Medical expert of the article
New publications
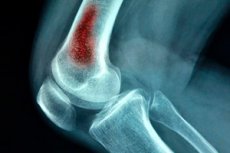
Acute hematogenous osteomyelitis
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
One of the most life-threatening variants of surgical infection is acute hematogenous osteomyelitis. This pathology predominantly occurs in children, although adults can also become ill as a result of traumatic injuries (gunshot wounds, postoperative complications, etc.). The pathology is a purulent intraosseous process caused by the infectious agent entering the bloodstream. [1]
Epidemiology
In purulent hematogenous osteomyelitis, there is a purulent inflammatory process in the bone. It involves medullary structures, periosteum and compact bone tissue. Sometimes the disease becomes a consequence of the spread of purulent reaction to bone tissue from nearby organs and tissues. Such a development is characteristic of odontogenic osteomyelitis caused by dental caries, for rib osteomyelitis associated with pleural empyema, for phalangeal osteomyelitis caused by panaricia, etc.
In the vast majority of cases, the causative agent is Staphylococcus aureus, or its combinations with other pathogens - in particular, with Proteus or Pseudomonas bacillus.
Acute hematogenous osteomyelitis is considered a predominantly pediatric pathology. The main percentage of patients (more than 95%) are children of preschool and primary school age. The reason for this selectivity is simple and is related to the age-related anatomical features of bone trophicity and structure, namely:
- The strong development of the blood vascular network;
- Blood supplying epiphyseal, metaphyseal and diaphyseal autonomy;
- A large number of small vascular branchings running along the radial pathway through the epiphyseal cartilage to the ossification nucleus.
The metaphyseal circulatory network is formed in children over 2 years of age, and until then the epiphyseal network is predominant. These networks exist separately from each other, but are connected by means of anastomoses. The formation of a common vascular system occurs as the epiphyseal growth area ossifies. In patients 2-3 years of age, the metaepiphyseal areas are affected, while at older ages the problem affects mainly the diaphysis.
Acute hematogenous osteomyelitis is diagnosed more often in children 7-15 years old, in boys - three times more often than in girls. An adult can also get sick, but it is much less common.
The development of pathology in newborns is often associated with infection of the umbilical wound. [2]
Causes of the acute hematogenous osteomyelitis.
The common cause of the formation of such a serious pathology as acute hematogenous osteomyelitis is the penetration of pathogens inside the bone marrow, which give rise to the development of a purulent reaction. Foci of infection, from which pathogens spread through the bloodstream and get into the bone, can become otitis media, tonsillitis (purulent), furunculosis, suppurative wounds. And the pathology does not occur immediately after the primary infection: months and even years may pass.
The main causative agent of acute hematogenous osteomyelitis is Staphylococcus aureus: it is found in about eight out of ten patients. In some cases, it is a combined infection, including Proteus and Synegnaeus bacillus.
The intensity of the inflammatory process is largely related to the peculiarities of the bone structure. The inflammatory reaction develops in a medullary structure surrounded by a rigid environment of denser cortical walls. Under such circumstances, there is no possibility of reducing tissue pressure by expanding the inflamed area, so the reaction unrestrainedly spreads beyond the boundaries of the primary zone through the vascular network and Haversian canals.
From the moment of pathologic focus formation, osteomyelitis can be considered as a potentially septic process that includes the stages of presepsis and sepsis. [3]
Risk factors
The vast majority of cases of acute hematogenous osteomyelitis occur in children and adolescents and in general in patients with weak immune defenses. Risk groups include the following categories:
- Preschoolers and elementary school children;
- Elderly persons (over sixty years of age);
- Patients with congenital or acquired immunodeficiency conditions;
- Patients with septic conditions;
- Cancer patients;
- Patients suffering from chronic infectious-inflammatory pathologies.
Any internal sources of bacterial invasion can be classified as provoking factors. This can be dental caries, tonsillitis (especially purulent), undrained foci of inflammation, as well as various premorbid conditions. An important role is played by the allergic disposition of the body, a drop in immunity as a result of simultaneous introduction of several prophylactic vaccines, as well as trauma, hypothermia, stressful situations. [4]
Pathogenesis
The pathogenetic mechanism of acute hematogenous osteomyelitis formation has not been sufficiently studied to date. Presumably, the basic factors of pathogenesis are:
- The presence of an infectious agent in the body;
- Individual bone anatomy;
- Severe immune compromise.
A feature of the inflammatory response in acute hematogenous osteomyelitis is its confinement in the hard tube of the bone, which entails severe compression of the vascular network. The pain syndrome becomes the result of increased pressure within the medullary space. The indicator of hypertension can be up to 300-500 mm Hg (the norm for a healthy child is from 60 to 100 mm Hg).
If the pathology is not detected at the stage of the inflammatory process within the bone marrow canal, then on the fourth or fifth day from the start of osteomyelitis, purulent masses begin to spread through the Haversian and Volkmannian system to the periosteum, as a result of which it gradually delaminates.
By the eighth or tenth day, purulent masses together with decay products continue to delaminate the periosteum, after which there is a breakthrough of pus into soft tissue structures. This leads to the formation of intermuscular and subcutaneous phlegmon. This situation is said to be a neglected disease: therapy of late diagnosed acute hematogenous osteomyelitis is complex and long.
Pain syndrome in most cases subsides against the background of spontaneous breakthrough of the subperiosteal abscess into nearby structures, which is accompanied by a sharp decrease in pressure inside the medullary space. [5]
Symptoms of the acute hematogenous osteomyelitis.
Symptomatology depends to some extent on the form of the pathological process, which can be localized and generalized.
In the localized form, the pain is severe, tumescent, and concentrated in the area of the affected bone. Touching or tapping on the limb causes extremely unpleasant sensations, motor activity is sharply limited, the skin over the area of inflammation is hot, reddish, often edematous.
In the generalized form, local manifestations are combined with general. Signs of intoxication increase, temperature rises, chills and excessive sweating occur. With further spread of purulent foci, the situation is markedly worsened. Multiple bone lesions, the development of purulent pericarditis or purulent destructive pneumonia are possible.
In the local course of acute hematogenous osteomyelitis, local signs dominate, but are not the only ones: symptoms of intoxication are present in any case. In the course of interviewing the patient, there are necessarily present complaints of unsatisfactory general condition, chills, fever. Externally, attention is drawn to the swelling of the skin, its pallor or redness, visible vasculature. Palpatorially, a growing painful area is detected, when attempting percussion, the pain becomes especially bright. [6]
First signs
Acute hematogenous osteomyelitis starts suddenly, often - after trauma (even a small), or another provoking factor (eg, hypothermia).
The main and persistent sign of pathology is bone pain, spreading, from aching to particularly intense. Pain prevents a person from sleeping, makes him irritable, nervous. As a rule, extremely unpleasant sensations spread to the entire affected limb, but the focus of pain can often be unmistakably identified. Such a pain syndrome is due to intraosseous pressure increase against the background of the growing inflammatory process in the bone. It is noteworthy that bone pain is characterized by constancy.
The next main sign in acute osteomyelitis is a high temperature. At the initial pathological stage, the indicators may be in the range of 37-38 ° C, but with the development of generalized osteomyelitis, the temperature rises sharply and steadily to 39-41 ° C, sometimes accompanied by fever. Simultaneously with generalized hyperthermia there is a local increase in temperature in the area of the lesion.
The third initial sign of the disease is a functional disorder of the affected limb. The patient begins to limp, motor activity is sharply limited to the point of complete impossibility. Even a slight movement of the affected limb causes severe pain, which forces a person to find a forced position with the maximum possible muscle relaxation. In particular, when the hip is affected, the patient prefers to bend the leg in both the hip and knee joints: the limb is slightly turned outward. If this position persists for a long time, a flexion joint contracture may form.
Then, about 48-96 hours from the onset of acute osteomyelitis, the affected limb swells. Over time, edema spreads to other tissues. The skin over the pathologic focus becomes tense, dense. Severely affects the general well-being. Severe course of pathology can be accompanied by the spread of the disease process to other bones.
Local symptoms of acute hematogenous osteomyelitis
Acute hematogenous osteomyelitis starts with a sharp rise in temperature. Simultaneously, pain appears in the area of the pathological focus. The diseased limb loses the ability to move, the patient tries to give it a forced position. The limited area swells, the skin acquires pastosity, a local increase in temperature is noted when palpating. In a short time, the swollen area turns red, fluctuation is noted.
Microosteoperforation confirms the presence of intraosseous increased pressure, which allows the diagnosis to be established even in the absence of purulent masses in the bone marrow cavity or under the periosteum. In some situations, it is appropriate to perform a diagnostic bone puncture with further cytology of the obtained material.
Blood tests demonstrate leukocytosis and a leftward shift of the formula, as well as toxic neutrophil granularity. The erythrocyte sedimentation rate is significantly increased, and this increase is stable. The protein spectrum of blood is also changed: there is dysproteinemia, increased globulin fractions, hypoalbuminemia. Prolonged osteomyelitis is accompanied by anemia associated with cerebrospinal toxic depression.
The nature of pain in acute hematogenous osteomyelitis
Pain in acute hematogenous osteomyelitis:
- Strong;
- Tumescent;
- Intensified by palpation and tapping on the pathologic area;
- After a while become extremely sharp, unbearable, with instantaneous aggravation at the slightest movement.
Because of the severe pain syndrome, the patient assumes a forced position, he can neither eat nor sleep, becomes irritable. If no help is rendered, there is a possibility of mental confusion, delirium and hallucinations.
Classification
Depending on the course, acute and chronic osteomyelitis are distinguished.
The mechanism of pathology development is also reflected in the classification:
- Endogenous osteomyelitis (hematogenous);
- Exogenous (as a result of trauma, surgical intervention, gunshot wound, etc.);
- Neurogenic (contact-compression).
Depending on the clinical stage, differentiate between:
- Acute osteomyelitis (lasts up to 14-21 days);
- Subacute (up to 22-28 days);
- Chronic (more than 28 days).
Atypical forms of the disease are represented by Brody abscess, albuminous osteomyelitis Ollier, sclerosing osteomyelitis Garre.
According to the clinical picture, acute hematogenous osteomyelitis goes through such stages:
- The patient's well-being deteriorates, loss of appetite, unexplained apathy.
- There is insomnia, fever, possible phenomena of dyspepsia.
- After about 24 hours, the temperature reaches high levels (about 39°C).
- Intoxication increases, the skin becomes pale to bluish. Pain is pronounced, acute, active movements are absent, passive movements are severely limited.
When the pathological focus breaks through, the skin becomes hyperemic, the patient's condition improves somewhat. The formation of multiple bone foci is possible - approximately 1-2 weeks after the primary focus appears.
Forms
According to the area of localization of the pathological focus of acute purulent hematogenous osteomyelitis is epiphyseal, metaphyseal, diaphyseal, with lesions of spongy, flat and short bones. Symptomatology and peculiarities of therapy of the pathological process depend on both the age and general state of health of the patient, and on the location of the inflammation zone. Metaphyses and diaphyses of long tubular bones are affected mainly in preschool and junior school age. The picture of pathology is multifaceted and closely related to such factors as the state of immunity and virulence of the pathogenic microorganism.
Local form of acute hematogenous osteomyelitis is not "pure", as it combines both local and general manifestations, although local signs are somewhat dominant. There is a bright rasping pain in the area of the bone, draws attention to the intense swelling (the skin is swollen, tense). When tapping, the patient demonstrates a clear pain response. In the local form, motor ability may be preserved for some time.
The pathology predominantly affects long tubular bones. Flat and short bones are much less frequently affected. In most cases, the bones are affected:
- Femur (up to 40% of cases);
- Tibia (about 30% of cases);
- Humerus (about 10%).
Much less frequently, the problem is found in the bones of the foot, pelvis, and upper jaw.
Acute hematogenous osteomyelitis of the long tubular bones has a different distribution. Thus, we can talk about the following variants of the disease:
- Metadiaphyseal acute hematogenous osteomyelitis - affects the metaphysis and more than 50% of the diaphysis;
- Metaepiphyseal acute hematogenous osteomyelitis - affects the metaphysis and most of the epiphysis;
- Metaphyseal osteomyelitis - extends to the edge of the epiphysis or diaphysis;
- Total osteomyelitis - affects the diaphysis and both metaphyses.
Septicopiemic form of acute hematogenous osteomyelitis is a particularly common variant of the disease, manifested by the acute development of sepsis. In some patients, a small prodromal interval is noted, characterized by a feeling of fatigue, weakness, pain in the head. The temperature rises to 39°C, with significant daily fluctuations of 1.5-2°C. Pain in the area of the lesion appears a couple of hours after the start of the pathological process. The pain syndrome has a rasping character, is characterized by high intensity, the patient can neither eat nor sleep, is constantly in a forced position, avoiding in every possible way any touch to the affected limb. General well-being is extremely poor, there are clear signs of severe intoxication. Local manifestations are detected gradually, pain is localized only by the second day, but the reaction to touch is present almost immediately. Swelling and local picture become distinct only on the third or fourth day. If medical attention is not rendered, the area of edema is supplemented by redness and fluctuation. This form is often accompanied by metastasis of the purulent-infectious process, with the formation of purulent foci in other tissues and organs (bone structures, lungs, kidneys, liver).
The toxic form of acute hematogenous osteomyelitis (other names - lightning, adynamic) is characterized by the most severe course, with dominant general toxic manifestations. Pathology develops rapidly, hyperthermia is sharp, quickly reaching high values of 40-41 ° C. There is a particular severity of the condition, possible disturbance of consciousness, delusional-hallucinatory episodes. Cardiac activity is affected: there is tachycardia, weak filling of the pulse, muffled heart tones. Due to the atypicality of symptomatology, this form is often difficult to diagnose. The condition of the patient is very severe, which in many cases makes it impossible to determine the primary inflammatory focus.
Complications and consequences
Complications of acute hematogenous osteomyelitis are local and general.
Among the local ones, the most common are:
- Deformities, bone defects;
- Pathologic fractures;
- The formation of false joints;
- Ankylosis;
- Purulent arthritis, phlegmons;
- Osteomyelitic ulcers;
- Fistula wall malignancy.
Possible common complications:
- Septic conditions;
- Renal amyloidosis;
- Dystrophy of the internal organs.
The most frequent complication is sepsis: its development is noted in case of delayed or incorrect treatment measures.
The occurrence of purulent arthritis is due to the spread of the infectious agent from the affected bone through the lymphatic system, or with purulent breakthrough into the joint cavity.
Pathological bone fracture occurs due to the destruction of the affected bone. In this case, a false joint is sometimes formed - a pathology that is characterized by a stable disruption of the continuity and mobility of the bone element, which is not specific to a particular department.
Epiphyseal and metaphyseal hematogenous pathology can cause growth disturbance and severe distortion (shortening) of the bone, which is due to the direct location of the focus near the growth zone. [7]
Diagnostics of the acute hematogenous osteomyelitis.
Diagnostic measures begin with the collection of complaints and anamnesis.
The patient complains of fever, pain in the affected bone, impaired motor function. In the anamnesis, there may be an indication of trauma, surgical interventions, as well as the presence of other infectious foci in the body.
In the course of physical examination, one notices increased pain on palpation and percussion, increased temperature, hyperemia and edema in the area of the projection of the pathological focus.
The tests demonstrate the presence of an inflammatory process in the body: in the blood there is a leukocytosis with a shift to the left, as well as an increase in the sedimentation rate of erythrocytes. Protein, erythrocytes and cylinders are present in the urine.
Instrumental diagnostics is represented by the following investigations:
- Radiography - defines a picture typical of acute hematogenous osteomyelitis. It includes: a blurred image of the bone, fibrillation of bone crossbars, and subsequently - alternating zones of bone thinning and thickening, periosteal thickening. Radiologic signs of acute hematogenous osteomyelitis are detected gradually, within 2-3 weeks from the onset of the disease. At first, periosteum detachment with manifestations of periostitis is detected. Next, areas of sparse tissue are formed in the metaphysis zone. After 8-16 weeks, sequestrations and cavities are formed.
- Radiological diagnosis of acute hematogenous osteomyelitis can be supplemented by fistulography with contrast. Thanks to the study, the degree of filling of bone cavities and surrounding soft tissue structures with contrast agent is revealed.
- Ultrasound helps to assess the degree of spread of the inflammatory reaction in the soft tissues, detect sequestrations and paraosseous purulent foci.
- Angiography is used to identify avascular bone segments and to rule out phlebothrombosis.
A separate bacteriologic study is performed to identify the causative agent. The majority of patients are isolated with Staphylococcus aureus, somewhat less frequently with Pseudomonas bacillus or Proteus, even less frequently with Enterobacteriaceae or anaerobes. [8]
Differential diagnosis
Differential diagnosis is made between hematogenous and posttraumatic osteomyelitis.
|
Hematogenous inflammation |
Post-traumatic inflammation | |
|
They get sick more often |
Pediatric and adolescent patients |
Mostly adult patients |
|
Type of infection |
Endogenous-hematogenic |
Exogenous |
|
Etiologic factor |
Hematogenous infection |
Trauma combined with infection |
|
Dominant pathogen |
Staphylococcus aureus |
Cocci, Escherichia coli or Pseudomonas, Proteus, mixed infection |
|
Reactive state |
A sharp increase in the body's reactivity |
Normal body reactivity |
|
Morphological factor |
Primary osteomyelitis |
Secondary purulent ostitis |
|
Sequestration |
True sequestrations occur throughout the pathologic process |
Pseudosequestrians arise first, true ones later on |
|
Fracture |
It's rare |
Present as an underlying pathology |
|
Infection of the joint |
It's a fairly common occurrence |
Rarely, only in cases of intra-articular fracture |
|
Septic complications |
Often |
Rarely |
Who to contact?
Treatment of the acute hematogenous osteomyelitis.
Therapeutic measures are urgent and complex, they involve the earliest possible effect on the causative agent, avoid septic complications and limit the local focus of infection. It is important to relieve intoxication as soon as possible, minimize the load on vital organs, optimize the protective potential of the patient and prepare him for the upcoming surgical intervention. [9]
First of all, it is necessary to normalize body temperature and prevent the development of toxemia, which is especially important in children. Use physical methods of cooling, medically dilate peripheral vessels (Drotaverine, Papaverine) and reduce the temperature (administer 4% amidopyrine in the amount of 0.1 ml/kg, 50% analgin in the amount of 0.1 ml per year of life of the baby). Homeostasis is corrected by intravenous infusion to eliminate hypovolemia and stabilize water-salt and acid-base balance.
Infusion therapy is started with the administration of glucose solution and medium and low molecular weight polymers with detoxification ability (Reopolyglukin, Hemodez, etc.), as well as protein solutions (native plasma, albumin, blood). Fluid volumes are replenished with electrolyte solutions. Correction of acidotic state is carried out by administration of 4% sodium bicarbonate or Trisamine. In severe intoxication with dyspepsia and hypokalemia, potassium chloride is administered. If it is necessary to use special techniques, hemosorption - extracorporeal blood purification is performed.
The most complicated patients are subject to exchange transfusion, with replacement of 1.5-2 volumes of circulating blood. Force diuresis is also used with increasing the water load with 5% glucose solution, Ringer-Locke's solution and further administration of Mannitol and Lasix.
Some patients successfully practice plasmapheresis, use proteolysis inhibitors (Trasylol, Contrical). To eliminate disseminated intravascular coagulation syndrome intravenously administered Heparin in the amount of 1--=150 units per kg in 6 hours (not earlier than 12 hours after surgery). Vitamin C, rutin and calcium-containing drugs are used to reduce capillary permeability.
Pentoxol, Methyluracil, potassium orotate are prescribed to activate metabolism. Immunotherapeutic measures involve infusion of hyperimmune anti-staphylococcal plasma, staphylococcal vaccine and hyperimmune anti-staphylococcal γ-globulin.
It is obligatory to provide parenteral nutrition, calculated taking into account the recommended caloric content and balance of proteins, fats, carbohydrates. If possible, the patient is gradually transferred to a normal diet.
Antibiotic therapy is performed simultaneously with infusions (intravenous, intramuscular), as well as intraosseous (into the affected bone). Before identification of the causative agent, without wasting time, penicillin sodium salt is administered intravenously in high doses. Intraosseous administration involves the use of antibiotics with a broad spectrum of activity.
48 hours after evaluation of bacterial tests intraosseous injection, depending on resistance: cephalosporin preparations, Gentamicin, Claforan, etc., is administered. Additional injection of 5 million-10 million units of penicillin with 20 ml of 0.25% novocaine into the femoral artery is possible.
Preparations for intraosseous injection are pre-cooled to +20°C.
Local treatment of acute hematogenous osteomyelitis
The main point of local treatment is to reduce the high intraosseous pressure and prevent further spread of the pathologic process. Periostomy is complemented by specific microscopic trepanations that allow draining the cavity without disturbing the bone structure.
The technique involves the following manipulations:
- Cutting of the skin and PJC over the area of greatest pain;
- Muscle separation along the fibers;
- Opening of periosteum phlegmon, and in its absence - periosteum dissection;
- Execution of perforation holes using special milling cutters, with a needle placed in the center for intraosseous antibiotic therapy;
- Plaster splinting.
In total bone lesions, the above manipulations are performed in two metaphyseal areas. At the postoperative stage, the patient is dressed and examined daily, and wound revision is performed if necessary. The entire skeletal system is also examined for timely determination of probable secondary infected foci. If such foci are found, a bone puncture with temperature and pressure measurements is performed.
Physiotherapy can be applied as the acute inflammatory process subsides. Electrophoresis of antibacterial drugs, UVA, ultrahigh-frequency therapy are prescribed.
About a month later, a control radiograph is performed and the dynamics of treatment is evaluated.
Surgical treatment of acute hematogenous osteomyelitis
Surgical intervention in hematogenous osteomyelitis is prescribed in the presence of:
- Sequestration;
- Osteomyelitic bone cavity;
- Fistulas or ulcers;
- Changes in parenchymatous organs (due to osteomyelitis);
- Of localized malignancy.
Surgery for acute hematogenous osteomyelitis can be radical, conventionally radical, and reconstructive.
Radical interventions include these:
- Marginal resection of the affected bone segment;
- End resection of a part of a long bone in complicated traumatic osteomyelitis;
- Segmental resection of part of the long bone;
- Disarticulation or removal of the segment with the affected bone.
Conditionally radicalized interventions include these:
- Fistulosequestrectomy - involves excision of the fistula channels in conjunction with bone sequestrations;
- Sequestrnecrectomy - consists of resection of sequestrations from the compacted box after bone trepanation, or removal of the bony cavity in the form of a navicular flattening;
- Fistulosequestrnecrectomy (other name: extended necrectomy) - involves excision of a piece of necrosis, sequestrum, granulation, fistula, or scar tissue within healthy structures;
- Trepanation of the long tubular bone with sequestrnecrectomy is performed to gain access to the compacted box in the bone marrow canal with further resumption of its patency;
- Removal of the osteomyelitic focus followed by bilocal percutaneous compression-distraction osteosynthesis to replace the bone defect.
Restorative interventions involve the replacement of pronounced tissue defects and can be as follows:
- Soft tissue plastics (flap transfers);
- Plastic replacement with vascularized tissue;
- Combined techniques;
- Residual cavity filling;
- Plasty of bone cavities with blood-fed tissues (e.g., myoplasty);
- Replacement surgery using the Ilizarov method, extra-axial osteosynthesis.
Prevention
Prevention consists in early diagnosis, timely hospitalization, providing full therapeutic and surgical care to patients with any infectious-inflammatory processes. If necessary, prescribe courses of antibiotic therapy, anti-staphylococcal plasma and immunization with staphylococcal anatoxin, autovaccination, stimulation of reticulo-endothelial system functions. It is mandatory to exclude the possibility of aggressive impact of provoking factors, such as a sharp change in ambient temperature (hypothermia, overheating), trauma, etc.
Avoid the development of acute hematogenous osteomyelitis can be avoided by avoiding the influence of potentially unfavorable factors. For example, we are talking about intercurrent infectious processes, stressful situations, excessive physical activity, factors of excessive cold or heat.
Common therapeutic interventions include:
- Leading a healthy lifestyle;
- A full, varied and quality diet;
- Avoiding stressful situations;
- Regular immune support;
- Timely sanitation of infectious foci;
- Timely seeking medical help for injuries, traumas, wounds.
An important role plays and avoid self-medication: in the development of pathological processes, with injuries (both closed and open) consultations with doctors are mandatory.
Forecast
All patients who have undergone acute hematogenous osteomyelitis, necessarily put on the dispensary record. This is necessary for the timely detection of disease recurrence (exacerbation), evaluation of the results of therapy, preventive antibiotic therapy (for example, in the most "dangerous" periods - spring and fall). A person who has contracted the disease should visit his or her primary care physician at least twice a year.
From the first day after surgical intervention for hematogenous osteomyelitis patient gradually increase motor activity:
- Allow turns within the confines of the bed;
- Perform breathing exercises (static and dynamic exercises);
- Recommend lifting the torso while holding onto a suspension device above the bed.
To accelerate rehabilitation, improve trophic and metabolic processes, physical procedures are prescribed - in particular, magnetotherapy and UVB. A therapeutic course of physiotherapy may include from five to ten procedures.
In general, acute hematogenous osteomyelitis has a conditionally favorable prognosis. The patient's chances of recovery and full restoration of functionality of musculoskeletal mechanisms depend on the degree of pathologic process and the success of selected therapy, as well as on the timeliness and radicality of surgical treatment.
List of authoritative books and studies related to the study of acute hematogenous osteomyelitis
- "Bone and Joint Infections: From Microbiology to Diagnostics and Treatment" - authors: W. Zimmerli, M. E. Corti (Year: 2015)
- "Osteomyelitis: Diagnosis, Treatment and Prognosis" - by Mahmut Nedim Doral (Year: 2012)
- "Pediatric Osteoarticular Infections" - by Pierre Lascombes, Antoine G. S. Lascombes (Year: 2017)
- "Osteomyelitis: Risk Factors, Diagnosis and Treatment Options" - by Thore Zantop (Year: 2016)
- "Osteomyelitis - A Medical Dictionary, Bibliography, and Annotated Research Guide to Internet References" - by Icon Health Publications (Year: 2004)
- "Osteomyelitis: Symptoms, Causes and Treatments" - by Alton Carr (Year: 2012)
- "Osteomyelitis Research Advances" - by Carlos A. Leonard (Year: 2007)
- "Bone and Joint Infections: From Bacteriology to Diagnostics and Treatment" - by Andreas F. Mavrogenis (Year: 2018)
- "Clinical Microbiology Procedures Handbook, Vol. 1" by Amy L. Leber (Year: 2016)
- "Osteomyelitis: New Insights for the Healthcare Professional: 2012 Edition" - by Q. Ashton Acton (Year: 2012)
Literature
Kotelnikov, G. P. Traumatology / edited by Kotelnikov G. P.., Mironov S. P. - Moscow: GEOTAR-Media, 2018.

