Medical expert of the article
New publications
Anaplastic meningioma
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
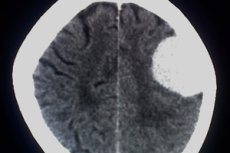
Arachnoid endothelioma or anaplastic meningioma is a tumor pathology originating from arachnoid endothelial tissue. The tumor belongs to the category of relatively malignant, and according to the WHO classification, it is assigned the third degree of malignancy.
Anaplastic meningioma is characterized by rapid growth and intensive penetration into the surrounding healthy structures with subsequent destruction. The tumor is considered aggressive-current, it can increase, reaching large volumes, after only a few months. The malignant process has a well-defined structural cellular atypia. [1]
Epidemiology
Anaplastic meningioma originates from the cells of the arachnoid medulla. It is the most common primary tumor of the central nervous system. It is most often located in the area of the cranial vault (convexital meningioma), the superior sagittal sinus (parasagittal meningioma), and the wings of the main bone.
It is not as common to find the tumor in other parts of the cranial base:
- In the anterior or posterior cranial fossa;
- Of the tuberosity of the Turkish saddle;
- Of the cerebellar tent;
- Lateral ventricles;
- Of the optic nerve sheath.
About 6% of meningiomas are localized in the spinal canal.
Anaplastic meningioma affects mainly elderly and middle-aged patients. In children, the disease is found only in isolated cases. Women have the disease somewhat more often than men, which is due to frequent hormonal changes. [2]
Causes of the anaplastic meningioma
Scientists cannot give a clear cause of anaplastic meningioma. Presumably, some provoking factors are associated with the appearance of the disease, for example:
- Radiation exposure (nuclear, radiation exposure).
- Hereditary predisposition.
- Negative effects of intoxications, chemicals that can enter the body through the respiratory system, mucous membranes, food products.
- Traumatic head injuries, craniocerebral injuries (mainly in the form of remote consequences).
Potential risks may be tobacco smoking, chronic infectious diseases, living in close proximity to power lines, improper diet with a predominance of unnatural foods, frequent stress and negative psycho-emotional mood.
One of the topics for reflection is food carcinogens. We are talking about margarines and hydrogenated oils, sausages and semi-finished products, snacks and chips, sweet carbonated drinks, etc. All these products cause irreparable harm, especially against the background of low consumption of plant-based foods. All of these products cause irreparable harm, especially in the context of low consumption of plant foods.
Exogenous factors have always included the environment, including ionizing radiation, humidity and air pollution. The relationship with the incidence of oncology in this case is direct. Atypical cells begin to grow, divide uncontrollably, forming anaplastic meningioma. [3]
Risk factors
It is important to be aware of the risk factors that increase the likelihood of developing anaplastic meningioma:
- Advanced age;
- Oncologic pathologies in the anamnesis (even successfully treated);
- Cancer pathologies in blood relatives;
- Smoking, alcohol abuse;
- Metabolic disorders, head trauma;
- Certain infectious processes - for example, human papillomavirus;
- Exposure to chemical and toxic agents;
- Ionizing effects (including ultraviolet rays).
The risks of CNS neoplasms, including anaplastic meningioma, are repeatedly increased against the background of immunosuppression, provoked by drug therapy in tissue and organ transplantation, as well as in other cases of severe weakening or stress of the immune system. [4]
Pathogenesis
In some patients, the development of anaplastic meningioma may be due to the presence of one of the hereditary pathologies, in particular, neurofibromatosis types I and II, and so on. The majority of such syndromes are transmitted by autosomal dominant inheritance. However, the share of inherited diseases is no more than 5-6%. The remaining percentage of cases of primary anaplastic meningiomas occurs sporadically - that is, without any clearly defined cause.
Diffuse type of growth with penetration (sprouting) into nearby healthy brain tissue is typical for this tumor process.
The question of provoking factors in the development of anaplastic meningioma is still relevant. There is a high probability of genetically determined diseases, but heredity does not prevail in all cases. Possible mutations are expressed by a violation of the number of chromosomes, DNA damage. These changes do not affect the whole organism, but only the tissues of a certain localization. Acquired mutations or generative are based on the concept of "cancer factors", but are not always transmitted "by inheritance".
Thus, the pathogenetic mechanism of meningioma development should be considered individually. To the occurrence of the pathological process are more predisposed to those people who have had cases of the disease among the closest relatives. If there were tumors of the central nervous system in the family line, the risk of anaplastic meningioma actually doubles.
Symptoms of the anaplastic meningioma
The symptomatology of anaplastic meningioma is diverse and depends mainly on the localization and prevalence of the pathological process. The leading place in determining the clinical picture is occupied by the evaluation of neurological signs.
- General cerebral symptoms:
- Head pain;
- Increased blood pressure, hydrocephalus.
- Focal neurologic symptoms:
- Impairment or loss of some functions - particularly motor and sensory impairment, cranial nerve dysfunction, mental and speech disorders, memory impairment, etc.;
- Seizures.
- Endocrine disorders (when the pituitary gland is involved).
Depending on the course, aplastic meningiomas can be overt and asymptomatic. The first signs often appear abruptly - for example, in the form of an epileptiform or hydrocephalus-occlusive seizure, or hemorrhage.
The most common initial manifestations of the disease:
- Pain in the head (dull, constant, prone to worsening);
- Vomiting, nausea unrelated to food intake;
- Dizziness, vestibular disorders;
- Visual impairment, speech impairment;
- Seizures;
- Decreased sensation, weakening of the limbs, paresis or paralysis (more often unilateral).
Stages
Grade-classification of meningiomas:
- Benign neoplasms, without sprouting into surrounding tissues.
- Malignant foci with a high recurrence rate, relatively aggressive and rapid growth.
- Malignant foci with a high rate of recurrence, rapid growth and involvement of surrounding brain tissue.
Chang-classification:
- T1 - neoplasm up to 30 cm in diameter, with localization within the cerebellar vermis and the roof of the 4th ventricle.
- T2 - neoplasm over 30 mm in diameter, with sprouting into adjacent tissues, or with partial filling of the 4th ventricle.
- T3A - a nidus over 30 mm in diameter growing into the area of the cerebral conduit or into the foramen of Luschka and Majandie, provoking hydrocephalus.
- T3B - foci over 30 mm, growing into the brainstem.
- T4 - mass over 30 mm with hydrocephalus caused by blockage of the cerebrospinal fluid outflow pathway and with sprouting into the brain stem.
- M0 - no metastases.
- M1 - microscopy reveals tumor cells in the cerebrospinal fluid.
- M2 - metastasis within the subpautine space of the 3rd and 4th ventricles.
- M3 - metastasis to the subpautine space of the spinal cord.
- M4 - metastasis beyond the central nervous system.
Forms
Meningiomas have different histological species affiliation. According to this principle, the following types of pathology are distinguished:
- Meningotheliomatous meningioma includes mosaic-appearing cells with a round or oval nucleus and a moderate number of chromatin. The tumor stroma has a small vasculature and thin connective tissue fibers encircling the cell fields. The structure is typical, consisting of layering of squamous tumor cells, with a calcified central part of the focus.
- Fibrous meningioma is represented by fibroblast-like structures arranged in parallel and intertwined in the form of bundles containing connective tissue fibers. The shape of the nuclei is elongated.
- The transitional neoplasm consists of elements of fibrous and meningotheliomatous meningioma.
- A psammomatous neoplasm includes many psammomas.
- Angiomatous meningioma is provided with a well-developed vascular network.
- Microcystic meningioma is represented by multiple microscopic cysts surrounded by tumor cells of star-like configuration.
- Secretory meningioma is a rare tumor that tends to secrete components that form hyaline inclusions.
- Metaplastic meningioma is accompanied by transformation of meningothelial structures into structures of other types.
Complications and consequences
The probability of anaplastic meningioma recurrence after treatment is estimated at 60-80%. The survival rate usually does not exceed 2 years.
At the postoperative stage, it is possible to develop complications of infectious-inflammatory nature, including wound suppuration, meningitis, purulent processes in the cranial bones, etc. Such complications require intensive antibiotic therapy, sometimes - repeated surgical intervention. [5]
In patients with blood coagulation disorders or a tendency to hypertension in the initial postoperative phase, it is possible to develop internal bleeding in the area of the operation. [6]
Other possible complications include:
- Recurrence of anaplastic meningioma (relapse);
- Spread of daughter tumor foci to other tissues and organs (metastasis).
Diagnostics of the anaplastic meningioma
Magnetic resonance imaging of the brain is considered the diagnostic standard for suspected primary tumor of the central nervous system. Contrast agent injection, T1 modes without contrast enhancement, T2 modes, T2 FLAIR, T1 with contrast enhancement or in three projections or in SPGR mode are used. These methods provide the most complete information about the location, scale, structure of the neoplasm, its penetration into neighboring tissues, sprouting into vessels.
The basic criterion for the final diagnosis of anaplastic meningioma is the result of histologic analysis. The main features of a highly malignant tumor process are considered to be cell atypia, polymorphism, small cytoplasmic volume, high mitotic activity, dense localization of cell elements, proliferation of vascular endothelium, areas of pinpoint hemorrhages and tissue necrosis, and altered intercellular matrix.
In severe cases with a marked risk of mortality, the diagnosis of anaplastic meningioma can be made on the basis of clinical and radiologic information. [7]
Blood tests - general and biochemical - are prescribed as part of standard diagnostic measures. The quality of blood coagulation, the likelihood of anemia and inflammatory processes are assessed.
- Extended clinical blood work.
- Blood biochemistry (urea, creatinine, total protein, albumin, total bilirubin, lactate dehydrogenase, alanine aminotransferase, aspartate aminotransferase levels).
- Study of the blood coagulation system, indicators of hemostasis.
- Blood tests for tumor markers (plasma AFP, chorionic gonadotropin, lactate dehydrogenase activity).
Molecular genetic analysis of IDH1-IDH2 gene mutations in the biomaterial as well as assessment of MGMT gene methylation is recommended.
Instrumental diagnosis is presented in most cases:
- With a CT scan with contrast;
- MRI with contrast.
The benefit of early diagnostic measures should not be underestimated, because anaplastic meningioma grows faster over time and becomes more aggressive towards neighboring tissues and structures, which can pose a direct threat to the patient's life. [8]
Differential diagnosis
Differential diagnosis is performed with non-oncological pathologies - for example, with hemorrhage in patients with arterial or arteriovenous malformations, with pseudotumorosis type of demyelinating process, inflammatory diseases of the brain (abscesses, toxoplasmosis, etc.).
In addition, primary tumor processes of the central nervous system and metastases are distinguished. For this purpose, magnetic resonance imaging is performed, which identifies anaplastic meningiomas with a fairly high accuracy and indicates the distinguishing points from other similar pathologies.
When indicated, the attending physician may order a CT scan with or without contrast, CT angiography or MR angiography, magnetic resonance tractography, functional MRI with evaluation of motor areas and speech centers, CT perfusion or MR perfusion.
Who to contact?
Treatment of the anaplastic meningioma
The meningioma is not always located in a way that would be convenient for its removal. Surgery is only indicated when there is no or minimized risk of damage to important functional brain areas.
Anaplastic meningioma is considered a malignant neoplasm, although it has the properties of both malignant and benign tumors. The pathological process can destroy brain tissue, squeeze it, spread metastases. To stop the disease, mainly surgical (optimally) and radiosurgical tactics are used.
A contraindication to performing surgery is considered to be:
- The patient's advanced age;
- Lack of adequate access to the nidus (e.g., its growth into the cavernous sinus).
Classical radiation therapy is practically not used due to its ineffectiveness and high probability of damage to healthy areas of the brain and spinal cord. In some cases, radiation is prescribed in combination with surgical resection to destroy the pathologic focus in inoperable areas, or to reduce the risk of meningioma re-formation.
Radiation therapy with the CyberKnife device is considered one of the most modern and minimally traumatic ways to eliminate meningiomas with diametric sizes up to 35-40 mm. A stream of ionizing radiation is directed at the focus. The risk of damage to surrounding structures is minimized.
Thanks to the CyberKnife, anaplastic meningiomas can be safely removed. The procedure is performed on an outpatient basis and no hospitalization is required. [9]
Medications
It is possible to administer chemotherapy on individualized regimens, [10] for example:
- Lomustine 100 mg/m², Vincristine 1.5 mg/m², Procarbazine 70 mg/m²;
- Temozolomide as part of chemoradiation treatment 75-100 mg/m²;
- Temozolomide 150-200 mg/m², Cisplatin or Carboplatin 80 mg/m².
The following regimens are indicated for recurrent anaplastic meningioma:
- Bevacizumab 5-10 mg/kg (day 1, 15) and Irinotecan 125-200 mg/m² (day 1, 15) every 28 days;
- Bevacizumab 5-10 mg/kg (day 1, 15, 29) and Lomustine 90 mg/m² (day 1) every 6 weeks;
- Bevacizumab 5-10 mg/kg (day 1, 15) and Lomustine 40 mg/m² (day 1, 8, 15, 22) every six weeks;
- Bevacizumab 5-10 mg/kg (day 1, 15) every 28 days.
Complementary therapy is also prescribed on an individual basis:
- Corticosteroid drugs Dexamethasone, Prednisolone in doses depending on the severity of symptoms (the minimum effective dosage is prescribed). After regression of symptoms, the dose is gradually reduced until complete withdrawal. Simultaneously with corticosteroids it is recommended to take gastroprotectors (proton pump blockers). In case of severe edema, additionally prescribe saluretics (Furosemide) or osmotic diuretics (Mannitol).
- In the presence of seizures or epileptiform manifestations, anticonvulsants are used. Valproic acid, Levetiracetam, Lamotrigine are preferred. The use of carbamazepine, phenobarbital and phenytoin against the background of chemotherapy is highly undesirable. In order to prevent seizures, anticonvulsants are not used. Therapy regimens are individualized.
- Analgesics are prescribed for patients with spinal cord or spinal column lesions. They are mainly narcotic analgesics such as Fentanyl, Trimeperidine in individual doses.
- Correction of hemostasis involves the perioperative administration of low-molecular-weight heparins, such as calcium nadroparin, sodium dalteparin, etc., to prevent pulmonary embolism. Patients who constantly take blood thinning drugs (Aspirin, Clopidogrel), replace them with low-molecular-weight heparins no later than a week before the intervention, with further withdrawal a day before surgery and resumption 48 hours after surgery.
Surgical treatment
The operation is performed to reduce the size of anaplastic meningioma as much as possible, as well as to normalize intracranial pressure, reduce neurological insufficiency and remove the necessary morphological material.
To perform the resection and biopsy, the patient is admitted to a special neurosurgical department or clinic, whose specialists have experience in performing neuro-oncological interventions. Microsurgical techniques and a surgical microscope must be used during the operation.
Operative access is performed by bone-plastic trepanation in the projection of the intended surgical manipulations.
If the operation is planned to be performed anatomically close to the motor areas of the cortex or motor pathways, or near the nuclei of cranial nerves, intraoperative electro-physiologic monitoring is additionally included.
It is optimal to intervene within two weeks of diagnosis. Failure to do so may result in rapid worsening of the neurologic picture and the development of a life-threatening condition.
Neuronavigation suites and intraoperative fluorescence navigation with 5-aminolevulenic acid are used to make the surgery as complete and radical as possible.
At the postoperative stage, patients with resection of anaplastic meningioma undergo contrast-enhanced computed tomography or magnetic resonance imaging.
Prevention
Provoking factors of development and methods of prevention of cancer development of the central nervous system are constantly studied by scientists all over the world. Unfortunately, thousands of people are diagnosed with meningiomas every year, and most of these patients cannot be cured of the disease due to late detection.
It is important that absolutely all risk factors should be perceived within the framework of individual responsibility for their own health. The recommendations on nutrition, elimination of bad habits, the need for protection from ultraviolet radiation are often ignored by most people. Despite the presence of proven and logical root causes, people continue to abuse alcohol, smoke, consume products containing a lot of carcinogens.
The simplest and most affordable prevention involves, first and foremost, leading a healthy lifestyle. This significantly reduces the risks of anaplastic meningioma and other malignant neoplasms, and increases the chances of survival for many patients who are already fighting the disease.
Forecast
The outcome of the pathology depends on the location, prevalence of anaplastic meningioma. In many cases, neoplasms recur, metastasize, which significantly worsens the prognosis of the disease. It is not always possible to completely remove such tumor processes - for example, there are difficulties with resection of meningiomas of the falx tentorial angle, cranial base and cavernous sinus, petroclival foci, multiple masses.
Due to the diverse and unclear symptomatology, timely diagnosis is often difficult. In elderly patients, the picture of tumor process is sometimes mistaken for age-related brain changes, which further aggravates the situation. It is very important to suspect the problem in time and refer the patient for diagnostic measures - magnetic resonance and computer tomography, as well as for consultation with an oncologist, neurosurgeon, radiotherapist.
On average, anaplastic meningioma recurs in 70% of cases. Survival is limited to 1-2 years.

