Parotid salivary gland
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Parotid salivary gland (glangula parotidea) is a paired, serous type of secretion. It has an irregular shape, outside it is covered with a thin capsule. Weight of the gland 20-30 g.
Parotid gland, most of it is located on the outer surface of the mandible, the smaller part is located in the mandibular fossa formed by the branch of the lower jaw, the inner pterygoid muscle, the mastoid process, the sternocleidomastoid muscle, the posterior abdomen of the digastric muscle, the lower wall of the external auditory canal . The form of the gland is very diverse, but many authors find that it is similar to a trihedral pyramid, although in reality the parotid salivary gland is difficult to compare with anything.
Parotid salivary gland three surfaces: outer, anterior, posterior, and two bases or, in the words of many authors, "two poles". The anterior edge of the gland somewhat covers the outer surface of the masticatory muscle, the posterior margin - the sternocleidomastoid muscle; the lower pole often reaches the angle of the lower jaw, and the upper pole sometimes reaches the zygomatic arch.
Parotid salivary gland is enclosed in a case formed by the parotid-chewing fascia, which is a superficial leaf of the facial fascia. This case together with the chewing muscle is attached above to the zygomatic bones and zygomatic arch, below - to the outer surface of the angle of the lower jaw. At the posterior edge of the masticatory muscle, the chewing fascia splits and covers a portion located on the outer surface of this muscle. The front fascia is a dense leaf from which the processes penetrate into the thickness of the gland and divide it into lobules. In the course of the parotid duct, the fascia thickens and contains the vessels accompanying it and, sometimes, an additional lobule of the gland. The glandular gland is a space that limits the leaflets of the parotid-chewing fascia. In the formation of the inner sheet of the fascia of the gland, there are the cases of the nodulating and bile-abdominal muscles (the posterior abdomen), the cuffs of muscles coming from the styloid process; in front - the fascial pouch of the inner pterygoid muscle, below and inside - the cuffs of the dorsal and duodenal muscles (anterior abdomen). The upper surface of the gland, facing the external auditory canal, and the inner surface of the pharyngeal process of the gland are not covered with a fascia and are separated by loose fiber. Parotid salivary gland spurs into the gap between the ear canal and the capsule of the temporomandibular joint spurs in the region of the pharyngeal process, in the lower part, where the inner surface is turned to the posterior abdomen of the dorsal and silo-hyaline muscles, there is also a strong fascia. Part of the inner surface of the gland without fascial cover belongs to the cellulose of the near-hypopharyngeal space. Parotid-chewing fascia passes into the fascial formations of neighboring structures (externally to the superficial fascia of the neck, from behind to the pre-invertebrate fascia, inside - to the shigophyllous aponeurosis and vascular cava). The thickness of the capsule depends on the age and sex of the person.
The skin is well displaced, under it there is a thin layer of subcutaneous fat that surrounds the outer sheet of the fascia of the gland and passes into the cellulose of neighboring regions, which leads to unhindered spread of the tumor infiltrate in all directions. A deep leaf of the parotid fascia separates the gland from the lateral wall of the pharynx, the posterior abdomen of the digastric muscle, from the muscles and ligaments attached to the styloid process, from the posterior surface of the internal pterygoid muscle.
At the posterior edge of the gland, the inner fascia leaf merges with the outer one, and at the angle of the lower jaw both sheets form a strong septum separating the lower pole from the submaxillary.
The fascial vessels and nerves are fused with the glandular capsule, so they do not leave any defects in the capsule at their entry or exit points. However, the possibility of the pathological process is described along the course of the external carotid artery into the region of the carotid triangle of the neck, and along the internal jaw artery - into the maxillofacial gap of the masticatory space.
At the anterior margin, above the parotid duct, sometimes there is an additional fraction 1-2 cm in diameter. It occurs in 10-20% of individuals and can be a source of tumor development.
Parotid salivary gland secretes its secret from the parotid salivary duct. Usually it happens to be a main line and takes in its path side channels (from 7 to 18). In some cases, it is formed from the fusion of two almost equal in diameter ducts, sometimes has a branching structure. A parotid duct appears on the border of the upper and middle third and is directed obliquely upward and forward, and then, turning downwards, it runs horizontally along the outer surface of the masticatory muscle. At its edge, the duct curls inwards, permeates the skew fat and the buccal muscle. Then, for 5 cm, the duct is located along the mucous membrane of the cheek and opens on the eve of the mouth at the level of the upper second molar or between the first and second upper molars. The opening of the parotid duct has a rounded shape or a narrow slit shape, it is often located on the dorsal elevation in the form of a papilla. The diameter of the duct is 3 mm, its length is from 15 to 40 mm. In the parotid duct, the duct of the additional lobe of the gland drains, which gives rise to the fact that many researchers do not call it an independent gland. Often, the anterior margin extends far forward and almost reaches the anterior edge of the masticatory muscle. In such cases, the beginning of the parotid duct is masked by the gland.
Most anatomists and surgeons determine the projection of the parotid duct along the line connecting the tragus of the ear and the corner of the mouth. In children, the duct is often projected along the line: the corner of the mouth and the earlobe of the ear.
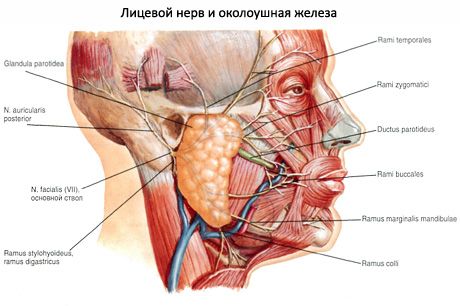
Parotid salivary gland is permeated with numerous blood and lymphatic vessels, nerves and lymph nodes. In most cases, the vessels are located in the thickness of the gland, closer to its front surface. Sometimes the vessels pass through the inner surface of the gland. The largest blood vessel is the external carotid artery, which is tightly fused with the parenchyma of the gland and is then divided into its terminal branches: the posterior ear, superficial temporal, transverse facial and maxillary. Outside the external carotid artery is the external jugular vein. The back ear and transverse facial vein enter into it. Venous blood flows through the posterior-jawed vein, which is formed from the fusion of superficial temporal and jaw veins.
Innervation: sensitive - parotid branches of the ear-temporal nerve, secretory (parasympathetic) - fibers of the ear-temporal nerve (from the ear node), sympathetic - from the outer carotid plexus.
The parotid salivary gland is innervated by the parotid branches of the ear-temporal nerve; secretory fibers - from the ear ganglion; sympathetic nerves accompany the superficial temporal artery. The additional part and parotid duct are innervated by the branches of the facial nerve.
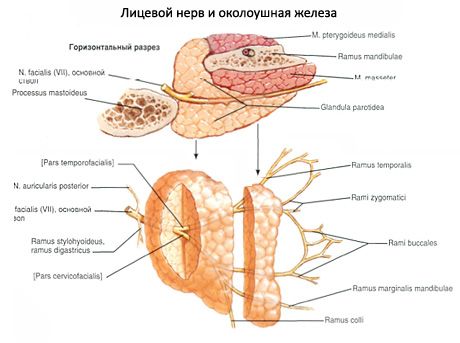
Parotid salivary gland is permeated with the extracranial section of the facial nerve, which is the VII pair of cranial nerves. The facial nerve emerges from the skull through an awl-mastoid aperture. The length of the nerve to the posterior margin is on average 10 mm. During the operation, as some surgeons say, it is possible to extend this nerve segment by pulling the lower jaw forward. The facial nerve penetrates more often in the middle third of the gland. In the parenchyma of the gland, the nerve passes a common trunk of approximately 15 mm, always outside of the external carotid artery and the external jugular vein. Then the facial nerve is divided into two branches. One branch goes horizontally, continuing the course of the common trunk, and is divided into three branches. The other branch is directed downwards almost at right angles, passes the largest distance (about 20 mm) in the parenchyma of the gland and is also divided into two branches. Very rarely, the facial nerve is divided before joining the organ. In the gland itself nerves widely anastomose with each other, which creates considerable difficulties in isolating them during the operation. From the tissue of the gland to the mimic muscles of the face there are five main branches of the facial nerve: temporal, zygomatic, buccal, mandibular, cervical.
According to the general opinion of the researchers, the topography of the five main branches of the facial nerve is extremely variable. Different variants of facial nerve division are described. As a guide in practical surgery, the location of the parotid duct can be used to locate the mandibular branch going to the corner of the mouth, and to find the zygomatic branch a straight line connecting the angle of the eye with the earlobe.
Parotid salivary gland is also permeated with an ear-temporal nerve, which is a branch of the mandibular nerve. The ear-temporal nerve penetrates into the gland somewhat lower and behind the articular process of the lower jaw and splits into many small trunks, the topography of which is complex. One of the branches accompanies the superficial temporal artery, the other branches form a thickening in the form of a plate, from which numerous thin branches branching into the different sides (including the skin of the auricle and external auditory canal), which anastomose with the sympathetic plexus of the external carotid artery.
Parotid salivary gland has a superficial and a deep part. The superficial part corresponds to that part of the gland that is located on the masticatory muscle. The deep part occupies the indentation behind the branch of the lower jaw. The facial nerve and its connective tissue case, passing through the thickness of the gland, are the landmark, on the outside of which the surface part is located, from the inside - deep.
Blood supply: parotid branches of the surfaces of the temporal artery, venous outflow - into the submandibular vein.
Outflow of lymph: to superficial and deep parotid lymph nodes.
What do need to examine?


 [
[