Subaortic stenosis
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
In hypertrophy and other myocardial defects in the area of the interventricular septum, blood transportation to the aorta is impaired. This area precedes the area of the aortic valve, so this narrowing is characterized as subaortic outflow tract stenosis. In patients at the moment of contraction of the left ventricle there is an obstruction that prevents blood flow, which is manifested by dizziness, impaired consciousness and breathing. Treatment can be either conservative or surgical, depending on the form and clinical picture of the disease.
Idiopathic hypertrophic subaortic stenosis
If the causes of subaortic stenosis cannot be identified, and it is also impossible to find a relationship between the development of pathology and any damaging and hereditary factors, then such a disease is called idiopathic.
The term is applied to stenosis provoked by unspecified causes or spontaneous stenosis.
Speaking of hypertrophic subaortic stenosis, they mean abnormal overgrowth of myofibrils, which can manifest itself in the following forms:
- Annular hypertrophic stenosis (has the appearance of a collar covering the canal);
- Semilunar hypertrophic stenosis (has a ridge shape on the septum or mitral valve leaflet);
- Tunnel stenosis (the entire left ventricular outflow tract is affected).
Anatomical variants
There is a spectrum of variants of subvalvular aortic stenosis occurring in isolation or in combination with others. They are as follows:
- Thin discrete membrane: the most common lesion
- Muscular fibrous ridge.
- Diffuse fibrotic muscular tunnel-like narrowing of the left ventricular outflow tract (LVOT). [1], [2]
- Additional or abnormal mitral valve tissue
In most patients, obstruction is caused by a membrane attached to the interventricular septum or encompassing the left ventricular outflow tract. [3], [4], [5] Its position can be anything from directly under the aortic valve to the left ventricle. It is noted that the base of the aortic valve flaps is involved in this subaortic tissue, which limits mobility and dilates the left ventricular outflow tract.
Epidemiology
Subvalvular aortic stenosis is a rare condition seen in infants and neonates, but is the second most common type of aortic stenosis. It is responsible for approximately 1% of all congenital heart defects (8 in 10,000 newborns) and 15% to 20% of all fixed obstructive lesions of the left ventricular outflow tract.
Children with congenital aortic stenosis have 10 to 14% of cases of subvalvular aortic stenosis. It is more common in males and ranges from 65% to 75% of cases, [6], [7] with a male to female ratio of 2:1. The prevalence of subvalvular aortic stenosis is 6.5% of all adult congenital heart disease. [8]
One-valve aortic stenosis is associated with other cardiac malformations in 50-65% of cases. [9] In a report of 35 patients, concomitant lesions were found.
- Ventricular septal defect (VSD) (20%)
- Open ductus arteriosus (34%)
- Pulmonary stenosis (9%)
- Coarctation of the aorta (23%)
- Various other lesions (14%)
Among all left ventricular outflow tract obstructions, subaortic stenosis occurs in approximately 10-30% of cases.
It is noted that the problem occurs more often in men (one and a half to two times more often than in women).
Associated pathologies in most cases are:
- Bicuspid aortic valve;
- Aortic valve stenosis;
- Coarctation of the aorta;
- Open ductus arteriosus;
- Interventricular septal defect;
- Fallot's tetrad;
- Complete atrioventricular communication.
Approximately 20-80% of patients with congenital subaortic stenosis have concomitant congenital heart disease, and 50% are diagnosed with increasing aortic valve insufficiency, which is associated with hemodynamic abnormalities. In addition, subaortic stenosis may be one of the manifestations of Schon's complex.
Congenital isolated stenosis is a rare diagnosis among newborn infants and children in the first year of life. At older ages, the pathology may exist latently for many years. However, after the age of 30, congenital subaortic stenosis is virtually uncommon. [10]
Causes of the subaortic stenosis
Many mechanisms contribute to the development of fixed subvalvular aortic stenosis, such as genetic factors, hemodynamic abnormalities seen in other cardiac lesions, or underlying left ventricular outflow tract morphology that increases turbulence in the outflow tract. [11] Various defects (mostly congenital) can cause the development of subaortic stenosis. In particular, such defects may include:
- Improper attachment of the anterior mitral valve leaflet to the interventricular membrane, mitral valve or chordal abnormalities;
- Thickening, thickening of the mitral valve with the formation of mechanical obstruction;
- Isolated divergence of the anterior mitral valve leaflet with chordae;
- Parachute-shaped mitral valve curvature;
- Hypertrophy of the left ventricular outflow tract musculature;
- Fibrous thickening below the aortic valve with circulatory coverage of the left ventricular outflow tract, etc.
Pathologic changes can affect both the subvalvular structures of the aortic valve and nearby anatomic elements (e.g., mitral valve). [12]
Risk factors
The main factor in the development of subaortic stenosis is a genetic disorder. Hereditary forms of the disease are accompanied by a deficiency in the formation of myocardial contraction proteins. Idiopathic spontaneous subaortic stenosis is not uncommon.
In most cases, specialists mention the following provoking factors:
- Interventricular septal hypertrophy;
- Metabolic disorders, including diabetes mellitus, thyrotoxicosis, obesity, and amyloidosis;
- Chemotherapy treatment;
- Use of anabolics, narcotics;
- Connective tissue diseases;
- Bacterial and viral infectious pathologies;
- Chronic alcohol dependence;
- Radiation exposure, including radiation treatment;
- Sports heart syndrome.
Subaortic stenosis due to hypertrophy of the interventricular septum leads to persistent circulatory failure. At the moment of contractile activity, blood is transported between the valve leaflet and the septum. Due to insufficient pressure, there is greater overlap of the mitral valve of the left ventricular outflow tract. As a result, not enough blood flows into the aorta, pulmonary outflow is impeded, cardiac and cerebral deficit develops, and arrhythmia develops.
Pathogenesis
Congenital subaortic stenosis is accompanied by structural changes in the subvalvular space of the aortic valve, or by developmental defects in nearby structures, such as the mitral valve.
Membranous diaphragmatic stenosis may be due to the presence of a circular fibrous membrane with holes in the left ventricular outflow tract or a fibrous sulcus fold that reduces more than half of the left ventricular outflow tract. The membranous orifice may be as large as 5-15 mm. In most cases, the membrane is localized immediately below the fibrous ring of the aortic valve, or slightly below, and is attached along the base of the anterior mitral valve leaflet to the interventricular septum below the right coronary or noncoronary leaflet.
Valvular subaortic stenosis is manifested by a fibrotic thickening of a valvular type, with localization 5-20 mm below the aortic valve.
Fibromuscular subaortic stenosis is a peculiar thickening, similar to a "collar", localized 10-30 mm below the aortic valve, in contact with the anterior mitral valve leaflet, "hugging" the left ventricular outflow tract like a semilunar roll. The narrowing can be quite long, up to 20-30 mm. The pathology is often detected against the background of hypoplasia of the valve fibrous ring and changes in the side of the valve flaps.
Tunnel-shaped subaortic stenosis is the most pronounced type of this pathology, which is characterized by intense hypertrophic changes in the musculature of the left ventricular outflow tract. As a result, a fibrous-muscular tunnel 10-30 mm long is formed. Its lumen is narrowed, which is associated with dense fibrous layering. The left ventricular musculature is hypertrophied, subendocardial ischemia, fibrosis, sometimes severe hypertrophy of the interventricular septum (compared to the posterior left ventricular wall), and histologically disoriented muscle fibers are noted. [13]
Symptoms of the subaortic stenosis
The severity and intensity of the clinical picture depends on the degree of narrowing of the alimentary canal. The following first signs are most often recorded:
- Periodic episodes of blurred consciousness, semi-fainting and fainting;
- Shortness of breath;
- Chest pain (episodic or constant);
- Heart rhythm disturbances;
- Tachycardia, palpitations;
- Dizziness.
Symptomatology increases against the background of physical exertion, overeating, alcohol consumption, excitement, fear, sudden change of body position. Heart pain is similar to angina pectoris, but in subaortic stenosis, taking nitrates (Nitroglycerin) does not relieve, but increases pain.
Over time, the pathology worsens. In the course of medical examination, left-sided displacement of the apical tremor, its bifurcation or amplification is detected. In the area of the carotid arteries, the pulse is two-wave (dicrotic), prone to rapid increase. Due to increased venous pressure, the cervical vessels are dilated, the lower extremities swell, there is an accumulation of fluid in the abdominal cavity (ascites) and in the pleural cavity (hydrothorax).
Heart murmur is auscultated at the moment of systole over the apex, its loudness increases in the upright position, on inhalation and during breath-holding. [14]
Complications and consequences
Specialists talk about several characteristic variants of the course of subaortic stenosis:
- In a benign course, patients feel satisfactory, and diagnostic measures do not reveal obvious hemodynamic disorders.
- With a complex progressive course, patients note increasing weakness, increasing cardiac pain, the appearance of dyspnea at rest, periodic fainting.
- The terminal stage is accompanied by the development of severe circulatory failure.
The most common complications are:
- A bout of heart palpitations (tachycardia);
- Extrasystole;
- Atrial fibrillation and threatening cerebral embolism;
- Sudden cardiac arrest.
Diagnostics of the subaortic stenosis
At the initial diagnostic stage, symptomatology is assessed, palpation and percussion of the heart zone and neck vessels are performed. In subaortic stenosis, it is possible to detect percussive expansion of cardiac borders to the left due to left ventricular hypertrophy, as well as palpation - blurring of the apical tremor. Palpation may reveal systolic tremor at the cardiac base with continuation along the carotid arteries.
Auscultation reveals:
- Coarse systolic murmur dominating in the second intercostal space on the right side, radiating to the carotid arteries;
- Diastolic regurgitation murmur at the aortic valve.
The following tests are recommended: coagulogram, platelet count to predict the risk of perioperative bleeding and the amount of blood loss. In addition, a hematologic study is performed to detect anemia. [15]
Instrumental diagnosis involves the use of such techniques:
- Chest X-ray with determination of the heart size (in subaortic stenosis the heart is enlarged, acquires a spherical configuration);
- Electrocardiography (subaortic stenosis is accompanied by signs of left ventricular muscle hypertrophy, appearance of deep Q teeth, ST decrease, T abnormality in the first standard lead, V5, V6; dilated P in the second and third leads as a result of enlarged left atrium is detected);
- Holter electrocardiography (to detect tachycardic attacks, atrial fibrillation, extrasystoles);
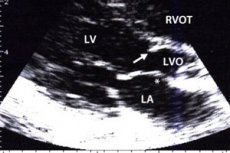
- Ultrasound (in subaortic stenosis, the septum is 1.25 times thicker than the left ventricular wall; there is insufficient left ventricular capacity, decreased blood flow through the aortic valve, closure of the latter in the middle of systole, and left atrial cavity dilation);
- Cardiac probing (changes in inspiratory breath-hold pressure, increases in final diastolic pressure);
- Ventriculography, angiography (reveals a problem with blood escaping into the aorta at the time of left ventricular contraction).
Differential diagnosis
Differential diagnosis in some cases is performed between congenital subaortic stenosis and hypertrophic cardiomyopathy with impaired outflow from the left ventricle. The obtained diagnostic results play an important role in the choice of subsequent therapeutic tactics.
Who to contact?
Treatment of the subaortic stenosis
The difficulty lies in the fact that surgical intervention for subaortic stenosis is always highly traumatic and associated with increased life risks, and conservative therapy does not always lead to the desired effect.
In order to reduce cardiac load, improve left ventricular function, it is possible to prescribe such drugs:
- β-blockers (Anapriline, with a gradual increase in daily dosage from 40 to 160 mg);
- Calcium channel inhibitors (Isoptin);
- Antiarrhythmic drugs (Cordarone).
If there is a threat of inflammatory complications (e.g., endocarditis), antibiotic therapy with cephalosporin antibiotics (Cefazolin) or aminoglycosides (Amikacin) may be prescribed. [16]
These common medications are not recommended for subaortic stenosis:
- Diuretics;
- Nitroglycerin;
- Cardiac glycosides;
- Dopamine, Adrenaline;
- Vasodilators.
With severely ongoing pathology and the lack of effect from conservative therapy, with pressure differences in the ventricle and aorta more than 50 mm Hg, doctors can raise the question of surgical intervention, in particular:
- Mitral valve prosthesis to optimize ventricular performance;
- Myoectomy - excision of myocardium to improve septal function.
Among the alternative methods, placement of a pacemaker or cardioverter is leading.
Treatment is necessarily supplemented by changes in the diet of the patient. Recommended:
- Eat often and small meals without overeating;
- Exclude salt, animal fats, spicy spices and seasonings (to improve the vascular system);
- Limit fluid intake to 800-1000 ml per day;
- Eliminate alcoholic beverages, sodas, coffee and strong tea;
- In the diet give preference to vegetarian soups, porridge and stewed vegetables, boiled sea fish, dairy products, fruits, nuts, herbs and berries.
The criteria and timing of surgical intervention in subvalvular aortic stenosis are controversial. Early intervention in these patients is counterbalanced by a high incidence of postoperative recurrences, late reoperations and development of aortic regurgitation after obstruction relief. [17], [18]
- In children and adolescents with an average Doppler gradient of less than 30 mm Hg and no left ventricular hypertrophy, treatment of subvalvular aortic stenosis consists of non-intervention and medical monitoring.
- In children and adolescents with a Dopplerometric mean gradient of 50 mmHg or more, surgical treatment is necessary.
- Children and adolescents with mean Doppler gradients of 30 to 50 mm Hg may be considered for surgical intervention if they have symptomatic angina, syncope, or dyspnea on exertion, if they are asymptomatic but develop changes on resting or exercise ECG, or at older ages. At diagnosis. [19]
- Prevention of aortic regurgitation alone is not usually a criterion for surgical intervention. However, progression and worsening of regurgitation to a significant degree is an indication for surgical intervention.
Prevention
Hereditary forms of subaortic stenosis cannot be prevented, but preventive measures are necessary to prevent the development of complications of the disease. First of all, it is necessary to monitor physical activity, avoid overloading, avoid strength training and other exercises that increase the risk of hypertrophic changes in the myocardium.
Any exercise is canceled if the following changes are detected:
- A clear pressure mismatch in the left heart;
- Marked myocardial hypertrophy;
- Ventricular or supraventricular arrhythmia;
- Cases of sudden death among direct relatives (cause of death may be undetermined, or the result of cardiomyopathy with hypertrophy).
In case of systematic weakness, dizziness, pain on physical exertion, shortness of breath, it is necessary to consult a doctor. In case of hereditary predisposition, it is recommended to undergo annual preventive diagnostics, including ultrasound, electrocardiography and ventriculography. It is desirable throughout life to follow a diet with restriction of salt and animal fats, as well as with a fractional diet. It is important to constantly monitor physical activity, do not overload the body with strength training, exercise only under the supervision of a doctor and trainer.
Prophylactic measures to prevent the development of subaortic stenosis are closely related to the prevention of atherosclerosis, rheumatism, and infectious inflammatory lesions of the heart. Patients with cardiovascular diseases are subject to medical examination, as they require regular monitoring by a cardiologist and rheumatologist.
Forecast
Subaortic stenosis is sometimes latent, without any pronounced symptoms, for many years. When obvious clinical manifestations appear, there is a significant increase in the probability of complications, including lethal outcome. Among the main unfavorable signs:
- Angina;
- Pre-syncope, fainting;
- Left ventricular failure (usually in such situations, the five-year survival rate is two to five years).
Infants and children should be monitored frequently (every 4-6 months) to understand the rate of progression because subvalvular aortic stenosis is a progressive disease.
Survival in patients who have undergone subaortic membrane excision surgery is excellent, but these patients must be monitored because the left ventricular outflow tract gradient slowly increases over time. Long-term follow-up of postoperative patients is important. Most patients will require reoperation at some point in their lives because of recurrence. [20]
Independent predictors of increased reoperation rates are as follows:
- Female gender
- Peak instantaneous LVOT gradient progression over time
- Difference between preoperative and postoperative peak instantaneous LVEF gradients
- Preoperative peak instantaneous LV gradient greater than or equal to 80 mm Hg.
- Age over 30 at the time of diagnosis
With the development of left ventricular insufficiency and with timely surgical intervention, five-year survival is reported in more than 80% of cases, and ten-year survival in 70% of cases. Complicated subaortic stenosis has an unfavorable prognosis.

