Medical expert of the article
New publications
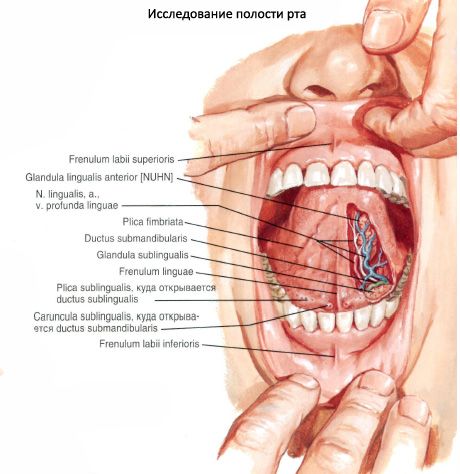
The hyoid salivary gland
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The sublingual salivary gland (glangula sublingualis) is paired, with predominantly mucous secretion. It is located on the mylohyoid muscle, directly under the mucous membrane of the floor of the oral cavity. Its lateral surface is in contact with the inner surface of the body of the lower jaw in the area of the homonymous fossa. The medial side of the gland is adjacent to the genioglossus, geniohyoid and hyoglossus muscles. The large duct (ductus sublingualis major) is the main excretory duct and opens on the homonymous papilla. Several small ducts (ductus sublinguals minores), which are additional for the excretion of saliva, flow into the oral cavity on the surface of the homonymous fold.
Numerous small ducts open along the fold. There are five intermuscular slits, through which the pathological process quickly spreads to neighboring structures. Outwardly and anteriorly there is the space of the mylohyoid groove, where the lingual nerve, the duct of the submandibular sclerosis with the surrounding lobe of the gland and the nerve of the same name with the lingual vein pass. This is the "weakest" place in the space. The sublingual cellular space also communicates with the anterior parapharyngeal space through the stylohyoid muscle and its fascial sheath.
Innervation: secretory (parasympathetic) - fibers of the facial nerve, through the chorda tympani and ganglion, sympathetic - from the external carotid plexus.
Blood supply: submental artery. Venous drainage: veins.
Lymph drainage: to the submandibular and submental lymph nodes.
What do need to examine?


 [
[