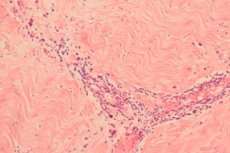
Rheumatic pericarditis
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
In people with systemic diseases - including rheumatic diseases - the inflammatory process can spread to the structures of the heart, and when the surrounding connective tissue lining (pericardium) is affected, rheumatic pericarditis develops. [1]
Epidemiology
According to clinicians and researchers:
- Each year, acute rheumatic fever is diagnosed in about 325,000 children (mostly in developing countries), and pericarditis occurs in 5-10% of patients with rheumatic fever;
- Rheumatic heart disease affects 35-39 million people worldwide;
- Rheumatic pericarditis occurs in 30-50% of patients with rheumatoid arthritis, 20-50% of patients with SLE, and 17% of patients with systemic scleroderma.
Causes of the rheumatic pericarditis
First of all, the key causes of rheumatic pericarditis are related to chronic rheumatic diseases of a systemic nature: inflammatory damage to the heart muscles and valves - rheumocarditis or rheumatic heart disease, rheumatoid or rheumatic arthritis and polyarthritis.
This group of diseases, which are autoimmune inflammation of connective tissue of the cardiovascular system, joints, and other organs, are collectively a consequence of acute rheumatic fever, which occurs when affected by a streptococcal infection - a dozen rheumatogenic strains of group A beta-hemolytic streptococcus (Streptococcus pyogenes). [2]
In some cases, rheumatic fever causes long-term heart damage inflammation of all the heart membranes - pancarditis - which can lead to pericarditis, myocarditis and endocarditis. [3]
In addition, rheumatic pericardial lesions may be a consequence of an autoimmune disease such as systemic lupus erythematosus (SLE), chronic polysystemic behçet's disease, scleroderma, sjögren's syndrome, genetically determined familial Mediterranean fever.
Read also:
Risk factors
All the diseases listed above are risk factors for the development of rheumatic pericarditis. And their occurrence, in turn, is most often due to untreated or under-treated streptococcal infections, in particular chronic tonsillitis (sore throat), pharyngitis, scarlatina, after which three to four weeks later in 3-6% of cases acute rheumatic fever appears.
Rheumatism can occur at any age, but it usually affects children between the ages of 5-15.
There is an increased likelihood of rheumatic lesions of the pericardial pouch in case of genetic propensity, as well as predisposition to inflammatory diseases of an autoimmune nature - with an increased reaction (hypersensitivity) of the immune system. [4]
Pathogenesis
In cases of rheumatic pericarditis, the pathogenesis of the lesion of the outer connective tissue membrane of the heart lies in the fact that there is a similarity between a group of cells (epitope) of Streptococcus pyogenes group A antigens (streptococcal surface proteins M) and several protein cells of the cardiac membrane tissues, causing a type II and III hypersensitivity reaction of the immune system. That is, after interacting with group A staphylococcus in some people, the protective cells of the humoral immune system begin to attack the pericardial tissue cells that they mistake for bacterial proteins. And this mechanism is called molecular mimicry.
In this case, mature antigen-presenting B cells (B-lymphocytes) present bacterial antigen to T-helper cells (Th2 and CD4+T cells), and they release inflammatory mediators (cytokines), promote the growth of cytotoxic T-leukocytes and increase the activity of other immune cells - phagocytes (macrophages and neutrophils). [5]
Th2 cells then transform into plasma cells and induce the production of antibodies (globular proteins or immunoglobulins) against bacterial cell wall proteins. But at the same time - because of the unique host response to the specific streptococcal antigen - the antibodies affect myocardial, endocardial and pericardial tissues of the heart, initiating their inflammation.
So, acute rheumatic fever, rheumatic heart disease and rheumatic pericarditis are thought to be the result of an autoimmune response. [6]
Symptoms of the rheumatic pericarditis
Specialists distinguish such types of this pathology as:
- Rheumatic acute pericarditis;
- Rheumatic chronic pericarditis;
- Rheumatic serous pericarditis;
- Rheumatic serous-fibrinous or fibrinous pericarditis;
- Rheumatic exudative pericarditis;
- Compressive or constrictive rheumatic pericarditis (resulting in loss of the normal elasticity of the pericardial sac).
Ultrasound and other imaging methods of cardiac examination can determine the volume of abnormal fluid accumulation in the pericardial cavity - pericardial cavity effusion, which may be minor, moderate or significant.
And the four stages of the disease (diffuse ST segment elevation in all leads, pseudonormalization. Inverted T-notches and normalization) are determined by specialists on ECG.
In most cases, the first signs of rheumatic pericarditis are manifested by a feeling of heaviness and pressure in the heart area, general weakness, dizziness and shortness of breath.
Other symptoms include left-sided chest pains of varying duration and intensity (often irradiating to the subclavian and other areas), sinus tachycardia at rest, edema, increased jugular vein pressure, and decreased blood pressure.
Patients with acute rheumatic pericarditis have sharp pain behind the sternum, which is relieved by sitting or bending forward. In almost all cases, a pericardial friction murmur is heard. [7]
All details in the publication - symptoms of pericarditis
Complications and consequences
Complications and consequences of rheumatic pericardial lesion are congestive heart failure, formation of foci of calcinosis in the pericardium, as well as compression effect on the heart (due to the accumulation of effusion and increased pressure in the pericardial cavity) and circulatory failure due to decreased cardiac output and systemic venous stasis - cardiac tamponade [8] and cardiogenic obstructive shock. [9]
Diagnostics of the rheumatic pericarditis
Read: diagnosing pericarditis
Blood tests: general, COE, serum level of C-reactive protein, urea nitrogen and creatinine, IgM autoantibodies (rheumatoid factor), antibodies to streptolysin - titer antistreptolysin O ), antibodies to Streptococcus pyogenes enzymes (streptokinase, hyaluronidase, etc.). Laboratory examination of pericardial fluid is also performed.
Instrumental diagnostics is performed: ECG, transthoracic EchoCG, chest X-ray, CT and MRI of the mediastinal region, pericardioscopy. More information in the publication - instrumental methods of cardiac examination
Differential diagnosis
The differential diagnosis includes rheumocarditis, endocarditis, myocarditis, other types of pericarditis, aortic dissection with traumatic effusion into the pericardial cavity, and myocardial infarction.
Who to contact?
Treatment of the rheumatic pericarditis
Read the article - treating Pericarditis
What medications are used for rheumatic pericarditis?
Pain is usually managed with non-steroidal anti-inflammatory drugs: Aspirin (Acetylsalicylic acid), Indomethacin, Ibuprofen and others.
The anti-inflammatory drug Colchicine (taken orally, twice a day - 0.5 mg) is most often prescribed to patients with acute pericarditis.
Systemic corticosteroids that suppress immune and inflammatory reactions are used: low-dose injections of Prednisolone, Betamethasone or Diprospan, taking tablets containing methylprednisolone, etc.
In recurrent pericarditis of rheumatic etiology, injectable interleukin IL-1 antagonist drugs can be used: Anakinra, Rilonacept, Canakinumab.
In cases with serologic evidence of recent streptococcal infection, an intravenous antibiotic (Penicillin) is indicated.
If the volume of pericardial effusion is small and without any symptoms, the patient undergoes periodic ultrasound examination. But when the effusion impairs cardiac function and causes cardiac tamponade, the pericardial cavity should be drained by pericardial puncture, pericardiocentesis.
Surgical treatment involves removal of the effusion through the pericardial window, which is done by dissecting the pericardium with temporary placement of a drainage catheter to prevent cardiac tamponade.
In addition, severe cases of constrictive pericarditis of rheumatic etiology may require pericardectomy, during which the visceral and parietal layers of the pericardium are removed to restore normal ventricular filling dynamics.
Prevention
The pathogenesis as well as susceptibility to rheumatic fever has not been fully elucidated, and its primary prevention is impossible due to the lack of a suitable vaccine. So it is possible to prevent the development of diseases associated with beta-hemolytic streptococcus group A only through their timely treatment. It is also necessary to monitor the state of the cardiovascular system in patients with autoimmune pathologies.
Forecast
The prognosis of rheumatic pericarditis is worsened by the high recurrence rate and the difficulty in controlling symptoms. In addition, pericarditis of this etiology is usually associated with acute rheumatic involvement of all layers of the heart, i.e. Rheumatic myocarditis and endocarditis are likely to be present. Fatal cardiac tamponade is also likely to occur.

