Bone marrow aplasia
Last reviewed: 25.06.2018

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Bone marrow aplasia (or hematopoietic aplasia) is a syndrome of bone marrow insufficiency, which includes a group of disorders in which the hematopoietic function performed by the bone marrow is sharply suppressed. The consequence of this disorder is the development of pancytopenia (a deficiency of all blood cells is observed: leukocytes, erythrocytes, and platelets). Deep pancytopenia is a life-threatening condition.
Causes bone marrow aplasia
The causes of bone marrow aplasia include the following:
- Chemotherapy and radiation therapy.
- Autoimmune disorders.
- Environmentally harmful working conditions.
- Various viral infections.
- Contact with herbicides and insecticides.
- Some medications, such as those used to treat rheumatoid arthritis or antibiotics.
- Nocturnal hemoglobinuria.
- Hemolytic anemia.
- Diseases of connective tissue.
- Pregnancy - the bone marrow is damaged due to a perverted reaction of the immune system.
Risk factors
Among the risk factors for bone marrow aplasia are those described below.
- chemical compounds: cytostatics - they help stop cell division, they are usually used to treat tumors. A certain dosage of such drugs can damage the bone marrow, disrupting the formation of blood cells; immunosuppressants - suppress the body's immune system, they are used when there is excessive activation of the immune system, which damages its own healthy tissues. If you stop taking them, hematopoiesis is often restored;
- substances that affect the body if the patient has individual hypersensitivity to them. These are antibiotics (antibacterial drugs), gasoline, mercury, various dyes, chloramphenicol, and gold preparations. Such substances can cause both reversible and irreversible destruction of bone marrow function. They can enter the body through the skin, through breathing in aerosols, orally - with water and food;
- irradiation with ionic particles (radiation) – for example, if safety regulations are violated at nuclear power plants or in medical institutions where tumors are treated using radiation therapy;
- viral infections – such as influenza, hepatitis virus, etc.
Pathogenesis
The pathogenesis of bone marrow aplasia has not yet been fully studied. Several different mechanisms of its development are currently being considered:
- Bone marrow is affected through the pluripotent stem cell;
- The hematopoietic process is suppressed due to the influence of humoral or cellular immune mechanisms;
- Components of the microenvironment begin to function incorrectly;
- Development of a deficiency of factors that promote the hematopoietic process.
- Mutations in genes that cause hereditary bone marrow failure syndromes.
In this disease, the content of components (vitamin B12, iron, and protoporphyrin), which are directly involved in hematopoiesis, does not decrease, but at the same time, hematopoietic tissue cannot use them.
Symptoms bone marrow aplasia
Bone marrow aplasia manifests itself depending on which cellular element of the blood was affected:
- If there is a decrease in the level of red blood cells, shortness of breath, general weakness and other symptoms of anemia appear;
- If the level of white blood cells decreases, fever occurs and the body's susceptibility to infections increases;
- If the platelet level is reduced, there is a tendency to develop hemorrhagic syndrome, petechiae, and bleeding.
In partial red cell aplasia of the bone marrow, a sharp decrease in the production of red blood cells, deep reticulocytopenia, and isolated normochromic anemia are observed.
There are congenital and acquired forms of this disease. The second manifests itself in the form of acquired primary erythroblastophthisis, as well as a syndrome that occurs with other diseases (this can be lung cancer, hepatitis, leukemia, infectious mononucleosis or pneumonia, as well as sickle cell anemia, mumps or ulcerative colitis, etc.).
Complications and consequences
Complications of bone marrow aplasia include:
- Anemic coma, in which loss of consciousness occurs, development of a comatose state. There is no reaction to any external stimuli, since oxygen does not enter the brain in the required quantities - this occurs due to the fact that the level of red blood cells in the blood decreases quickly and significantly;
- Various bleedings (hemorrhagic complications) begin. The worst option in this case is a hemorrhagic stroke (some part of the brain is soaked with blood and as a result dies);
- Infections – microorganisms (various fungi, bacteria or viruses) cause infectious diseases;
- Impaired functional state of some internal organs (such as the kidneys or heart), especially with concomitant chronic pathology.
Diagnostics bone marrow aplasia
When diagnosing bone marrow aplasia, the patient's medical history and complaints are studied: how long ago the symptoms of the disease appeared, and what the patient associates their appearance with.
Next, the patient's life history is clarified:
- The presence of concomitant chronic diseases in the patient.
- Presence of hereditary diseases.
- Does the patient have any bad habits?
- It is clarified whether any medications have been taken recently for a long time.
- The presence of tumors in the patient.
- Was there contact with various toxic elements?
- Was the patient exposed to radiation or other radiation factors?
After this, a physical examination is performed. The skin color is determined (with bone marrow aplasia, pallor is observed), the pulse rate is determined (most often it is rapid) and the blood pressure indicators (it is low). The mucous membranes and skin are examined for the presence of hemorrhages and purulent vesicles, etc.
Tests
During the process of diagnosing the disease, some laboratory tests are also carried out.
A blood test is performed - if the patient has bone marrow aplasia, a decrease in the hemoglobin level will be detected, as well as the number of red blood cells. The color index of the blood remains normal. The number of platelets with leukocytes decreases, and in addition to this, the correct ratio of leukocytes is disrupted, because the content of granulocytes decreases.
A urine test is also performed to determine the presence of red blood cells in the urine - this is a sign of hemorrhagic syndrome, or the presence of leukocytes and microorganisms, which is a symptom of the development of infectious complications in the body.
A biochemical blood test is also performed. It determines the levels of glucose, cholesterol, uric acid (to identify concomitant damage to any organs), creatinine, and electrolytes (sodium, potassium, and calcium).
 [ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ]
[ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ]
Instrumental diagnostics
During instrumental diagnostics the following procedures are carried out.
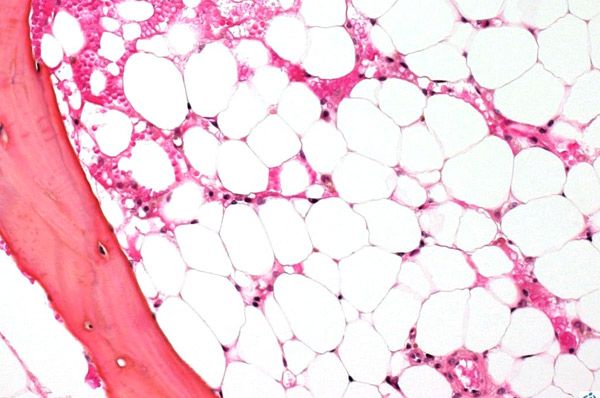
In order to examine the bone marrow, a puncture (piercing, during which the internal contents are extracted) of a bone is performed, usually the sternum or hip bone. With the help of a microscopic examination, the replacement of hematopoietic tissue with scar or fat is determined.
A trephine biopsy, which examines the bone marrow and its relationship with nearby tissues. During this procedure, a special device called a trephine is used - with its help, a column of bone marrow is taken from the ilium along with the periosteum and bone.
Electrocardiography, which allows identifying problems with the nutrition of the heart muscle and heart rhythm.
What tests are needed?
Differential diagnosis
Differential diagnostics are carried out with the following diseases:
- Nocturnal paroxysmal hemoglobinuria;
- Hypoplastic anemia (and also transient erythroblastopenia in children);
- Hypersplenism;
- Myelodysplastic syndrome;
- Acute and hairy cell leukemia;
- SKV;
- DIC syndrome;
- Anemia that develops as a result of hypopituitarism, hypothyroidism or liver disease.
Who to contact?
Treatment bone marrow aplasia
It is almost impossible to eliminate the disease using etiotropic treatment (by affecting its cause). Removing the provoking factor may help (for example, stopping the medication, leaving the radiation zone, etc.), but in this case, the rate of bone marrow death only decreases, but stable hematopoiesis cannot be restored using this method.
Immunosuppressive treatment is used if transplantation is not possible (there is no donor suitable for the patient). In this case, drugs from the cyclosporine A or antilymphocyte globulin groups are used. Sometimes they are used together.
Use of GM-CSF (drugs that stimulate the production of white blood cells). This treatment is used if the white blood cell count drops to less than 2x109 g/L. Corticosteroid drugs may also be used in this case.
Anabolic steroids are used, which stimulate protein formation.
The following methods are used in the treatment of bone marrow aplasia:
- Transfusion of blood elements.
Transfusions are performed with washed red blood cells (donor red blood cells that are freed from proteins) - this method reduces the severity and number of negative reactions to the transfusion procedure. Such transfusions are performed only if there is a threat to the patient's life. These are the following conditions:
- the patient falls into an anemic coma;
- severe anemia (in this case, the hemoglobin level falls below 70 g/l).
Transfusion of donor platelets is performed if the patient experiences bleeding and a clearly expressed decrease in the number of platelets.
Hemostatic therapy is carried out depending on the area where the bleeding began.
When infectious complications occur, the following treatment methods are used:
- Antibacterial treatment. This is performed after nasopharyngeal swabs, as well as urine and blood cultures, have been taken to determine which microorganism caused the infection and to determine its sensitivity to antibiotics;
- Systemic antifungal treatment is mandatory;
- local antiseptic treatment of areas that may become entry points for infection (these are the places through which bacteria, fungi or viruses enter the body). Such procedures usually involve rinsing the mouth with the use of different medications in turn.
Medicines
In case of bone marrow aplasia, drug treatment is mandatory. The most commonly used drugs are those belonging to 3 drug groups: cytostatics (6-mercaptopuril, cyclophosphamide, methotrexate, cyclosporine A, and also imuran), immunosuppressants (dexamethasone, and also methylprednisolone) and antibiotics (macrolides, cephalosporins, chloroquinolones, and also azalides). Sometimes drugs can be used that correct intestinal microflora disorders and problems with blood pressure, enzyme drugs, etc.
Methylprednisolone is prescribed orally. In case of organ transplantation – in a dosage of no more than 0.007 g/day.
Side effects of the drug: water and sodium may be retained in the body, blood pressure increases, potassium loss may occur, osteoporosis, muscle weakness, drug-induced gastritis; resistance to various infections may decrease; suppression of adrenal gland activity, some mental disorders, problems with the menstrual cycle.
The drug is contraindicated in severe hypertension; stage 3 circulatory failure, as well as pregnancy and acute endocarditis, as well as nephritis, various psychoses, osteoporosis, ulcers of the duodenum or stomach; after a recent operation; in the active stage of tuberculosis, syphilis; in the elderly, as well as in children under 12 years of age.
Methylprednisolone is prescribed with caution in the presence of diabetes mellitus, only if there are absolute indications or for the treatment of patients with insulin resistance, with high titers of anti-insulin antibodies. In tuberculosis or infectious diseases, the drug can be used only in combination with antibiotics or drugs that treat tuberculosis.
Imuran - on the first day, it is allowed to use a dose of no more than 5 mg per 1 kg of human weight per day (must be taken in 2-3 doses), but the dosage generally depends on the immunosuppression regimen. The size of the maintenance dose is 1-4 mg / kg of weight per day. It is established depending on the tolerance of the patient's body and his clinical condition. Studies indicate that treatment with Imuran should be carried out over a long course, even using small doses.
Overdose may cause throat ulcers, bleeding and bruising, and infections. These symptoms are more common in chronic overdose.
Side effects - after bone marrow transplantation, patients treated with azathioprine in combination with other immunosuppressants often experience bacterial, fungal or viral infections. Other side effects include arrhythmia, signs of meningism, headaches, lesions of the lips and mouth, paresthesia, etc.
Cyclosporine A is administered intravenously - the daily dose is divided into 2 doses and administered 2-6 hours before. For the initial daily dose, 3-5 mg/kg is sufficient. Intravenous administration is optimal in the treatment of patients who have undergone bone marrow transplantation. Before the transplant (4-12 hours once before the operation), the patient is given a dose of 10-15 mg/kg orally, and then the same daily dose is used for the next 1-2 weeks. Later, the dose is reduced to the usual maintenance dose (approximately 2-6 mg/kg).
Symptoms of overdose include drowsiness, severe vomiting, tachycardia, headaches, and development of severe renal failure.
When taking Cyclosporine, the following precautions must be followed. Therapy must be administered in a hospital by doctors who have extensive experience in treating patients with immunosuppressants. It must be remembered that as a result of taking Cyclosporine, the predisposition to the development of malignant lymphoproliferative tumors increases. That is why it is necessary to decide before starting to take it whether the positive effect of its treatment justifies all the associated risks. During pregnancy, the drug is allowed to be used only due to strict indications. Since there is a risk of anaphylactoid reactions as a result of intravenous administration, antihistamines should be taken for prophylaxis, and the patient should be transferred to the oral route of administration of the drug as quickly as possible.
Vitamins
If the patient has bleeding, in addition to hemotherapy, a 10% solution of calcium chloride (orally) should be taken, as well as vitamin K (15-20 mg per day). In addition, ascorbic acid is prescribed in large quantities (0.5-1 g / day) and vitamin P (at a dosage of 0.15-0.3 g / day). It is recommended to take folic acid in large doses (maximum 200 mg / day), as well as vitamin B6, preferably in the form of injections (50 mg of pyridoxine daily).
Physiotherapy treatment
To activate the bone marrow, physiotherapy is used - diathermy of tubular bones in the shin or sternum area. The procedure should be performed every day for 20 minutes. It should be noted that this option is only possible if there is no pronounced bleeding.
Surgical treatment
Bone marrow transplantation is performed in cases of severe aplasia. The effectiveness of such an operation increases if the patient is young and has had a small number of transfusions of donor blood elements (no more than 10).
This treatment involves extracting bone marrow from the donor and then transplanting it into the recipient. Before the stem cell suspension is introduced, it is treated with cytostatics.
After the transplant, the patient will undergo a long course of immunosuppressive treatment, which is necessary to prevent possible rejection of the transplant by the body, as well as to prevent other negative immune reactions.
Prevention
Primary preventive measures regarding bone marrow aplasia are as follows: it is necessary to prevent the impact of external negative factors on the body. To do this, it is necessary to observe safety precautions when working with dyes or objects that may be sources of ionizing radiation, and also to control the process of using medications.
Secondary prevention, which is necessary to prevent a possible deterioration of the condition of a person with an already developed disease or to prevent a relapse, consists of the following measures:
- Outpatient monitoring. Monitoring should continue even if the patient shows signs of recovery;
- Long-term supportive drug therapy.
Forecast
Bone marrow aplasia usually has an unfavorable prognosis - if timely treatment is not carried out, the patient dies in 90% of cases.
Thanks to donor bone marrow transplantation, 9 out of 10 patients can live more than 5 years. Therefore, this method is considered the most effective method of treatment.
Sometimes it is not possible to perform a transplant, but modern drug therapy can also give results. About half of patients can live more than 5 years thanks to it. But in most cases, patients who became ill at the age of no more than 40 survive.
List of authoritative books and studies related to the study of bone marrow aplasia
- Book: "Aplastic Anemia: Pathophysiology and Treatment" Author: Hubert Schrezenmeier and Andrea Bacigalupo Year: 2009
- Book: "Aplastic Anemia and Other Bone Marrow Failure Syndromes" Author: Neal S. Young and Colin G. Steward Year: 2018
- Study: "Diagnosis and management of acquired aplastic anemia in children" Authors: Monica Bessler and Blanche P. Alter Year: 2016
- Study: "Aplastic Anemia: Pathogenesis, Diagnosis, and Management" Author: Jaroslaw P. Maciejewski and Neal S. Young Year: 2018
- Book: "Aplastic Anemia" Author: John W. Adamson Year: 2009
