Medical expert of the article
New publications
13c urease test: preparation, results, positive, negative
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Since the discovery of the Helicobacter pylori bacterium associated with chronic gastritis and gastric and duodenal ulcers, diagnostic methods have been developed, including the urease test, which allows detecting these microorganisms in a specific patient, confirming their involvement in the development of gastrointestinal diseases and prescribing effective treatment.
Urease enzyme as a biomarker of Helicobacter infection
H. pylori bacteria protect themselves from the acidic environment in the lumen of the stomach in two ways. First, by damaging the mucous membrane with their flagella, the microorganisms reach its lower layers, right down to the epithelial cells, where the pH is higher (i.e., the acidity is lower). Second, the bacteria neutralize the acid by synthesizing large quantities of the catalytically active high-molecular metalloenzyme urease or urea amidohydrolase.
The use of urease in the diagnosis of Helicobacter is possible due not only to the cytoplasmic activity of this enzyme, but also to external interaction with host cells.
Under the action of urease, the breakdown of gastric urea into hydrogen nitride (ammonia) and carbon dioxide (carbon dioxide) occurs. They react with hydrochloric acid in the gastric juice and provide a zone of neutral acidity around H. pylori, and also support the metabolism of bacterial cells.
This is why urease is the most important factor in the colonization of H. pylori in the human gastric mucosa, and the detection of ureolytic activity is considered a biomarker of the virulence of this bacterium, which gastroenterologists – by conducting a urease test – use to diagnose Helicobacter infection, as well as to monitor the results of drug-induced destruction (eradication) of bacteria.
H. pylori diagnostics includes invasive and non-invasive tests – depending on whether endoscopic examination of the stomach (fibrogastroduodenoscopy) is required or not. The invasive test is the rapid urease test or express urease test (RUT-test), which requires obtaining tissue samples (biopsy). 13C urea breath test (13C-UBT) is the most common non-invasive test.
It should be noted that non-invasive diagnostics of H.pylori can be performed using a blood test for antibodies (specificity at the level of 75%, sensitivity - 84%), urine ELISA (with a sensitivity of 96% and specificity of 79%), and a coprogram for bacterial antigens. More information - Helicobacter pylori infection: antibodies to Helicobacter pylori in the blood
Indications for the procedure urease test
Colonization of the gastric mucosa by H. pylori in itself is not a disease; it is a factor in increased bacterial load on the body, which under certain conditions can trigger the development of a number of pathologies of the stomach and upper gastrointestinal tract.
Indications for diagnostics of Helicobacter infection, in particular, the urease test, are associated with gastritis with increased acidity, antral and atrophic gastritis, duodenitis, gastric ulcer and duodenal ulcer, gastric MALT lymphoma. After endoscopic resection of early-stage gastric cancer, a histological examination can be performed in combination with a rapid urease test - FGDS with a urease test.
Gastroenterologists may prescribe a urease test if patients complain of a feeling of heaviness and discomfort in the epigastric region, frequent heartburn after eating, sour or rotten belching, bitterness in the mouth, nausea, intestinal disorders, aching or cramping pain in the stomach.
Preparation
Preparation for the 13C urea breath test consists of the patient stopping: taking antibiotics 4 weeks before the test, and NSAIDs, proton pump inhibitors (reducing stomach acidity) and antacids or adsorbents used for heartburn - at least two weeks before. Taking any medications should be stopped five to six days, and drinking alcohol and smoking - three days before the test.
It is also recommended to avoid eating legumes for about a week before testing, as beans, peas, lentils, soybeans and beans contain urease (which protects plants from diseases and insect pests).
The evening before the test, a late heavy dinner is contraindicated; on the day of testing, you should perform normal oral hygiene, and an hour and a half before the test, you should not drink anything or use gum.
Who to contact?
Technique urease test
Technique of implementation:
- First, a basic breathing sample is taken - an exhalation is made into a soft plastic container (and hermetically sealed);
- liquid with added 13C-urea is taken orally;
- After 25-30 minutes, a second sample of exhaled air is taken into another container.
The samples obtained in this way are analyzed on a mass spectrometer with separation of isotopes in a second sample and determination of their concentration. The difference between the values in the second and first sample is expressed as delta (δ) compared to the baseline level. Normal values, i.e. negative values of the labeled atom 13C in uninfected patients vary from 0.15-0.46%, and positive values in the presence of infection are 1.2-9.5% with a urea hydrolysis rate of more than 12-14 μg/min.
To put it simply: the detection of 13C-labeled carbon dioxide in exhaled air indicates that urea has been hydrolyzed by the urease enzyme H. pylori, which, in fact, confirms the fact of its presence in the stomach.
H. pylori breath test
The 13C-UBT test or 13C urea breath test for Helicobacter pylori is one of the most important non-invasive methods for detecting this infection: with 100% sensitivity and 98% specificity, the risk of false positive and false negative results compared to histology and blood antibody testing is 2.3% lower.
The analysis is based on the hydrolysis of orally administered liquid urea labeled with a carbon atom (stable non-radioactive isotope) 13C (50-75 mg 13C-urea diluted in 100 ml of liquid) by H. pylori urease.
Urea labeled with an isotope indicator undergoes hydrolysis in the stomach with the release of ammonia and carbon dioxide containing labeled atoms, which diffuses into the blood and is excreted from the lungs during breathing. The labeled carbon dioxide is recorded by an analytical device - a mass spectrometer, the operation of which is based on non-dispersive isotope-selective spectroscopy, or an infrared spectroscopic analyzer.
Rapid urease test
Rapid Urease Test (RUT) is performed during endoscopic examination of the stomach and duodenum - using modern endofibroscopes - and simultaneous collection of biopsy samples. The biomaterial is supposed to be taken from the antral part of the stomach. So fibrogastroduodenoscopy or FGDS with urease test is an invasive diagnostic method.
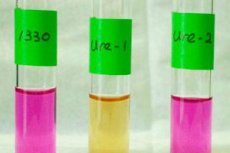
The obtained biopsy is completely immersed in a prepared standardized medium containing agar gel, urea, acid-base indicator phenolsulfophthalein and a bacteriostatic agent (added to prevent the growth of contaminating microorganisms and false positive results).
If H. pylori bacteria are present in the stomach tissue sample, the urease they produce will hydrolyze urea and raise the pH, which is clearly visible as the indicator changes from yellow to orange (at pH 6.8) and purple (at pH> 8). 75% of positive tests change color within 120-180 minutes, and the faster the indicator changes color, the greater the number of bacteria. But tests that appear negative are kept for 24 hours.
Rapid Urease Test Positive, What Does It Mean? A positive RUT test – the indicator turns red – means that the biopsy sample placed in the agar medium contains at least 105 H. pylori bacteria, although their concentration is usually higher.
The sensitivity of various test modifications varies in the range of 90-98%, and the specificity – 97-99%.

As noted by gastroenterologists, if the patient's conclusion indicates a sharply positive urease test (three crosses), this means: pH> 8, and the indicator changed color in less than 60 minutes from the moment of immersion of the biopsy, which indicates a large number of H.pylori and a high level of urease expression. The approximate number of bacteria can be counted during histological examination of the biopsy under a microscope, and if it exceeds 40-50 in the visualized area, the level of infection is considered high.
The 13C urea breath test rarely gives false-positive results, and in patients with suspected gastric or duodenal ulcer, one positive test is considered to confirm the diagnosis, whereas a negative result should be confirmed by EGD with urea test.


 [
[