Medical expert of the article
New publications
Acute hematogenous osteomyelitis in children
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
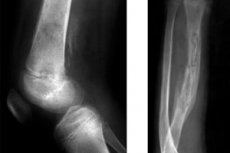
Infectious inflammation of the bone, provoked by bacteria that have entered the bone tissue with the bloodstream, is defined as hematogenous osteomyelitis. In pediatric practice, acute hematogenous osteomyelitis in children is considered a relatively common disease.
Epidemiology
Hematogenous osteomyelitis accounts for the majority of bone inflammation in childhood, and epidemiologic data indicate that the disease occurs in one in five thousand children under 13 years of age. Boys are twice as likely to be affected as girls, and children <5 years of age account for more than 50% of cases.Acute hematogenous osteomyelitis is particularly common in children <5 years of age and usually affects the metaphyses because of the abundant but slow blood flow in growing bone. [1], [2] The average age of patients is 7-10 years; up to 90% of cases are associated with Staphylococcus aureus.
The lower limb is most commonly affected, with the femur and tibia accounting for about 80% of cases.
The upper extremities are less commonly affected, with osteomyelitis of the humerus occurring in 12% of cases and osteomyelitis of the radius or ulna in 5% of patients.
Causes of the acute hematogenous osteomyelitis in children.
The causes of this disease are bacterial invasion, and the predominant pathogen is Staphylococcus aureus, which is part of the human opportunistic microflora, and its constant asymptomatic carriage (on the skin, oral mucous membranes and upper respiratory tract) is estimated at 30% of the total population. [3] For more information see. - causes and pathogenesis of staphylococcal infection
Acute gametogenic osteomyelitis caused by out-of-hospital methicillin-resistant S aureus (CA-MRSA) has become common in many countries. [4], [5] A 2016 study from a large US institution found that the incidence of acute musculoskeletal infections caused by MRSA increased from 11.8% in 2001-2002 to 34.8% in 2009-2010. [6]
In some countries (e.g., Spain, France, the United Kingdom, Israel, and Switzerland), Kingella kingae is increasingly recognized as a common etiology of pediatric bone and joint infections, especially in children <5 years of age. [7] Data on the epidemiology of K kingae infection in the United States are limited. In one US study of 99 children with septic arthritis, K kingae infection was diagnosed in 10 children aged ≤4 years; Polymerase chain reaction (PCR) alone identified the causative agent in 8 cases. [8]
Transient bacteremia (i.e., the presence of bacteria in the blood), as well as septicemia create prerequisites for hematogenous dissemination of infection and the formation of secondary foci of inflammation in various organs and tissues - including bone.
Arterial vessels supplying blood to bone tissue penetrate the medullary substance and connect with smaller periosteal arteries, providing perfusion of the cortical layer of bone and ion (calcium) exchange. Branches of arteries flowing into the arteriovenous sinuses of the brain substance carry blood to hematopoietic and stromal cells. And the development of acute hematogenous osteomyelitis in children experts explain the increased blood supply of growing bones, which facilitates the entry of bacteria into bone tissue.
Acute hematogenous osteomyelitis etiologically may be associated with streptococcal infection, particularly Streptococcus pyogenes (beta-hemolytic group A streptococcus) and Streptococcus pneumoniae (pneumococcus).
Bone inflammation can also be caused by:
- Haemophilus influenzae infection (Haemophilus influenzae);
- Kingella kingae, a member of the obligate microflora of the nasopharynx, involved in the development of acute inflammation of the sternum and heel bones in young children;
- Bartonella bacillus (Bartonella henselae), which can cause osteomyelitis of the axial skeleton as a complication of cat scratch disease in debilitated children;
- Salmonella nontyphoidal (Salmonella non-rushnontyphoidal), which usually affects the digestive tract, but with immune problems can cause a generalized form of bacteremia, penetrate through the bloodstream to other organs and tissues with the development of focal infection.
As clinical practice shows, acute hematogenous osteomyelitis of newborns is most often caused by infection of bone tissues by Streptococcus agalactiae (group B streptococci colonizing vaginal mucous membranes), Staphylococcus aureus and Escherichia coli (Escherichia coli).
Risk factors
Risk factors for bacteria entering the bloodstream can be: damage to the gums during brushing or dental procedures, tooth abscess - with the development of hematogenous osteomyelitis of the jaw; ear and paranasal sinus infections; pustular diseases of the skin and subcutaneous tissue (impetigo, furunculosis, staphylococcal pyoderma, streptoderma); bacterial tonsillitis, pharyngitis and pneumonia, as well as treatment of bone fractures with the installation of external compression-distraction structures. Read more - staphylococcal infection in children
Risk factors for acute bone inflammation in children include a weakened immune system of various etiologies, diabetes mellitus, dialysis therapy, sickle cell anemia, and juvenile rheumatoid arthritis.
And predisposing factors for hematogenous osteomyelitis in newborns include prematurity, cesarean delivery, and invasive procedures (umbilical cord or vein catheterization).
Pathogenesis
Osteomyelitis may result from direct inoculation as a result of penetrating trauma or may spread from an adjacent site of infection, but the most common mechanism of infection in children is hematogenous inoculation of bone during an episode of bacteremia.
After penetration of bacteria into the intensely blood-supplied bone tissue, foci of bacterial contamination are formed in it and proliferation of microorganisms in the bone begins. For example, in S. Aureus lesions, the pathogenesis of hematogenous osteomyelitis, which almost always begins in the metaphyses of long bones adjacent to the epiphyseal growth zone, is caused by virulence factors of this bacterium.
In particular, under the action of the coagulase enzyme produced by the microorganism, blood fibrinogen is transformed into fibrin with the formation of thrombus in the arteriovenous sinuses of the cerebral substance of the bone. Thus, having cut off its "living space" from the complement system (the action of protective blood cells) S. Aureus begins to multiply, producing enzymes, secreting exotoxins (antigens) and secreting by-products, which leads to damage to the membranes of bone tissue cells and their death.
Bone lysis also occurs as a result of the action of lysosomal enzymes of leukocytes, which enter the affected area to absorb infectious organisms. The purulent exudate formed in this process spreads into the blood vessels of the bone, disrupting blood flow, gets under the periosteum and into the bone tissue with elevation of the periosteum and formation of a subosteal abscess. As a result, inflammatory changes in the bone occur: sequestrations - areas of dead infected bone.
Osteomyelitis can be categorized as acute (duration of symptoms <2 weeks), subacute (duration of symptoms from 2 weeks to 3 months), and chronic (prolonged infection that develops over months or years). [9]
Symptoms of the acute hematogenous osteomyelitis in children.
The first signs of acute hematogenous osteomyelitis in children may be sudden or appear gradually in the form of reddening of the skin over the affected bone, local swelling (edema) and hyperthermia.
The most common clinical features of pediatric hcmetogenic osteomyelitis reported in a 2012 systematic review are: pain (81%), localized signs/symptoms (70%), fever (62%), decreased range of motion (50%), and decreased weight bearing (49%). [10] Systemic signs and symptoms such as high fever, tachycardia, and painful claudication are more commonly reported in children with MRSA osteomyelitis than in children with methicillin-sensitive S aureus osteomyelitis (MSSA), although these findings are not specific to MRSA alone. [11] In contrast, children <4 years of age with K kingae bone and joint infection have more benign manifestations and course: less than 15% fever on admission and 39% with normal C-reactive protein (CRP) levels. [12]
Read more in the publication - osteomyelitis of long tubular bones in children
Children with pelvic osteomyelitis are often unable to shift their weight from the affected area, but a stooping gait appears when they attempt to do so.
Stages
The stages of osteomyelitis are divided into intramedullary and extramedullary, and the types are defined as superficial osteomyelitis (affecting the cortical layer of bone); medullary (inflammation is localized in the cavitas medullaris - the medullary cavity); focal or localized (limited to an area of the cortical layer and medullary canal) and diffuse (inflammation of the bone takes over its entire diameter).
Complications and consequences
Complications and consequences that can occur in acute osteomyelitis in children include:
- Bone deformity and impaired longitudinal bone growth, which leads to serious orthopedic problems;
- Bone fistula formation;
- Pathologic fractures;
- The development of septic arthritis;
- The development of chronic osteomyelitis;
- Infectious inflammation of adjacent soft tissues.
Diagnostics of the acute hematogenous osteomyelitis in children.
Read more in the publication - diagnosis of osteomyelitis
Differential diagnosis
The differential diagnosis of acute hematogenous osteomyelitis in children includes infection (e.g., septic arthritis, cellulitis), trauma, malignancy (e.g., osteoid osteoma, acute lymphoblastic leukemia, Ewing's sarcoma, osteosarcoma), bone infarction (in children with sickle cell anemia or other hemoglobinopathies), metabolic diseases (e.g., Gaucher disease), vitamin A deficiency, avascular necrosis, or chronic recurrent multifocal osteomyelitis.
Who to contact?
Treatment of the acute hematogenous osteomyelitis in children.
Treatment is multidisciplinary, involving pediatricians, pediatric infectious disease specialists, orthopedic surgeons, and radiologists. [14]
Full details in the articles:
- Treatment of osteomyelitis
- Antibiotics for staphylococcus aureus.
- Treatment of streptococcal infection
- Treatment of Haemophilus influenzae infection
Studies have shown that appropriate antibiotic therapy without surgery may be sufficient in 90% of cases of acute hematogenous osteomyelitis. [16] In some cases of complicated osteomyelitis caused by CA-MRSA, surgical incision and drainage (including multiple procedures) may be indicated. [17] Surgical intervention - in the form of drainage of purulent accumulations in the bone or removal of infected bone tissue - is performed when subcutaneous, intraosseous, or adjacent soft tissue abscesses are present or when there is no improvement with medical therapy.
Indications for surgical treatment in acute hematogenous osteomyelitisare persistent symptoms (fever, local inflammation) that do not respond to empirical antibiotic therapy, the presence of periosteal or other deep soft tissue abscess (more common with MRSA or strains expressing virulence genes such as PVL), concomitant septic arthritis, especially of the hip and shoulder joints, the presence of bone necrosis and fistula formation. [18]
Prevention
To prevent acute infectious bone inflammation is necessary:
Forecast
For most children, the prognosis of acute hematogenous osteomyelitis - if treated aggressively early - is favorable. Although there is a possibility of recurrence of infection several years later, even after successful treatment.
List of authoritative books and studies related to the study of acute hematogenous osteomyelitis in children
- "Pediatric Bone: Biology and Diseases" (2003) - by Francis H. Glorieux, John M. Pettifor, Harald Jüppner.
- "Bone and Joint Infections: From Microbiology to Diagnostics and Treatment" (2015) - by Werner Zimmerli, J. Ralf Ross, Parham Sendi.
Research and articles:
- "Acute Hematogenous Osteomyelitis in Children: Clinical Presentation and Management" (2018) - authors: L.Y. Novikova et al. The article was published in the Journal of Pediatric Orthopaedics."
- "Hematogenous Osteomyelitis in Children: A Comprehensive Review" (2017) - authors: S.M. Morozov et al. The article was published in the Journal of Bone and Joint Infection."
Использованная литература

