Medical expert of the article
New publications
Waldenström's B-cell lymphoplasmacytic lymphoma
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
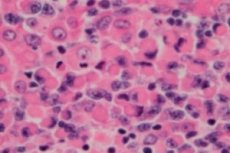
A malignant lymphoproliferative (immunoproliferative) disorder, lymphoplasmacytic lymphoma or Waldenstrom's macroglobulinemia is a cellular neoplasm of small B-lymphocytes – B-cells that provide the protective functions of the lymphatic system and humoral immunity of the body. The diagnosis should be made only after excluding all other small B-cell lymphomas. Waldenstrom's macroglobulinemia was described in 1944 by Jan G. Waldenstrom, who reported unusual manifestations of lymphadenopathic bleeding, anemia, increased sedimentation rate, hyperviscosity, and hypergammaglobulinemia in two patients. [ 1 ], [ 2 ]
Epidemiology
This type of lymphoma is a rare, sluggish hematological malignancy, and clinical statistics estimate its detection rate in this group of diseases at approximately 2%. Moreover, there are almost twice as many male patients as female patients.
According to some data, the incidence of annual cases of lymphoplasmacytic lymphoma in European countries is one in 102 thousand people, and in the USA – one in 260 thousand. [ 3 ]
Causes lymphoplasmacytic lymphoma.
To date, the etiology of most oncological diseases remains unknown, but research into the genetic basis of some of them continues. Studying the causes of malignant plasma cell diseases, including B-cell lymphoplasmacytic lymphoma – Waldenstrom's macroglobulinemia, researchers have discovered a connection between pathological proliferation (cell division) of B- lymphocytes at a late stage of their differentiation with the presence of certain molecular-gene disorders that alter basic cellular functions.
In patients with Waldenstrom's macroglobulinemia, changes in some genes have been identified - somatic mutations, that is, affecting only tissues with damage to the genes of a separate clonal population of cells and forming variants of their genome, which lead to cyclical and structural disorders at the cellular level.
First of all, these are somatic mutations of the MYD88 (L265P) gene and CXCR4, encoding a cytosolic protein that is important for the innate and adaptive immune response: as an adapter, it ensures the transmission of signals from the proinflammatory mediator IL-1 (interleukin-1) and Toll-like receptor cells that activate the immune response. As a result of somatic mutation, anomalies arise in the polypeptide chain of the molecule of this protein - its structural basis. [ 4 ]
Risk factors
In addition to general risk factors (exposure to elevated levels of radiation, carcinogenic chemicals, etc.), the following are considered to be predictors of an increased likelihood of developing Waldenstrom's macroglobulinemia as a low-grade lymphoproliferative disease:
- old age (over 65 years);
- the presence of relatives with this diagnosis, as well as with B-cell non-Hodgkin's lymphoma or chronic lymphocytic leukemia;
- chronic hepatitis C;
- a history of benign monoclonal gammopathy, an idiopathic hematological disease, the essence of which is the production of abnormally altered gamma globulins of type M by lymphocyte plasma cells;
- autoimmune diseases, in particular Sjogren's syndrome.
Pathogenesis
Upon contact with an antigen or stimulation by T-lymphocytes, some B-lymphocytes transform into plasma cells – lymphocytic plasma cells, which, after certain transformations, begin to produce protective globular proteins, i.e. gamma globulins (immunoglobulins or antibodies).
The pathogenesis of lymphoplasmacytic lymphoma/Waldenstrom's macroglobulinemia involves hyperproliferation of B cells, an excess of the lymphocytic plasma cell clone, and excess production of immunoglobulin M (IgM), also called monoclonal immunoglobulin or M protein, in the blood. This is the major antibody with a large molecular weight and pentameric structure, produced during the initial attack on specific bacterial or viral antigens. [ 5 ]
Almost all the symptoms of this disease are associated with manifestations of the activity of M-protein, which can disrupt the rheological properties of blood, increase its viscosity; permeate the lymphoid and myeloid tissues of the bone marrow, accumulate in peripheral lymphoid tissues (with the formation of slowly growing neoplasms capable of exerting pressure on surrounding organs, nerve fibers or blood vessels).
Although chronic lymphocytic leukemia, Waldenstrom's macroglobulinemia or lymphoplasmacytic lymphoma, and multiple myeloma are separate diseases, they all involve increased proliferation of B lymphocytes.
Symptoms lymphoplasmacytic lymphoma.
The first signs of the disease are nonspecific and may include weakness and increased fatigue (due to the development of normochromic anemia), weight loss, shortness of breath, nocturnal hyperhidrosis and recurring subfebrile fever.
In addition, at the initial stage of the disease, there is a disturbance of the sensitivity of the hands and feet, peripheral neuropathy (numbness or tingling in the feet and legs) occurs, small focal hemorrhages of the skin capillaries (purpura) appear, as well as cold urticaria (due to the formation and aggregation of abnormal cryoglobulin proteins in the blood serum).
Symptoms associated with hyperviscosity syndrome include headaches and dizziness, retinal damage and vision loss, tinnitus and hearing loss, cramps, muscle pain, high blood pressure, spontaneous nosebleeds, and bleeding gums. Women may experience uterine bleeding.
Also observed: enlarged lymph nodes (lymphadenopathy); enlarged spleen (splenomegaly); heart failure with cardialgia and heart rhythm disturbances. Although visceral infiltration is rare, the stomach and intestines may be affected, with the development of diarrhea (often with fatty feces). [ 6 ], [ 7 ]
Forms
The 2017 World Health Organization classification of tumors of hematopoietic and lymphoid tissues establishes four diagnostic criteria for Waldenstrom macroglobulinemia, including:
- Presence of monoclonal IgM gammopathy
- Infiltration of bone marrow by small lymphocytes showing plasmacytoid or plasma cell differentiation
- Bone marrow infiltration with intertrabecular structure
- Immunophenotype consistent with Waldenstrom's macroglobulinemia, which includes surface IgM+, CD19+, CD20+, CD22+, CD25+, CD27+, FMC7+, variable CD5, CD10-, CD23-, CD103-, and CD108-
Complications and consequences
Patients with lymphoplasmacytic lymphoma develop complications and consequences in the form of:
- decreased immunity;
- bone marrow failure with disruption of its hematopoietic functions and the development of anemia;
- deficiency of such formed elements of the blood as erythrocytes, leukocytes, platelets;
- lesions of the gastrointestinal tract with chronic diarrhea and impaired intestinal absorption (malabsorption syndrome);
- inflammation of the walls of blood vessels (complex immune vasculitis);
- increased bone fragility (osteoporosis);
- visual and hearing impairments;
- secondary amyloidosis of internal organs;
- progression to paraproteinemic hemoblastosis in the form of multiple myeloma;
- transformation into a highly malignant type of lymphoma – diffuse large B-cell lymphoma.
Diagnostics lymphoplasmacytic lymphoma.
The diagnosis of lymphoplasmacytic lymphoma/Waldenstrom's macroglobulinemia is usually difficult due to the lack of specific morphologic, immunophenotypic, or chromosomal changes. This deficiency makes differentiation of this disease from other small B-cell lymphomas a matter of exclusion.[ 8 ]
In addition to assessing the existing symptoms, to diagnose lymphoplasmacytic lymphoma, a general and biochemical blood test, a coagulogram, immunoelectrophoresis of blood proteins with determination of the level of immunoglobulin M in the blood, and a general urine test are necessary. [ 9 ]
A bone marrow biopsy is required, for which a bone marrow puncture is performed.
Instrumental diagnostics are performed: ultrasound of the lymph nodes and spleen, X-ray of bones, CT scan of the chest and abdominal cavity, ophthalmoscopy.
Differential diagnosis
Lymphoplasmacytic lymphoma is considered a diagnosis of exclusion, therefore differential diagnosis is carried out with B-cell chronic lymphocytic leukemia, multiple myeloma, follicular lymphoma, various subtypes of non-Hodgkin's lymphoma, plasmacytoma, reactive plasmacytosis, angiofollicular lymphoid hyperplasia (Castleman disease), etc.
Who to contact?
Treatment lymphoplasmacytic lymphoma.
It should be borne in mind that Waldenstrom's macroglobulinemia or lymphoplasmacytic lymphoma may be asymptomatic for many years and be diagnosed with an increase in the level of M-protein in the blood.
If there is no symptom, active monitoring is carried out with regular examinations and tests.
Based on the existing symptoms and laboratory test results, a decision is made to begin therapy, which depends on many factors (e.g. age, disease progression, etc.).
According to the protocol, the initial treatment of patients with this type of lymphoma is usually a combination of radiation therapy and chemotherapy with the administration of cytostatics, such as Cyclophosphamide, Doxorubicin, Vincristine, as well as corticosteroids - Metprednisolone or Dexamethasone (Dexasone).
The effectiveness of chemotherapy with drugs from the monoclonal antibody group, in particular, Rituximab, has been proven. [ 10 ]
In cases of generalized disease, Rituximab is used in combination with antitumor nucleoside analogues (Pentostatin, Cladribine). In slowly progressing disease with low levels of monoclonal immunoglobulin M, in addition to Rituximab, the cytostatic Chlorambucil (Leukeran) is used. [ 11 ]
To reduce blood viscosity and stabilize the level of its formed elements, therapeutic hemapheresis is used.
When the level of antibodies in the blood is critically low, replacement therapy with immunoglobulins is carried out to prevent concomitant repeated infections.
As oncohematologists note, despite the fact that treatment can lead to remission of the disease, most patients experience a relapse. If it occurs earlier than 24 months, an antitumor drug such as Ibrutinib (in tablet form) can be used. In case of later relapses, treatment is carried out according to the original scheme. [ 12 ], [ 13 ], [ 14 ]
Prevention
Experts determine the prognosis of the outcome of lymphoplasmacytic lymphoma according to the international prognostic system for assessing the main parameters: the patient's age and serum levels of hemoglobin, platelets, beta-2-microglobulin and monoclonal immunoglobulin. [ 15 ], [ 16 ]
The average survival rate for this diagnosis is about five years, but almost 40% of patients live ten years or longer.

