Mixed hydrocephalus
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Mixed hydrocephalus is a condition in which there is an excess of cerebral fluid inside the cranial cavity (cerebral ventricle) and/or outside of it. It is called "mixed" because it can combine both internal (inside the skull) factors, such as blockage of cerebral fluid circulation, and external (outside the skull) factors that can lead to an increase in brain fluid volume.
The causes of mixed hydrocephalus can be varied and may include the following:
-
Blockage of cerebral fluid circulation within the skull, such as due to tumors, bleeding, or inflammation.
-
Excess cerebral fluid due to disruption from external factors such as infections, trauma, or other medical conditions that can affect cerebral fluid dynamics.
-
A combination of internal and external factors leading to excess cerebral fluid and increased pressure inside the skull.
Symptoms of mixed hydrocephalus can vary depending on the cause and degree of impaired circulation of brain fluid. They may include headache, nausea, vomiting, difficulty with coordination and balance, changes in mental status, impaired vision, and other neurological symptoms.
Treatment for mixed hydrocephalus depends on the cause and severity of the condition. It may involve surgery to remove the blockage of cerebral fluid circulation, treatment of the underlying condition, or other medical procedures to normalize the level of cerebral fluid and pressure inside the skull. Treatment should always be under the guidance of qualified medical professionals. [1]
Causes of the mixed hydrocephalus
The causes of mixed hydrocephalus can be varied and may include the following factors:
- Congenital anomalies: Some babies may be born with brain abnormalities that can cause mixed hydrocephalus. These anomalies may include stenosis (narrowing) of Sylvius acuvductus or other defects.
- Inflammatory diseases: Infections such as meningitis can cause inflammation and block the normal circulation of cerebral spinal fluid, which can lead to mixed hydrocephalus.
- Trauma: Head trauma or brain injury can cause impaired fluid circulation and therefore hydrocephalus.
- Brain tumors: Brain tumors can compress brain structures and block the circulation of cerebral spinal fluid, which can lead to mixed hydrocephalus.
- Internal anomalies: Certain genetic or congenital anomalies can affect the development of systems responsible for the normal circulation and resorption of cerebral spinal fluid.
- Other Factors: Mixed hydrocephalus can also be caused by other medical conditions and factors that may vary from patient to patient. [2]
Pathogenesis
The pathogenesis of mixed hydrocephalus can be complex and involve several factors. Here are some of them:
- CSF production: Normally, cerebral spinal fluid is produced in the brain, and excess fluid should be expelled from the ventricles of the brain and circulate within the cranial cavity. In mixed hydrocephalus, there may be an imbalance between CSF production and resorption, which can lead to CSF accumulation.
- Blockage of drainage pathways: One common mechanism of mixed hydrocephalus is blockage of the drainage pathways that normally allow cerebral spinal fluid to leave the brain. This can be caused by tumors, blood clots, infections, or other abnormalities.
- Increased CSF production: In some cases, hydrocephalus may develop due to increased production of cerebral spinal fluid. This may be due to certain medical conditions or genetic factors.
- Resorption disorder: The main way that cerebral spinal fluid is resorbed from the brain is by absorption through special structures called villosites, which form within the ventricles of the brain. Disruption of this process can lead to CSF accumulation.
The pathogenesis of mixed hydrocephalus can be complex and multifaceted, and it can vary from patient to patient depending on the causes and characteristics of their disease. A consultation with a neurologist or neurosurgeon, as well as additional medical tests such as MRI or CT scans of the brain, are required to determine the exact pathogenesis and choose the most appropriate treatment. [3]
Symptoms of the mixed hydrocephalus
Symptoms of mixed hydrocephalus can vary depending on the degree of impaired circulation of brain fluid and the cause of its development. Common symptoms may include:
- Headache: This is one of the most common symptoms of mixed hydrocephalus. The headache may be moderate to intense and may get worse over time.
- Nausea and vomiting: Increased pressure inside the skull can cause nausea and vomiting.
- Difficulties with coordination and balance: Patients may have difficulty with movement, coordination, and balance.
- Vision impairment: Increased pressure inside the skull can put pressure on the optic nerves, which can lead to changes in vision, including blurred vision, double vision, and impaired vision.
- Seizures: Some patients with mixed hydrocephalus may have seizures.
- Changes in mental status: There may be changes in mental status such as irritability, depression, drowsiness or insomnia.
- Increased head volume (in children): Children with mixed hydrocephalus may have an increase in head volume (hydrocephalus) because their skull bones have not yet closed and the brain can push the skull outward.
- Other neurologic symptoms: Depending on the extent and location of cerebral fluid enlargement, other neurologic symptoms such as impaired motor function, changes in consciousness, and others may be present.
Symptoms of mixed hydrocephalus can vary and depend on many factors, including the cause and degree of impaired circulation of brain fluid. [4]
Mixed hydrocephalus in a child
This is a condition in which the inner cerebral ventricles (ventricles) fill with excess cerebral spinal fluid (CSF) and may also be accompanied by fluid accumulation outside the cerebral ventricles. This condition is a type of hydrocephalus, and it can have different causes and severity in different children.
The symptoms and severity of mixed hydrocephalus in a child can vary greatly depending on many factors, including:
- Cause of hydrocephalus: The prognosis and symptoms will depend on what caused the development of mixed hydrocephalus. It could be a congenital developmental disorder, a brain tumor, inflammation, or other factors.
- Child's age: In infants and newborns, mixed hydrocephalus can manifest in a variety of ways, such as rapid head enlargement, irritability, insomnia, and feeding problems. In older children, symptoms may include headaches, behavioral changes, coordination problems, and movement disorders.
- Severity: Hydrocephalus can be moderate or severe, which also affects symptoms and prognosis. Severe hydrocephalus can cause more severe neurological symptoms and have more serious consequences.
To determine the severity and cause of mixed hydrocephalus in a child, an extensive medical evaluation, including brain masses using MRI or CT scans and other diagnostic techniques, must be performed. Treatment will depend on the specific circumstances of each case and may include surgery to drain excess fluid or correct the underlying cause. It is important to discuss all questions and concerns with your pediatric neurosurgeon and other specialists to develop the best treatment plan for your child.
Stages
Hydrocephalus does not have strictly defined stages like some other diseases. However, we can talk about different degrees of severity and development of this condition depending on factors such as progression of symptoms, pressure inside the skull and structural changes in the brain. The following are the common degrees of hydrocephalus development:
- Initial stage: In this stage, the patient may have mild symptoms such as headaches, localized soreness or discomfort. The brain ventricles may be enlarged, but the volume of excess fluid is not yet too large.
- Progressive stage: Over the years, symptoms may increase and the hydrocephalus may become more severe. The inner cerebral ventricles may further dilate and intracranial pressure increases. The patient may experience more severe headaches, nausea, vomiting, and neurologic deficits.
- Severe stage: If untreated, hydrocephalus can become severe and cause serious impairment. Brain structures may be severely compressed, which can lead to cognitive impairment, loss of vision, hearing, and motor skills. This stage can be life threatening for the patient.
It should be noted that each case of hydrocephalus is unique and the severity can vary greatly. To accurately assess the stage of hydrocephalus and develop a treatment plan, an extensive medical examination and specialist follow-up is necessary.
Moderate and severe mixed hydrocephalus are gradations of the severity of the condition that medical professionals can use to describe the extent and impact of hydrocephalus on a patient. These terms can be useful in determining the need for treatment and predicting prognosis.
- Moderate mixed hydrocephalus: Usually indicates that there is a moderate accumulation of cerebral spinal fluid inside and/or outside the cerebral ventricles, causing moderate symptoms and/or changes on MRI or CT scan of the brain. The patient may experience headaches, nausea, vomiting, and some neurologic symptoms.
- Severe mixed hydrocephalus: Indicates a more serious accumulation of cerebral spinal fluid and more severe symptoms. The cerebral ventricles may be significantly dilated and the pressure inside the skull may be high. Patients with severe hydrocephalus may have severe headaches, visual disturbances, hearing loss, and other serious neurological symptoms that can threaten their health and quality of life.
Complications and consequences
Mixed hydrocephalus, like other forms of hydrocephalus, can cause a variety of complications and have serious consequences, especially if it is not treated properly. Here are some of the possible complications and consequences:
- Disorders of neurologic function: Accumulation of cerebral spinal fluid and increased pressure within the cranial cavity can lead to damage to the brain and nerve structures. This can manifest as headaches, seizures, loss of consciousness, impaired vision, hearing, motor skills, and other neurological deficits.
- Increased head volume: Hydrocephalus can cause an increase in head volume, especially in children. This can lead to cosmetic problems and physical discomfort.
- Developmental delay: Children with hydrocephalus may experience delays in physical and mental development due to the pressure placed on the brain. Early detection and treatment can help minimize these delays.
- Infections: If a patient has a shunt (a medical device to drain cerebral spinal fluid), he or she may be susceptible to infections that can cause serious complications.
- Psychosocial and emotional problems: Hydrocephalus and its treatment can have an impact on the psychosocial and emotional well-being of the patient and family. This may include stress, depression, anxiety, and other emotional problems.
- Complications after surgery: If hydrocephalus has been surgically corrected, complications may arise from the surgery itself or from medical devices (such as a shunt).
Importantly, early detection and treatment of mixed hydrocephalus can significantly reduce the risk of complications and improve the patient's prognosis. [5]
Diagnostics of the mixed hydrocephalus
Diagnosing mixed hydrocephalus involves several steps and medical procedures to determine if this condition is present and identify its cause. Here are some basic methods for diagnosing mixed hydrocephalus:
- Clinical Examination: The physician will perform an initial clinical examination of the patient, including gathering medical and family history, as well as eliciting and characterizing symptoms.
- Neurologic exam: Your doctor may perform a neurologic exam to assess neurologic function, including motor coordination, balance, vision, and others.
- Imaging education:
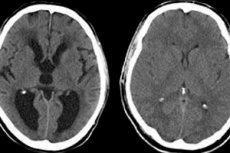
- Magnetic Resonance Imaging (MRI): MRI is a commonly used technique to visualize the brain and determine the volume of cerebral fluid, its distribution, and the presence of obstructions in its circulation. MRI can help identify changes inside and outside the skull.
- Computed tomography (CT): CT scans can also be used to visualize the brain and identify abnormalities, blockages, or changes associated with hydrocephalus.
- Ultrasound (in children): In infants and infants, a brain ultrasound may be performed to evaluate cerebral fluid volume and hydrocephalus.
- Cerebral spinal fluid analysis: Performing a lumbar puncture (spinal tap) with cerebral spinal fluid analysis may be necessary to detect infections or other pathologies that may cause hydrocephalus.
- Other tests: Additional tests and examinations may be needed to determine the cause of hydrocephalus, such as tests for infections, biochemical tests, and others.
The diagnosis of mixed hydrocephalus can be complex and requires the collaboration of various specialists, including neurosurgeons and neurologists. [6]
Differential diagnosis
The differential diagnosis of mixed hydrocephalus involves identifying and distinguishing this form of hydrocephalus from other conditions that may cause similar symptoms or have similar clinical manifestations. It is important to determine the underlying cause of hydrocephalus in order to choose the most effective treatment. Below are some conditions to consider in the differential diagnosis of mixed hydrocephalus:
- Internal hydrocephalus: The main difference between mixed hydrocephalus and internal hydrocephalus is where the excess fluid accumulates. Internal hydrocephalus is characterized by fluid accumulation within the brain ventricles (ventricles), while mixed hydrocephalus can involve both internal and external components. Diagnosis may include an MRI or CT scan of the brain to determine the location of the excess fluid.
- Communicating and noncommunicating hydrocephalus: To distinguish mixed hydrocephalus from other forms, such as communicating or noncommunicating hydrocephalus, it is necessary to examine the cerebral spinal fluid pathways and determine if there are blockages or obstructions in them.
- Brain tumors: Brain tumors can cause compression of brain structures and increased intracranial pressure, which can also have symptoms similar to hydrocephalus. An MRI or CT scan of the brain, as well as a tumor biopsy, may be needed to differentiate.
- Inflammatory diseases: Diseases such as meningitis or inflammation of the brain membranes may have similar symptoms to hydrocephalus. Diagnosis may include analysis of cerebrospinal fluid and laboratory tests.
- Hypertension and hypotension: High or low intracranial pressure can also have symptoms similar to hydrocephalus. Intracranial pressure measurements may be needed to differentiate.
These are just a few possible conditions that can mimic the symptoms of mixed hydrocephalus. Diagnosis and differential diagnosis should be made by experienced medical professionals using a variety of examination techniques to accurately determine the cause and form of hydrocephalus and to develop the most appropriate treatment plan.
Treatment of the mixed hydrocephalus
Treatment of mixed hydrocephalus depends on its cause and severity, as well as the condition and age of the patient. Treatment usually involves surgical techniques, as it is a chronic condition associated with impaired drainage or circulation of cerebral spinal fluid (CSF). Here are some of the main treatments for mixed hydrocephalus:
- Shunt placement: This is the most common treatment for hydrocephalus. A shunt is a medical device that is inserted inside the brain and/or ventricles of the brain and directs excess cerebral spinal fluid to another location in the body, usually the abdomen. Shunts can be of different types, and the choice of a particular type depends on the specifics of the case.
- Endoscopic tertiary ventricular resection: This method involves using an endoscopic technique to remove an obstruction or tumor that may be blocking the normal movement of cerebral spinal fluid within the brain.
- Endoscopic third ventricular window: This technique creates an artificial opening in the third ventricle of the brain to facilitate drainage of cerebral spinal fluid and improve circulation.
- Other surgical techniques: In some cases, other surgical procedures may be required, including correction of anomalies, removal of infections, or bypassing areas that block CSF circulation.
Treatment of mixed hydrocephalus should be individualized and performed by experienced neurosurgeons. After the surgical procedure, medical rehabilitation and long-term follow-up with physicians may be required to monitor the patient's condition and identify possible complications. It is important to consult a physician for advice and to develop the best treatment plan for each individual case. [7]
Forecast
The prognosis of mixed hydrocephalus depends on several factors, including the cause of the hydrocephalus, the extent of brain damage, the age of the patient, and the timeliness and effectiveness of the treatment provided. The overall prognosis can vary from case to case. Here are a few possible outcomes:
- Improvement: With successful and timely treatment, many patients with mixed hydrocephalus can achieve stabilization or improvement. Treatment may include surgical procedures to remove blockages or other causes of hydrocephalus. After successful treatment, symptoms may decrease or even disappear completely, and the patient can return to normal life.
- Permanent symptoms: In some cases, mixed hydrocephalus can lead to permanent symptoms and limitations in neurological function. This can happen if the brain damage is too severe or if treatment is ineffective.
- Complications: Hydrocephalus can cause various complications such as infections, visual impairment, developmental disorders in children, and long-term neurologic sequelae. The prognosis may be less favorable if complications cannot be controlled.
- Need for long-term care: In some cases, patients with mixed hydrocephalus may need long-term care and rehabilitation, especially if they have motor and mental impairment.
The prognosis may also depend on the age of the patient. Children whose hydrocephalus is diagnosed and treated early have a better chance of successful recovery and development of normal neurological functions.
It is important to realize that the prognosis of mixed hydrocephalus can be improved with timely diagnosis, proper treatment, and medical management. Patients and their families should cooperate with medical professionals and follow recommendations for best outcomes.

