Medical expert of the article
New publications
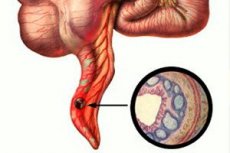
Acute phlegmonous appendicitis: purulent, ulcerative, gangrenous
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Epidemiology
- Women are more likely to suffer from the disease at the age of 15-40, men – 12-20;
- Men suffer from the disease much less often, but women have a much better prognosis and a lower risk of developing complications.
- Phlegmonous appendicitis is least often diagnosed in infants under one year of age and in the elderly.
- After age fifty, the risk of developing appendicitis decreases to 2 percent;
- Removal of the appendix accounts for 80% of all simple operations performed.
Causes phlegmonous appendicitis
The etiology of the disease has not been definitively established.
There are a few reasons for the occurrence of phlegmonous appendicitis:
- Thrombosis of the vessels of the appendix, and as a consequence ischemia of its tissues. Because of this, such a function of the lymphoid tissue as protective is reduced, inflammation occurs and the activity of opportunistic flora inside the intestine increases.
- Also, the cause of phlegmonous appendicitis may be the occurrence of complications of the catarrhal form of the disease.
- Mechanical obturation of the appendix.
Risk factors
The greatest risk for the development of phlegmonous appendicitis is the age from twenty to thirty years. Although the disease can also occur at absolutely any age.
Most often, risk factors are:
- endocrine - the presence in the appendix of the cecum (its mucous membrane) of many cells that produce the hormone serotonin.
- casuistic – the presence of foreign bodies (for example, grape seeds, seed peels, fish scales) in the human intestine.
- food - when a person eats mainly meat products or food rich in animal proteins.
Pathogenesis
The enterogenous route of infection most often becomes the cause of the disease. At the same time, the hematogenous and lyphogenous routes practically do not play a decisive role in the pathogenesis of the disease.
Various microorganisms that are in the appendix (protozoa, viruses and bacteria) are the cause of inflammation. Basically, this is the anaerobic form of flora (anaerobic cocci), less often - aerobic (enterococci, E. coli).
Symptoms phlegmonous appendicitis
The manifestation of phlegmonous appendicitis is quite pronounced:
- The first sign will be a sharp pain, most likely of unclear localization, increasing with movement. Then the pain will increase and take on a more precise location.
Other symptoms will include:
- general intoxication of the body and lethargy,
- grayish or white coating on the tongue,
- lack of appetite,
- nausea, possible vomiting,
- bloating, diarrhea or, conversely, constipation,
- headache and slight fever.
When examining a patient, a health professional will identify the following signs:
- at the site of pain, tension in the abdominal muscle tissue will be noted;
- affirmative symptoms of "sliding" and irritation of the peritoneum.
Where does it hurt?
Forms
There are several varieties of phlegmonous appendicitis:
- acute phlegmonous appendicitis – occurs in a very short period of time (several hours). Characterized by an acute onset of inflammation, with changes of a purulent rather than destructive nature.
- Phlegmonous-ulcerative appendicitis - against the background of the development of damage to the mucous membrane of the appendix by ulcerative processes, purulent inflammation occurs.
- The purulent stage of phlegmonous appendicitis is the "rise" of body temperature, further development of intoxication processes, increased pain intensity - all this indicates the occurrence of localized purulent foci on the walls of the appendix. The reason will be the continued development of microorganisms.
- Phlegmonous appendicitis in a child is manifested by purulent inflammation of the entire appendix. Macroscopic examination shows that it is thickened, completely covered with fibrin, intensely red. Microscopically, infiltration of all layers of the appendix is noticeable, there are signs of suppuration and slight rejection in the mucous membrane.
Complications and consequences
Phlegmonous appendicitis can have very unfavorable consequences if you do not seek medical help in a timely manner. These are:
- intestinal obstruction;
- the appearance of an appendicular mass or abscess;
- inflammation of the venous wall of the iliac or pelvic veins;
- thrombosis;
- peritonitis, resulting from a ruptured appendix;
- purulent inflammation of the veins of the liver;
- sepsis;
- multiple organ failure;
- fatal outcome.
Diagnostics phlegmonous appendicitis
Examination of the abdominal organs and radiography will not be able to detect inflammation in the appendix of the cecum.
X-ray examination will only help to clarify the differentiation of appendicitis from a perforated ulcer of the stomach or duodenum.
In this case, ultrasound diagnostics of the gastrointestinal tract can be used to distinguish phlegmonous appendicitis from inflammation in the gallbladder or urinary bladder.
What do need to examine?
How to examine?
Differential diagnosis
This type of research is carried out for the correct diagnosis of a whole group of diseases.
Cholecystitis. A tense hypochondrium on the right side, pain "radiating" to the shoulder blade or shoulder, the patient's history of signs of gallstone disease earlier, as well as the results of an ultrasound examination, will indicate acute inflammation of the gallbladder and help to correctly differentiate it from appendicitis. Often, the gallbladder, increasing in size, descends very low (sometimes even below the navel area), and pain is felt throughout the right half of the abdomen. Or the appendix, becoming inflamed and located under the liver, can stimulate the development of acute cholecystitis. Therefore, it can be very difficult to make a diagnosis without additional studies.
Pleuropneumonia or inflammation of the right lower lobe of the lungs. To distinguish this pathology from appendicitis, you need to listen to the lungs. In this case, you will hear weak breathing and wheezing. And with pleuropneumonia, you will also hear how the pleura rubs when breathing. If there is an accumulation of fluid from the blood vessels in the right cavity, you will hear a dullness of the percussion tone, a decrease in respiratory noise. Also with this disease, there may be a cough, fever and pain radiating to the right half of the abdomen.
Mesadenitis. Due to the localization of pain on the right iliac side, it is possible to disorient the medical specialist. But the presence in the anamnesis of a recent upper respiratory tract disease, and a combination with enlarged lymph nodes, and in six percent also with yersiniosis, will leave no doubt about the diagnosis.
Inflammation of Meckel's diverticulum ( diverticulitis ). Just like phlegmonous appendicitis, it requires urgent hospitalization and surgical intervention. The disease is rarely diagnosed before surgery and laparoscopy, which is done to establish a diagnosis. To establish a diagnosis, it is necessary to perform an intraoperative revision of 100 cm of the ileal region of the intestine.
Acute pancreatitis. Similar to appendicitis by the Shchetkin-Blumberg symptom. Very often there is repeated vomiting. The abdomen is slightly swollen in the upper sections. The patient feels poorly, but the temperature is almost not elevated. The tests show an elevated level of digestive enzyme in the urine.
Acute intestinal obstruction. It can be quite difficult to diagnose, especially with a neoplasm in the colon. The presence of cramping pain, increased peristaltic noise, constipation and flatulence will help to do this. Kloiber's "cups" are clearly visible on the X-ray.
Crohn's disease. Characterized by severe pain in the lower abdomen. Rarely, diarrhea and leukocytosis may occur. On the right side, a formation that hurts is clearly palpable. Basically, the diagnosis is made during an appendectomy, due to the mistaken assumption of the disease for acute appendicitis. In order for the diagnosis to be made correctly, laparoscopy will help medical workers. Also, before revision in the abdominal cavity, it is necessary to pay attention to changes in the appendix. If it is not the same as it was before surgery, attention should be paid to the ileal part of the intestine.
Acute gastroenterocolitis. Characterized by pain of a spastic, diffuse nature. The patient complains of nausea, vomiting, diarrhea and false urge to defecate. Bloating and rumbling of the abdomen are often noted. Appendicular symptoms will not be characteristic here.
Renal colic on the right side. Frequent urination is typical. When taking urine samples, macro- or microhematuria is revealed. There may also be abdominal distension. The main symptom will be Pasternatsky's symptom, since it is not mandatory for appendicitis (except for cases of retrocecal location of the appendix). If there are doubts about the diagnosis, an X-ray examination of the urinary tract should be performed. Most likely, the presence of "stones" in the right ureter and signs of pyeloexcretion will be detected. And "tapping" in the lumbar region will help to make an absolutely accurate diagnosis. You can also perform a novocaine blockade in the right spermatic cord or uterus. With renal colic, the pain will quickly subside, and with appendicitis it will remain.
Treatment phlegmonous appendicitis
If a diagnosis of phlegmonous appendicitis is made, surgical treatment should be performed immediately.
The intervention is performed under general anesthesia. If there are no contraindications, it is performed using endotracheal anesthesia. This type of anesthesia does not limit the surgeon's movement and makes it possible, if necessary, to perform a wide resection of the abdominal cavity. If the patient has an individual intolerance, local anesthesia may be used.
Most often, traditional appendectomy or laparoscopy is used.
Laparoscopy
Used if:
- there is no inflammatory process in the cecum;
- there are no adhesions on the intestines;
- no complications in the form of peritonitis, inflammatory infiltrate or retroperitoneal phlegmon.
Contraindications for its implementation will be: pregnancy in the third trimester, obesity, increased bleeding, and also if the appendix is located atypically.
Appendectomy is performed under general anesthesia.
Stages of the operation:
- It is necessary to make three punctures on the abdominal wall (5 to 10 cm long), so that one of them is on the navel.
- Insert a video camera and special instruments to remove the appendix.
- Conduct an intervention.
This type of surgery allows to reduce the patient's hospital stay, reduces the intensity of pain in the postoperative period, there is a faster recovery of the intestine, and the scar has a cosmetic appearance.
Appendectomy routine
Stages of intervention:
- The surgical field is treated and covered with sterile gauze pads.
- The surgeon makes an oblique skin incision (10-12 cm long) in the right iliac region.
- After cutting the subcutaneous fat, the doctor, using a scalpel and special surgical scissors, cuts the tendon of the oblique abdominal muscle. After this, the muscle is cut in the upper corner of the wound surface and the peritoneum is opened using blunt hooks.
- The wound is dried with a napkin. To identify bacterial flora, an analysis is required.
- Next, the doctor finds the cecum and removes it into the wound cavity. Adhesions, if any, are cut. In order to carefully examine the lateral canal and the iliac fossa, the loops of the small intestine should be moved away if they interfere. This is easy to do, since the appendix will most likely be located on the dome of the cecum. The surgeon, taking into account that he needs to fix the distal part of the appendix, passes a ligature under it and lowers the top into the abdominal cavity.
- A ligature is applied to the mesentery of the appendix so that the artery of the vermiform appendix is tied. To avoid thread slippage, if the mesentery is loose, the ligature is stitched.
- Then the peritoneal fold is necessarily cut off. The appendix is clamped at the base and tied.
- Using an atraumatic needle, the doctor, having previously retreated 1.5 cm, performs a circular suture.
- 0.5 cm from the suture, the clamp is applied again and the appendix is cut off.
- The operating doctor's assistant treats the stump with iodine solution and, having grasped it with special tweezers, inserts it into a circular suture. The surgeon tightens it.
- Before replacing the dome, a Z-suture must be made again and the apex of the cecum must be returned to the peritoneal cavity.
- The surgeon needs to stop the bleeding by drying the cavity with a napkin from the formed exudate.
- The wound is flushed with saline solution to eliminate the possibility of complications due to tissue residue, blood or infected effusion.
- The doctor sews up the muscles with 2-3 stitches. Then, using synthetic threads, he sews up the external aponeurosis of the oblique muscle.
This type of operation is characterized by a long postoperative rehabilitation period.
Retrograde appendectomy
It is performed in cases where it is not possible to isolate the appendix into the wound cavity. Its difference from a regular appendectomy is that in this case the mesentery is not cut off immediately and, while maintaining its blood supply, the stump is treated, and after the appendix is removed.
Features of performing surgery for phlegmonous appendicitis:
- Due to inflammation of the mucous membrane of the appendix, there is a possibility of effusion in the right air space. Therefore, the doctor must dry the pit, the right lateral canal and the pelvic cavity, be sure to take exudate for analysis. If it is cloudy, antibiotics must be administered in parallel.
- When the surgeon has doubts about the complete removal of the inflamed - phlegmonous appendix, mandatory drainage installation for three to four days will be required.
- In case of complications in the form of perforation, appendectomy is performed with absolute access, thereby facilitating the sanitation and removal of pathological tissues.
Postoperative period
To reduce the risk of postoperative complications, the patient should follow a gentle regime. Thus, getting out of bed after surgery is possible no earlier than six to eight hours later, but only if consciousness and breathing are fully restored.
Patients at risk of developing a postoperative hernia may need to wear a special postoperative bandage.
The patient needs to have dressings done every day, necessarily assessing the stage of wound healing and using antiseptics. Depending on the intensity of the pain, painkillers are used.
In cases where there was a need to use drainage to prevent purulent complications, the administration of antibacterial drugs from the cephalosporin or macrolide class is required in the postoperative period.
The stitches are removed seven to eight days after the operation if wound healing is not complicated.
After surgery for phlegmonous appendicitis, heavy physical activity is not recommended for about three months. The doctor may prescribe only exercise therapy or breathing exercises.
Diet after surgery for phlegmonous appendicitis
For two to four weeks after the operation and discharge from the hospital, to prevent constipation, you need to follow a diet. You can only eat foods that are recommended by the doctor.
The first two days you should eat only liquid porridge and vegetable puree. You should also add jelly or low-fat kefir to your diet. Then gradually introduce black bread with a small amount of butter. The transition to regular, familiar food for the patient can only be done if you feel excellent and have normal bowel movements. But do not forget that the food should not be spicy, pickled, smoked, fatty, fried or hard. Also, you should exclude coffee and strong tea, soda, and baked goods from rich dough from your diet. All food is prepared by baking or boiling.
You need to eat small portions, about five to six times a day.
More information of the treatment
Forecast
If treatment is started promptly, the prognosis is favorable. Mortality is no more than 0.03%, and the risk of complications, most often peritonitis in weakened people, is no more than 9%. Quite often, inflammation of the peritoneum occurs, but it is quickly limited to the omentum or the walls of adjacent internal organs.
Rarely, an infiltrate may form, after which, after some time, adhesions will form.


 [
[