Medical expert of the article
New publications
Normotensive hydrocephalus.
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
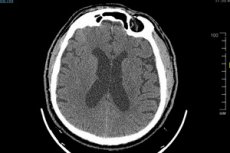
Normotensive hydrocephalus (normal intracranial pressure hydrocephalus) is a form of hydrocephalus in which the level of intracranial pressure (ICP) remains within normal limits, not increased. Hydrocephalus is generally characterized by the accumulation of excess cerebral spinal fluid (CSF) in the cerebral ventricles (ventricles) or brain space, which can lead to an increase in the volume of the skull and elevated IOP.
In normotensive hydrocephalus, the level of IOP remains normal and there is no increase in pressure inside the skull, which distinguishes this form of hydrocephalus from other, more common, forms in which pressure is usually elevated.
Symptoms of normotensive hydrocephalus may include headaches, nausea, vomiting, behavioral changes, impaired attention and concentration, impaired coordination of movements, and even neurological deficits. These may be less severe than other forms of hydrocephalus, but still require attention and diagnosis.
The causes of normotensive hydrocephalus can vary and include a variety of factors such as congenital brain abnormalities, abnormalities of the CSF resorption system, brain tumors, inflammation, head trauma, and others. An extensive physical examination, including MRI or CT scans of the brain and other diagnostic techniques, is usually required to make an accurate diagnosis and select the best treatment.
Treatment of normotensive hydrocephalus depends on its cause and symptoms and may include surgery, drug therapy, or other modalities depending on the clinical presentation of each case.
Causes of the normotensive hydrocephalus.
The causes of normotensive hydrocephalus are not always fully understood, but they may include the following factors:
- Age: Normotensive hydrocephalus is more common in the elderly, although it can occur in younger patients. The elderly are more susceptible to abnormalities in CSF circulation and resorption, which may contribute to the development of hydrocephalus.
- Delayed effects of trauma: Some cases of normotensive hydrocephalus may be associated with head injuries that occurred many years ago. These injuries can cause changes in CSF circulation and lead to CSF accumulation.
- Inflammatory processes: Sometimes normotensive hydrocephalus can result from inflammatory diseases of the brain or spinal cord, such as meningitis or encephalitis.
- Vascular disorders: Vascular abnormalities such as hypertension (high blood pressure) or cerebral vascular disease can impair CSF circulation and resorption and contribute to the development of hydrocephalus.
- Genetic factors: Hereditary factors may play a role in the development of normotensive hydrocephalus, although the exact genetic mechanisms are not always known.
Pathogenesis
The pathogenesis of normotensive hydrocephalus is not completely clear and may be diverse. Possible mechanisms for the development of normotensive hydrocephalus may include the following:
- Increased cerebral fluid production: One possible mechanism for normotensive hydrocephalus is increased cerebral fluid production. This may be due to hyperproduction of fluid by well-located glands such as the cerebellar yellow nucleus.
- Increased vascular resistance: Another mechanism involves changes in the blood vessels that can make it difficult for cerebral fluid to drain normally. This can be caused by changes in the blood vessels, the brain's ability to absorb brain fluid, or other factors that affect the circulation of brain fluid.
- Increased absorption: Some studies suggest that in normotensive hydrocephalus, there may be increased absorption of cerebral fluid within the cranial cavity, which may contribute to its accumulation.
- Genetic factors: In some cases of normotensive hydrocephalus, there may be a genetic predisposition, although the exact genetic mechanisms are not always understood.
Symptoms of the normotensive hydrocephalus.
Symptoms of normotensive hydrocephalus can include a variety of manifestations characterized by changes in brain function. It is important to note that symptoms may vary depending on the specific case and the severity of the hydrocephalus. Below are some possible symptoms of normotensive hydrocephalus:
- Headaches: Headaches can be one of the most common symptoms. They can occur due to an increase in the volume of the brain ventricles and an increase in intracranial pressure.
- Disorders of mental function: Irritability, behavioral changes, psychomotor slowing, poor concentration, and memory impairment may be associated with normotensive hydrocephalus.
- Nausea and vomiting: Increased pressure in the brain can affect the centers that regulate nausea and vomiting, which can lead to frequent episodes of nausea and vomiting.
- Movement disorders: This may include weakness in the limbs, impaired coordination of movement, unsteadiness when walking, and difficulty with muscle control.
- Visual and auditory disturbances: Visual problems, including double or blurred vision and decreased hearing, may be associated with normotensive hydrocephalus.
- Neurologic symptoms: These may include seizures, neurologic abnormalities, and changes in reflexes.
The triad of normotensive hydrocephalus is a set of clinical features that characterize the normotensive (normal intracranial pressure) form of hydrocephalus. The triad includes the following signs:
- Sensomotor disorders: Patients may experience sensory changes, weakness, spasticity (increased muscle tone), and other motor impairments.
- Hydrocephalus: This is the main sign of hydrocephalus. The ventricles of the brain fill with excess CSF, which can lead to increased head volume and other symptoms.
- Mental Disorders: Patients may also experience mental symptoms such as behavioral changes, psychomotor delay, cognitive impairment, and other mental disorders.
The triad can be caused by a variety of reasons, and accurate diagnosis and treatment usually requires consultation with a neurosurgeon and appropriate tests such as a computed tomography (CT) scan or magnetic resonance imaging (MRI) of the head.
It is important to note that the symptoms of normotensive hydrocephalus can be similar to those of other medical conditions, so an accurate diagnosis and treatment plan should be developed by an experienced medical professional.
Complications and consequences
Normotensive hydrocephalus (NPH) can cause a variety of complications and have serious consequences, especially if not detected and treated in time. The main complications and consequences of NPH include:
- Worsening neurological symptoms: The main symptoms of NPH are changes in walking (stumbling), pseudobulbar syndrome (impaired articulation of speech and swallowing), and increased urination. The complication is that these symptoms can worsen over time and lead to more severe motor and speech impairment.
- Cognitive deterioration: Some patients with NPH experience deterioration of cognitive functions such as memory, attention, and problem-solving abilities. This can lead to dementia or worsen existing dementia (e.g. Alzheimer's disease).
- Falls and Injuries: Due to impaired coordination and impaired walking, patients with NPH are at increased risk for falls and injuries, which can lead to fractures and other serious injuries.
- Deterioration of quality of life: All of the above complications and symptoms of NPH can significantly impair patients' quality of life and make them dependent on outside help.
- Depression and social isolation: Deteriorating health conditions and limited mobility can cause depression and social isolation in patients with NPH.
Diagnostics of the normotensive hydrocephalus.
Diagnosing normotensive hydrocephalus may involve several steps and medical procedures to determine if this condition is present and to identify its causes. Here are some basic methods for diagnosing normotensive hydrocephalus:
- Clinical Examination: The physician will perform an initial clinical examination of the patient, including gathering medical and family history, as well as eliciting and characterizing symptoms.
- Neurologic exam: Your doctor may perform a neurologic exam to assess neurologic function, including motor coordination, balance, vision, and others.
- Imaging education:
- Magnetic Resonance Imaging (MRI): MRI is a commonly used technique to visualize the brain and determine the volume of brain fluid, its distribution, and whether there are obstructions in its circulation. MRI can help identify changes inside and outside the skull.
- Computed tomography (CT): CT scans can also be used to visualize the brain and identify abnormalities, blockages, or changes associated with hydrocephalus.
- Cerebral spinal fluid analysis: Performing a lumbar puncture (spinal tap) with cerebral spinal fluid analysis may be necessary to detect infections or other pathologies that may cause hydrocephalus.
- Other tests: Additional tests and examinations may be needed to determine the cause of normotensive hydrocephalus, such as tests for infections, biochemical tests, and others.
Diagnosing normotensive hydrocephalus can be complex and requires the collaboration of various specialists, including neurosurgeons and neurologists. Once a diagnosis is made, doctors can determine appropriate treatment depending on the cause and severity of the hydrocephalus.
Differential diagnosis
The differential diagnosis of normotensive hydrocephalus requires ruling out other possible causes of symptoms that may mimic this condition. The following are some conditions and diseases to consider in the differential diagnosis of normotensive hydrocephalus:
- High or low intracranial pressure: Elevated or low IOP can cause symptoms similar to hydrocephalus. IOP measurements are required to differentiate between the two.
- Migraine: Migraine headaches can mimic the headaches that often accompany normotensive hydrocephalus. However, migraines are more often accompanied by characteristic features such as aura, photophobia, and auditory hypersensitivity.
- Brain tumors: Brain tumors can cause an increase in brain volume, which can lead to hydrocephalus. An MRI or CT scan of the brain and other examination methods may be required to differentiate between the two.
- Inflammatory diseases: Inflammatory processes such as meningitis or encephalitis may present with symptoms similar to hydrocephalus. Cerebrospinal fluid analysis and laboratory tests can help in the differential diagnosis.
- Other brain abnormalities: Congenital brain abnormalities such as cerebral palsy (cerebral palsy) or hydrocephalus with another cause can also mimic the symptoms of normotensive hydrocephalus.
- Trauma and Strokes: Head injuries and strokes can cause changes in brain structures and intracranial pressure, which can be similar to hydrocephalus.
Treatment of the normotensive hydrocephalus.
Treatment of normotensive hydrocephalus (NPH) usually involves surgical techniques because it is a chronic condition associated with a buildup of cerebral spinal fluid (CSF) inside the cranial cavity at normal or near-normal pressures. The main treatment for NPH is the placement of a shunt to help drain excess CSF from the brain. Here is more information about treating NPH:
- Shunt placement: This is the most common treatment for NPH. Doctors place a shunt (tube) that connects the ventricles of the brain to another part of the body, usually the abdomen. This gets rid of excess CSF and restores normal pressure inside the skull.
- Liquorodynamic studies: Occasionally, liquorodynamic studies, including liquorodynamic cisternography and a walk time test, are performed to make an accurate diagnosis and determine if the patient is suitable for surgical treatment.
- Medical Rehabilitation: After shunt placement, patients may require medical rehabilitation to restore physical and neurological functions such as walking and speech.
- Long-term follow-up: Patients who have undergone surgical treatment for NPH should be under regular medical supervision to monitor the condition and function of the shunt and to address any problems that arise.
NPH treatment should be individualized for each patient, and the need for and method of treatment should be decided by physicians based on symptoms, examination findings, and the patient's overall condition. Effective treatment of NPH can improve a patient's quality of life and prevent the progression of symptoms.
Forecast
The prognosis of normotensive hydrocephalus can be varied and depends on several factors, including the cause of the hydrocephalus, the extent of brain damage, the patient's age, the effectiveness of treatment, and the presence of complications. Below are some possible outcomes of normotensive hydrocephalus:
- Improvement: With successful and timely treatment, many patients with normotensive hydrocephalus can achieve stabilization or improvement. Treatment may include surgical procedures to facilitate the outflow of brain fluid or medication to manage symptoms. After successful treatment, symptoms may decrease or even disappear completely.
- Permanent symptoms: In some cases, normotensive hydrocephalus can lead to permanent symptoms and limitations in neurological function. This can happen if the brain damage is too severe or if treatment is ineffective.
- Complications: Hydrocephalus can cause various complications such as infections, visual impairment, developmental disorders in children, and long-term neurologic sequelae. The prognosis may be less favorable if complications cannot be controlled.
- Need for long-term care: In some cases, patients with normotensive hydrocephalus may need long-term care and rehabilitation, especially if they have motor and mental impairment.
The prognosis may also depend on the age of the patient. Children whose hydrocephalus is diagnosed and treated early have a better chance of successful recovery and development of normal neurological functions.
It is important to realize that the prognosis of normotensive hydrocephalus can be improved with timely diagnosis, proper treatment and medical management.

