per 100 ml of infusion). Separately take butter (about 100 grams). Heat the oil over low heat (do not bring to a boil). As soon as the oil is hot enough, but has not yet boiled, remove it from the heat, and pour in the previously prepared herbs and the main infusion. Stir, cover with a lid on top, insist in a dark place for a day (at room temperature). After this, the oil is ready for use. It is recommended to add 2 tablespoons per full bath.
- Recipe No. 3.
A mixture of massage base oils is used as a base: avocado oil and camphor oil in a ratio of 1:2, 2-3 drops of vitamins A and E are added. Mix. 2 drops of the following essential oils are added to the resulting mixture: common datura, horehound, common wormwood. Mix thoroughly, use for adding to the bath at the rate of 10-15 grams per bath.
- Recipe No. 4.
The balm for internal use has proven itself well. It is recommended to take it during a bath, which will enhance the effect of the thermal procedure. Vodka or pure alcohol is used as a base. Then add about a tablespoon of the following components: river avens, common wormwood, rose hips, lemongrass fruits, crushed St. John's wort flowers. Mix, insist for at least a day. Drink 2-3 tablespoons twice a day, for at least a month.
- Recipe No. 5.
Add a tablespoon of crushed yarrow flowers, St. John's wort, crushed hemp seeds, and stinging nettle leaves to cognac or cognac spirit (500 ml). Then add 2-3 drops of thuja essential oil. Drink a tablespoon twice a day.
Surgical treatment
If bacteria are present in the urine, surgical treatment methods are not used. They may be required only if a concomitant pathology is detected that requires surgical intervention, for example, a tumor of any genesis and localization. The main method of treating bacteria in the urine is antibiotic therapy.
Prevention
Prevention is based on the need to eat right, include the necessary amount of vitamins and minerals in the diet, regularly undergo preventive examinations, and, if necessary, undergo timely treatment. It is extremely important to maintain a high level of immunity, since the development of a bacterial infection is only possible with reduced immunity and impaired microflora. It is also necessary to fight a viral infection, since the persistence of viruses in the blood creates tension in the immune system and its further decline. [ 18 ]
Forecast
In most cases, with proper and timely treatment, the prognosis will be favorable. Bacteria in the urine of women and men are quite easily eliminated with antibiotic therapy. If left untreated, complications may arise. The main complication is bacteremia and sepsis, which can even end in death.

