Medical expert of the article
New publications
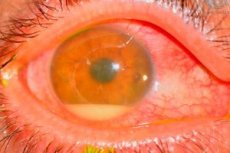
Acute postoperative endophthalmitis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Causes postoperative endophthalmitis
The causative agents are most often coagulase-negative staphylococci (eg, Staph. epidemidis), gram-positive (eg, Staph. aureus) and gram-negative (eg, Pseudomonas sp., Proteus sp.) microorganisms.
The source of infection is difficult to identify. The most common culprit is considered to be the patient's own bacterial flora of the eyelids, conjunctiva and lacrimal canals. Other potential sources of infection include contaminated solutions, instruments, the environment, including operating room personnel.
Symptoms postoperative endophthalmitis
The severity of endophthalmitis depends on the virulence of the pathogen.
- Extremely severe is characterized by pain, significant visual impairment, eyelid edema, chemosis, conjunctival injection, hyoid secretion, corneal infiltrates, and large hypopyon.
- Moderate severity is characterized by the loss of fibrinous exudate into the anterior chamber, lesser hypopyon, vitreitis, absence of fundus reflex and impossibility of ophthalmoscopy even in indirect light.
- The mild form may be accompanied by only minor pain, absence or slight hypopyon and preservation of some fundus reflex with the possibility of partial ophthalmoscopy with an indirect ophthalmoscope.
Determining the time interval from surgery to the development of endophthalmitis symptoms may be helpful in suggesting the causative agent. For example, Staph. aureus and gram-positive bacteria are usually present 2–4 days after surgery with severe endophthalmitis. Staph. epidermidis and coagulase-negative cocci usually appear 5–7 days after surgery with less severe symptoms.
Diagnostics postoperative endophthalmitis
- Detection of the pathogen in the aqueous humor or vitreous body confirms the diagnosis. However, a negative reaction does not exclude the presence of infection. Sampling in the operating room consists of the following:
- a 0.1 ml sample of aqueous humor is taken by aspiration with a needle on a tuberculin syringe from the existing second incision;
- The vitreous sample is best taken with a mini-vitrector through the pars plana 3.5 mm from the limbus. If a mini-vitrector is not available, an alternative is a partial sclerotomy 3.5 mm from the limbus with aspiration of the liquid vitreous from the mid-vitreous cavity using a needle on a tuberculin syringe. Vitreous in a volume of 0.1-0.3 ml is added to blood agar, liquid thioglucolate and Sabourand agar. If ready-made media are not available, a good alternative is to place the sample in special ready-made blood sample plates. A few drops are also placed on glass with Gram or Giemsa stain.
- Vitrectomy is indicated only in the case of an acute infectious process and a decrease in vision to light perception. With higher visual acuity (from hand movements and above), vitrectomy is not necessary.
- The antibiotics of choice are amikacin and ceftazidine, which are sensitive to most gram-positive and gram-negative bacteria, and vancomycin, which is sensitive to coagulase-negative and coagulase-positive cocci. Amikacin is synergistic with vancomycin, but is potentially more retinotoxic than ceftazidine and does not synergize with vancomycin.
- Intravitreal antibiotic administration begins immediately after the pathogen type has been identified and the density of the eyeball has decreased. Amikacin (0.4 mg in 0.1 ml) or ceftazidine (2.0 mg in 0.1 ml) and vancomycin (1 mg in 1.0 ml) are slowly injected into the midvitreal cavity using a needle. The bevel of the needle should be directed anteriorly to ensure minimal contact of the drug with the macula. After the first injection, the syringe should be disconnected and the needle left in the cavity to administer the second injection. If the likelihood of precipitate formation is high, two different needles with different antibiotics should be used. After the needle is withdrawn, a parabulbar injection of the antibiotic is administered;
- parabulbar injections of vancomycin 25 mg and ceftazidine 100 mg or gentamicin 20 mg and cefuroxime 125 mg allow therapeutic concentrations to be achieved. They are prescribed daily for 5-7 days, depending on the condition;
- local therapy is used sparingly, except in cases accompanied by infectious keratitis;
- Systemic therapy is questionable. The Endophthalmitis Vitrectomy Study Group showed that the general administration of ceftazidine and amikacin is ineffective. These antibiotics, being water-soluble, have weak activity against gram-positive bacteria and low permeability for the organ of vision. Perhaps other antibiotics, such as lipid-soluble quinolones (eg, ciprofloxacin, ofloxacin) and imepenem, which have better permeability and a broad antimicrobial spectrum, are more effective. The answer to this question remains to be obtained in the course of future studies.
- Steroid therapy is given after antibiotics to reduce inflammation. Steroids are less dangerous only if the bacteria are sensitive to the antibiotic.
- parabulbar betamethasone 4 mg or dexamethasone 4 mg (1 ml) daily for 5-7 days depending on the condition;
- orally prednisolone 20 mg 4 times a day for 10-14 days in severe cases;
- locally dexamethasone 0.1%, initially every 30 minutes, then less often.
- Further therapy and its extent are determined depending on the isolated bacterial culture and the clinical picture.
- Signs of improvement include a weakening of the cellular reaction and a decrease in hypopyon and fibrinous exudate in the anterior chamber. In this situation, treatment does not change regardless of the test results.
- If resistant bacterial cultures are isolated and the clinical picture worsens, antibiotic therapy should be changed.
- Treatment results are poor despite vigorous and correct therapy (in 55% of cases the achieved visual acuity is 6/60 or lower).
In some cases, decreased vision may be associated with retinotoxicity of antibiotics, especially aminoglycosides. FAG shows hypofluorescence due to ischemia.
What do need to examine?
Differential diagnosis
- Residual lens material in the anterior chamber or vitreous body can cause acute anterior uveitis.
- A toxic reaction may occur to the irrigation fluid or foreign materials used during surgery. Less commonly, a pronounced fibrinous film develops on the anterior surface of the intraocular lens. In this case, high doses of steroids (locally or parabulbarly) in combination with cycloplastics are effective, but synechiae with the intraocular lens may develop.
- Complex or prolonged surgery leads to corneal edema and uveitis, which are detected immediately in the postoperative period.
Who to contact?
Prevention
Optimal prevention has not yet been determined. However, the following measures may be helpful.
- Preoperative treatment of existing infections such as staphylococcal blepharitis, conjunctivitis, dacryocystitis, and in individuals with prostheses, sanitation of the contralateral cavity.
- Instillation of povidone-iodine before surgery:
- A commercially available 10% betadine solution used for skin preparation is diluted with saline to obtain a 5% concentration;
- Two drops of the diluted solution are injected into the conjunctival sac a few minutes before the operation, and gentle manipulations help distribute the solution over the surface of the eye. This solution can be used to treat the eyelids before applying the eyelid speculum;
- Before the operation, the eyeball is irrigated with saline solution.
- Careful placement of the eyelid speculum, which involves isolating the eyelashes and eyelid margins.
- Prophylactic administration of antibiotics
- Postoperative administration of antibiotics into the sub-Tenon space is widely used, but evidence of the effectiveness of the method is insufficient;
- Intraoperative irrigation of the anterior chamber with the addition of antibiotics (vancomycin) to the infusion solution may be an effective measure, but at the same time contribute to the emergence of resistant strains of bacteria.


 [
[