Medical expert of the article
New publications
Allergic vasculitis - causes, symptoms and treatment
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Allergic vasculitis is an inflammatory process of the vessel walls that occurs as a result of an allergic reaction. Allergic vasculitis is characterized by the predominant involvement of small-caliber blood vessels in the pathological process. Both men and women are susceptible to it, regardless of age.
Predisposing factors for allergic vasculitis are:
- Metabolic disorders:
- overweight,
- presence of diabetes mellitus,
- gout,
- atherosclerosis.
- Autoimmune diseases:
- systemic lupus erythematosus,
- rheumatoid arthritis.
- Cardiovascular pathology:
- hypertension,
- heart failure.
- Liver diseases and other concomitant pathologies:
- cirrhosis,
- inflammatory bowel disease,
- human immunodeficiency virus (HIV),
- malignant tumor, etc.
Vasculitis is classified according to clinical and histological manifestations, the size of the affected blood vessels and the depth of the pathological process.
Depending on the diameter of the affected blood vessels, allergic vasculitis is divided into:
- superficial (dermal vasculitis), when arterioles, venules and capillaries of the skin are affected,
- deep (dermo-hypodermal vasculitis), when medium and large caliber arteries and veins (the so-called muscular type vessels) are affected.
Infectious toxic agents play an important role in the formation of allergic vasculitis, stimulating the production of circulating immune complexes (CIC), which are deposited on the vascular endothelium (walls). Ultimately, the endothelium of blood vessels is damaged, an inflammatory process and increased permeability develop in it - allergic vasculitis is formed. The severity of vasculitis depends on the amount of CIC in the bloodstream.
 [ 1 ]
[ 1 ]
Causes of allergic vasculitis
There are several causes of allergic vasculitis.
- Infectious nature of occurrence:
- bacterial flora (ẞ - hemolytic streptococcus group A, tuberculosis mycobacterium, Staphylococcus aureus, leprosy);
- viral flora (flu, herpes, hepatitis A, B and C);
- fungal diseases (genus Candida).
- Reaction to taking medications:
- antibacterial drugs (penicillins, sulfonamides, streptomycin);
- insulin use;
- vitamin complexes;
- taking oral contraceptives;
- administration of streptokinase, etc.
- Exposure to food allergens – dairy proteins, gluten.
- The influence of chemical compounds – petroleum products, insecticides, household chemicals.
 [ 2 ]
[ 2 ]
Symptoms of allergic vasculitis
The leading clinical symptom of allergic vasculitis with damage to small-caliber vessels is palpable purpura. Palpable purpura is a hemorrhagic rash slightly raised above the skin (at the initial stage of the disease it may not be palpable).
In cases where blood coagulation is impaired and thrombocytopenia is observed, hemorrhages (petechiae) are clinically presented as spots and are not palpable. Allergic vasculitis is characterized by the occurrence of inflammatory infiltrates, which is why they are presented as papules that can be palpated.
The size of the rash in allergic vasculitis varies from a few millimeters to several centimeters. A characteristic feature is the symmetry of the rash.
In the case of a severe inflammatory process, palpable purpura transforms into a vesicular rash filled with hemorrhagic contents. Subsequently, necrosis and ulcers form in place of such blisters. In this connection, the following forms of allergic vasculitis are distinguished:
- papular,
- vesicular,
- bullous,
- pustular,
- ulcerative.
Sometimes allergic vasculitis may cause itching and soreness in the affected areas. After the rash heals, hyperpigmentation remains, and atrophic scars may also form.
Most often, the rash is located on the legs, although it is possible that it will spread to other areas (usually not affected are the face, mucous membranes, palms and soles).
Allergic vasculitis of the skin
Allergic vasculitis of the skin is a polyetiological set of diseases and their clinical symptom complex is very diverse. But the main clinical symptom is damage to the skin from spots to ulcers (i.e. polymorphism of the rash is characteristic). The rash is often accompanied by itching, burning or pain. In parallel with the damage to the skin, a deterioration in general health is noted: high temperature, lethargy, myalgia and arthralgia, loss of appetite, vomiting and pain in the abdomen.
There is no classification of allergic vasculitis of the skin as such, their division occurs from the depth of the damaging process. In this regard, superficial and deep vasculitis are distinguished.
Superficial allergic vasculitis is divided into:
- Hemorrhagic vasculitis (Schonlein-Henoch disease).
- Allergic arteriolitis of Ruiter.
- Hemorrhagic leukoclastic microbead of Miescher-Stork.
- Werther-Dumling nodular necrotizing vasculitis.
- Acute variolous lichenoid parapsoriasis.
- Hemosiderosis (capillaritis)
- annular telangiectatic purpura,
- eczematoid purpura,
- Schamberg's disease,
- pruritic purpura,
- purpuric pigmented lichenoid dermatitis,
- arcuate telangiectatic purpura,
- white atrophy of the skin,
- purpuric pigmented angiodermatitis,
- orthostatic purpura,
- reticular senile hemosiderosis.
- Hemosiderosis (capillaritis)
- Among deep allergic vasculitis, the following are distinguished:
- Cutaneous form of periarteritis nodosa.
- Erythema nodosum - acute and chronic forms.
Hemorrhagic vasculitis (Schonlein-Henoch disease)
Caused by systemic damage to the vascular endothelium, with the formation of erythema on the skin surface, which soon transforms into hemorrhagic elements. This form of vasculitis is characterized by damage to joints and vital organs (mainly the stomach, intestines and kidneys). Most often it develops in children as a result of an infectious disease (in ten to twenty days). It is characterized by an acute onset, an increase in temperature, and an intoxication syndrome.
The following types of hemorrhagic vasculitis are distinguished (conditionally):
- simple purpura,
- necrotic,
- rheumatic (articular),
- abdominal,
- lightning fast view.
The rash in hemorrhagic vasculitis is symmetrical, located on the legs and buttocks, and does not disappear when pressed. The rash is wave-like, and appears on average once a week. Joint damage occurs simultaneously with skin damage or after a couple of hours. Damage to large joints (knees, ankles) is typical.
With simple purpura, only skin rashes are observed. General well-being is not affected and internal organs are not affected, and if they are involved in the pathological process, then insignificantly. Acute course is typical for a child's body. The duration of the disease can vary from a couple of days to a couple of weeks. The rash in the form of erythematous spots can be up to two millimeters in size, but sometimes reach two centimeters. At the same time as the spots, urticarial elements are formed, accompanied by itching of the skin. Usually, with simple purpura, the rash passes without a trace, only in rare situations can hyperpigmentation remain.
Necrotic purpura is characterized by polymorphism of the rash, when the skin simultaneously has spots (erythema), nodular rash, blisters (with hemorrhagic or serous filling) and necrotic changes in the skin, ulcers and crusts of a hemorrhagic nature. After healing of the ulcers, scars often remain.
Rheumatic purpura is characterized by simultaneous damage to the skin and joints. Large joints (knees and ankles) are often damaged, they become painful and swelling is visible above their surface. Joints are affected simultaneously with skin damage, but can also precede vasculitis or vice versa - after a couple of hours or even weeks. The skin above the joints becomes yellow-green, which indicates that there was a hemorrhage here.
The abdominal form of hemorrhagic vasculitis often occurs in early childhood and adolescence. It is difficult to diagnose, since the rash on the skin may be absent and manifests itself only by symptoms of damage to the digestive tract - the presence of pain in the epigastrium and intestines, vomiting, when palpating - the anterior abdominal wall is tense and painful. Kidney damage is characterized by a variety of manifestations from minor disorders to a picture of acute glomerulonephritis, which may disappear or become chronic.
Lightning form - proceeds very hard, with high temperature, with generalized rash located on the surface of the skin and mucous membranes. The lightning form is characterized by damage to joints, vital organs. Extremely unfavorable course for life.
Ruiter's allergic arteriolitis
Infectious-allergic vasculitis of the skin. It develops during pathology of an infectious nature, in the presence of chronic infectious foci (tonsillitis, sinusitis, adnexitis, etc.). It is characterized by polymorphism of the rash - erythematous and hemorrhagic spots, vesicular and nodular rash, necrotic changes, ulcers, serous or hemorrhagic crusts. At the end of the disease, hyperpigmentation and scars remain. General well-being is impaired: weakness, lethargy, increased temperature, poor appetite. A long course of the disease with remissions and exacerbations is typical.
 [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
[ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
Miescher-Stork hemorrhagic leukoclastic microbead
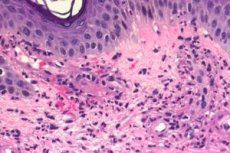
It occurs acutely as a result of a chronic infectious process. The rash is represented by erythematous and hemorrhagic spotted elements on the surface of the skin of the arms and legs, very rarely - on the face and in the area of the mucous membranes. During exacerbations, the general state of health changes - the temperature rises, appetite decreases, weakness appears. An intradermal test with a bacterial filtrate (streptococcal antigen obtained from the tonsils) is positive. During histological examination, significant leukoclasia is noted, characterized by the disintegration of the nucleus of granular leukocytes.
Werther-Dumling nodular necrotizing vasculitis
The main manifestation of this disease is brownish-bluish dermal-hypodermal flat papules (nodules), congestive in nature, dense when palpated, pea-sized. Along with papules, erythematous spots are noted, often transforming into hemorrhagic elements. Papular rashes become necrotic over time and ulcerative defects appear, forming into scar tissue (atrophic or hypertrophic scars). Burning and pain are usually absent. The rash is symmetrical, appears in the area of the extensor surfaces of the arms and legs, and is sometimes located around the joints (rashes may also be located on the torso and genitals). The disease lasts a long time with periods of exacerbations and remissions. During an exacerbation, the general state of health changes, and a rise in temperature is possible.
 [ 13 ]
[ 13 ]
Acute variolous lichenoid parapsoriasis
Papulosquamous skin disease with an acute course and unknown etiology. It is assumed that it occurs as a reaction to an infection. It often occurs in adolescence and young adulthood. Small follicular papules form on the skin, which transform into pustules with necrosis in the center. General well-being is impaired: the temperature rises, lymphadenitis usually occurs.
 [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
[ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
Hemosiderosis (capillaritis)
They arise as a result of hemosiderin deposition on the inner walls of blood vessels (precapillaries and capillaries). Hemosiderin is a pigment containing iron and formed as a result of hemoglobin breakdown. Hemosiderosis is characterized by: petechial rash, small brown-yellow spots and vascular asterisks. The rash is located in the area of the arms and legs (their distal parts), more in the area of the legs and is accompanied by a burning sensation of varying severity. General well-being and vital organs are not affected.
 [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
[ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
Cutaneous form of periarteritis nodosa
Allergic vasculitis of a generalized nature, accompanied by damage to arteries of the muscular type (medium and large). Capillaries are not included in the pathological process. More often this pathology is characteristic of men. It develops on the introduction of drugs - vaccines, serums, antibiotics, and also as a reaction to bacterial and viral infections. The disease often occurs acutely, less often subacutely. The temperature rises, weakness and loss of appetite appear. Nodules (thickenings) in the form of aneurysmal protrusions of blood vessels are formed along the arteries. Vascular occlusion, thrombus formation, followed by hemorrhage, ulceration and possible secondary infection occur. Vital organs (kidneys, digestive system, etc.) are subsequently affected. Rashes on the surface of the skin are represented by nodular rash - single or grouped, dense, mobile and painful. The rash is prone to necrosis and ulceration. Ulcerative defects bleed and heal for a long time.
 [ 24 ], [ 25 ], [ 26 ], [ 27 ]
[ 24 ], [ 25 ], [ 26 ], [ 27 ]
Erythema nodosum
A type of allergic vasculitis characterized by the formation of dense painful nodules and nodes, which are usually located in the shin area (on their anterior surface) symmetrically. After the healing of the nodular rash, a long-term compaction is noted, ulcers and scars are not typical. Often observed in women at a young age. A distinction is made between acute and chronic course. During the acute course of erythema nodosum, an increase in temperature, the occurrence of weakness, headache, myalgia and arthralgia are observed.
 [ 28 ], [ 29 ], [ 30 ], [ 31 ]
[ 28 ], [ 29 ], [ 30 ], [ 31 ]
Allergic vasculitis in children
Allergic vasculitis in children is characterized by a more acute onset, is severe and has more pronounced symptoms than in adults. Skin rashes tend to generalize. General well-being suffers greatly - there may be a high temperature reaction, lethargy, weight loss, loss of appetite, nausea, vomiting, pain in the epigastrium and intestines, arthralgia and myalgia, more pronounced symptoms of the inflammatory process. Allergic vasculitis is especially difficult to bear if vital organs and systems are involved in the process. A distinctive feature of allergic vasculitis in children is more frequent relapses. In childhood, hemorrhagic vasculitis (Schonlein-Henoch disease) and nodular periarteritis occur.
Risk factors in the development of allergic vasculitis in children are.
- Genetic predisposition to cardiovascular and rheumatic pathology.
- Frequent acute infectious diseases.
- A chronic infectious process in the body.
- The occurrence of a hyperergic reaction to medications, food products, insect bites.
- Vaccination.
- Hypothermia.
- Helminths often provoke the development of vasculitis.
- Compromised immunity.
 [ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ]
[ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ]
Infectious-allergic vasculitis
Infectious-allergic vasculitis is a hyperergic disease that occurs during infectious diseases due to accompanying toxic-allergic reactions. The cause of vasculitis is the damaging effect of infectious agents and their toxins on the walls of blood vessels. Skin rashes are polymorphic, and general well-being suffers significantly. Infectious-allergic vasculitis most often occurs with streptococcal and staphylococcal lesions of the body, with viral infections (flu, hepatitis), with tuberculosis, etc.
 [ 37 ]
[ 37 ]
Toxic-allergic vasculitis
Toxic-allergic vasculitis is a skin lesion that occurs as a response to substances that are allergens and have a toxic effect (medicines, food, chemicals). These substances can enter the body:
- when taken orally (through the digestive system),
- through the respiratory tract,
- during intravenous, intradermal or intramuscular administration.
The disease usually develops acutely. The rash can be polymorphic - urticarial, measles-like, scarlatino- or rubella-like, in the form of purpura, lichenoid, eczematous, etc. The rash is located on the skin and mucous membranes. The rash is accompanied by a deterioration in general health: an increase in temperature, itching and burning of the affected areas, dyspepsia (nausea, vomiting, abdominal pain), muscle and joint pain, and damage to the nervous system. In case of repeated contact with the factor that caused vasculitis, the rash usually appears in the same place, although it is possible that it will appear in a new place. A very severe course of toxic-allergic vasculitis is also possible - Lyell's syndrome and Stevens-Johnson syndrome.
Lyell's syndrome is a severe allergic bullous skin lesion. It begins acutely, the general health progressively worsens, and the intoxication syndrome rapidly increases. The skin rash is measles-like or scarlet fever-like, painful. After a couple of hours, the rash transforms into blisters filled with serous or serous-hemorrhagic contents. Quickly opening, they form bright red erosions. Light rubbing of healthy skin is accompanied by desquamation of the epidermis and exposure of the weeping surface (Nikolsky's symptom). Internal organs are often affected - the heart, liver, kidneys, intestines. Lyell's syndrome requires immediate medical attention.
Stevens-Jones syndrome is a severe form of exudative erythema. It begins suddenly and acutely with a rise in temperature. A false film of yellowish or white-yellow color forms on the conjunctiva, which can be removed. This film disappears on average in a month. If the course of the disease is complicated, a corneal leukoma and conjunctival scars occur. In parallel with the damage to the conjunctiva, the skin is also affected, erythematous spots, blisters, tubercles are formed on it, swelling and serous-bloody exudation on the lips, mucous membrane of the oral cavity occur. An unpleasant odor of purulent discharge from the mouth, external genitalia is released.
Systemic allergic vasculitis
Systemic allergic vasculitis is a disease that occurs as a result of inflammatory damage to the walls of blood vessels of an autoimmune nature with various clinical manifestations. Systemic allergic vasculitis includes:
- Nodular polyarteritis.
- Wegner's giant cell granulomatosis.
- Takayasu's arteritis (non-specific aortoarteritis).
- Hamman-Rich, Goodpsucher, Kawasaki, Churg-Strauss, Lyell and Stevens-Johnson syndromes.
- Buerger's disease, Horton's disease, Behcet's disease, Christian-Weber disease, Moschkowitz disease.
- Vasculitis in large and small collagenoses (systemic scleroderma, systemic lupus erythematosus, rheumatism, rheumatoid arthritis).
Systemic allergic vasculitis is characterized by the simultaneous involvement of many organs and systems in the pathological process. A distinctive feature is the presence of a pronounced exudative component, cyclicity in the course of the process and signs of sensitization, as well as the presence of histomorphological criteria of fibrinoid degeneration of the main substance of the connective tissues of the vascular walls.
Diagnosis of allergic vasculitis
Diagnosis of allergic vasculitis is based on:
- medical history,
- complaints,
- clinical picture,
- additional examination methods:
- general clinical laboratory tests (complete blood count, urine analysis, biochemical blood test, blood sugar test),
- determination of ASL-O in case of suspected diseases caused by beta-hemolytic streptococcus,
- conducting a quantitative analysis of blood immunoglobulins,
- determination of CIC (circulating immune complexes),
- bacteriological examination of nasopharyngeal smears, as well as urine and feces,
- examination of women by a gynecologist,
- PCR testing to detect various infections,
- conducting ECG and angiography, radiography,
- conducting ultrasound diagnostics of blood vessels,
- Consultations with specialists: dermatologist, phthisiologist, cardiologist, vascular surgeon, rheumatologist, venereologist.
 [ 38 ]
[ 38 ]
What do need to examine?
Who to contact?
Treatment of allergic vasculitis
Treatment of allergic vasculitis is complex.
- It is necessary to prevent the allergen from affecting the body, which contributed to the development of allergic vasculitis: stop taking the medicine or some product, exposure to chemical agents, etc.
- Bed rest is necessary, especially during the acute phase of the disease.
- A diet with lots of vegetables, fruits and protein products (limit salty, fried and fatty foods). In the diet, exclude foods that cause allergies (these can be citrus fruits, honey, nuts, chocolate, red fish, etc.).
- Drink plenty of fluids for the purpose of detoxification therapy (at least 1.5-2 liters per day). In severe cases, intravenous drip administration of physiological solutions with drugs.
- Detection and treatment of chronic infection. In which case it is possible to prescribe antibacterial drugs (from the macrolide group - sumamed, cephalosporins - cefotaxime, etc.).
- Often, especially in severe cases, glucocorticosteroids are prescribed, which have anti-inflammatory, antihistamine, and immunosuppressant effects (prednisolone, dexamethasone).
- In complex therapy the following are used:
- antiplatelet drugs – reduce thrombus formation (pentoxifylline, acetylsalicylic acid, clopidogrel, curantil, trental),
- vascular protectors that increase vascular tone, reduce their permeability, and reduce bleeding (ascorutin, dicynone, etamsylate),
- inhibitors of proteolytic enzymes, improve microcirculation, tissue respiration and reduce thrombus formation (aminocaproic acid),
- antihistamines (erius, tavegil, suprastin),
- non-steroidal anti-inflammatory drugs (dicloberl, movalis).
- Prescribing vitamins C and P (they have antioxidant effects, strengthen the walls of blood vessels, and improve immunity).
- It is possible to use medications for local application, especially during the healing period - solcoseryl, troxevasin (improve and accelerate healing).
- Extracorporeal methods of therapy for allergic vasculitis are widely used:
- plasmapheresis (this method removes part of the plasma containing harmful substances – toxins, antigens, etc.),
- hemosorption (this technique is used to remove toxins, antigens, and immune complexes from the blood).
A set of treatment measures is prescribed strictly individually for each case of allergic vasculitis. The causes of its occurrence, clinical picture, severity and acuteness of the process and age are taken into account.
Prevention of allergic vasculitis
Prevention of allergic vasculitis consists of the following.
- Timely and correct treatment of diseases that may lead to the development of vasculitis.
- Sanitation of chronic foci of infection.
- Avoid contact with known allergens.
- Eliminate unjustified use of medications and vaccinations.
- Lead a healthy lifestyle (do not drink alcohol, do not smoke).
- Eat right – more fruits, vegetables, proteins (exclude salty, fatty and fried foods).
- Play sports – swimming, running, walking, etc.
- Do not overcool or overheat, as this all negatively affects the state of the immune system and worsens the properties of the skin.
 [ 39 ]
[ 39 ]

