Influenza A virus
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
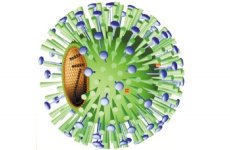
Influenza A virus is a virion that has a spherical shape and a diameter of 80-120 nm, its molecular weight is 250 MD. The virus genome is represented by a single-stranded fragmented (8 fragments) of negative RNA with a total mass of 5 MD. Type of symmetry of nucleocapsid is spiral. The influenza virus has a supercapsid (membrane) containing two glycoproteins - hemagglutinin and neuraminidase, which protrude above the membrane in the form of various spines. Hemagglutinin has a trimer structure with a mass of 225 kD; m of each 75 kD monomer. The monomer consists of a smaller subunit with a mass of 25 kD (HA2) and a larger subunit with a mass of 50 kD (HA1).
The main functions of hemagglutinin:
- recognizes the cellular receptor - mukopeptide, which has N-acetylneuram-a new (sialic) acid;
- ensures the fusion of the virion membrane with the membrane of the cell and the membranes of its lysosomes, ie, it is responsible for the penetration of the virion into the cell;
- determines the pandemic nature of the virus (changing hemagglutinin - the cause of pandemics, its variability - influenza epidemics);
- has the greatest protective properties, responsible for the formation of immunity.
In human, human and mammalian influenza A viruses, 13 antigen-differentiating types of hemagglutinin were detected, which were assigned end-to-end numbering (dH1dHlO3).
Neuraminidase (N) is a tetramer with a mass of 200-250 kD, each monomer has a mass of 50-60 kD. Its functions are:
- ensuring the dissemination of virions by cleavage of neuraminic acid from newly synthesized virions and the cell membrane;
- together with haemagglutinin, the determination of the pandemic and epidemic properties of the virus.
Influenza A virus detected 10 different variants of neuraminidase (N1-N10).
The virion nucleocapsid consists of 8 fragments of vRNA and capsid proteins forming a spiral strand. At the 3 'ends of all 8 fragments of vRNA, there are identical sequences of 12 nucleotides. The 5 'ends of each fragment also have the same sequence of 13 nucleotides. The 5 'and 3' ends are partially complementary to one another. This circumstance, obviously, allows to regulate transcription and replication of fragments. Each of the fragments is transcribed and replicated independently. With each of them, four capsid proteins are firmly linked: the nucleoprotein (NP), it fulfills a structural and regulatory role; protein PB1 - transcriptase; PB2 - endonuclease and RA - replicase. Proteins PB1 and PB2 have basic (alkaline) properties, and PA - acidic properties. The proteins PB1, PB2 and PA form a polymer. Nucleocapsid is surrounded by a matrix protein (M1-protein), which plays a leading role in the morphogenesis of the virion and protects virion RNA. Proteins M2 (encodes one of the reading frames of the 7th fragment), NS1 and NS2 (encoded by the eighth fragment of the vRNA that has, like the seventh fragment of the vRNA, two reading frames) are synthesized during the reproduction of the virus, but do not enter into its structure.
The life cycle of the influenza A virus
The influenza virus is absorbed on the cell membrane due to the interaction of its hemagglutinin with the mucopeptide. Then the virus enters the cell using one of two mechanisms:
- fusion of the virion membrane with the cell membrane or
- along the path fringed fovea - bordered vesicle - endosome - lysosome - fusion of the virion membrane with the lysosome membrane - the yield of nucleocapsid into the cytosol of the cell.
The second stage of "stripping" the virion (destruction of the matrix protein) occurs on the way to the nucleus. The peculiarity of the life cycle of the influenza virus lies in the fact that transcription of its vRNA requires seeding. The fact is that the virus can not synthesize the cap itself, or cap, a special site at the 5 'end of the mRNA, consisting of methylated guanine and 10-13 contiguous nucleotides, which is necessary for the recognition of the ribosome mRNA. Therefore, he uses his protein PB2 to bite off the cap from the cellular mRNA, and since the mRNA synthesis in cells occurs only in the nucleus, the viral RNA must necessarily penetrate into the nucleus first. It penetrates into it in the form of a ribonucleoprotein consisting of 8 fragments of RNA bound to proteins NP, PB1, PB2 and PA. Now the life of the cell is completely subject to the interests of the virus, its reproductions.
Feature of transcription
Three types of virus-specific RNAs are synthesized in the nucleus for vRNA: 1) positive complementary RNAs (mRNAs) used as matrices for the synthesis of viral proteins; they contain at the 5 'end a cap cleaved from the 5' end of the cellular mRNA, and at the 3 'end, a poly-A sequence; 2) full-length complementary RNA (cRNA), which serves as a template For the synthesis of virion RNAs (vRNAs); at the 5'-end of the cRNA the cap is absent, there is no poly-A sequence at the 3 'end; 3) negative virion RNA (vRNA), which is a genome for newly synthesized virions.
Immediately, before the synthesis is completed, vRNA and cRNA enter into association with capsid proteins, which enter the nucleus from the cytosol. However, only the ribonucleoproteins associated with vRNA are included in the virions. Ribonucleoproteins containing cRNA not only do not enter into the composition of virions, but do not even leave the nucleus of the cell. Viral mRNAs enter the cytosol, where they are translated. The newly synthesized vRNA molecules, after association with capsid proteins, migrate from the nucleus to the cytosol.
Features of the translation of viral proteins
Proteins NP, PB1, PB2, RA and M are synthesized on free polyribosomes. Proteins NP, PB1, PB2 and RA after synthesis from the cytosol return to the nucleus, where they bind to newly synthesized vRNA, and then return to the cytosol as nucleocapsid. Matrix protein after synthesis moves to the inner surface of the cell membrane, displacing from it in this area cellular proteins. Proteins H and N are synthesized on ribosomes bound to membranes of the endoplasmic reticulum, transported along them, undergoing glycosylation, and installed on the outer surface of the cell membrane, forming spines just opposite the protein M located on its inner surface. The protein H is processed during the processing by cutting into HA1 and HA2.
The final stage of the morphogenesis of the virion is controlled by M-protein. Nucleocapsid interacts with it; he, passing through the membrane of the cell, is covered first with M-protein, and then with a cellular lipid layer and supercapsed glycoproteins H and N. The life cycle of the virus takes 6-8 hours and ends with the budding of newly synthesized virions that are capable of attacking other cells of the tissue.
Stability of the virus in the external environment is low. It is easily destroyed by heating (at 56 ° C for 5-10 minutes), under the influence of sunlight and UV light and is easily neutralized by disinfectants.
Pathogenesis and symptoms of influenza A
The incubation period for influenza is short - 1-2 days. The virus multiplies in the epithelial cells of the mucous membrane of the respiratory tract with the predominant localization in the trachea, which clinically manifests itself as a dry, painful cough with pain along the trachea. The degradation products of the affected cells enter the bloodstream, cause severe intoxication and increase in body temperature to 38-39 ° C. Increase in vascular permeability, caused by damage to endothelial cells, can cause pathological changes in various organs: spot hemorrhages in the trachea, bronchi, and sometimes brain edema with a fatal outcome. The influenza virus has a depressing effect on blood and immune system. All this can lead to secondary viral and bacterial infections, which complicate the course of the disease.
Postinfectious immunity
Previous beliefs that after the influenza virus remains weak and short-term immunity are disproved after the return of the H1N1 virus in 1977. This virus caused the disease mainly in people under the age of 20, that is, those who had not been sick before, up to 1957. Consequently, postinfectious immunity is quite intense and prolonged, but has a pronounced type-specific character.
The main role in the formation of acquired immunity belongs to virus-neutralizing antibodies that block hemagglutinin and neuraminidase, as well as IgA secretory immunoglobulins.
Epidemiology of influenza A
The source of infection is a person, a sick or a carrier, rarely animals (domestic and wild birds, pigs). Infection from people occurs by airborne droplets, the incubation period is very short (1-2 days), so the epidemic spreads very quickly and can develop into a pandemic in the absence of collective immunity. Immunity is the main regulator of influenza epidemics. As the collective immunity builds up, the epidemic is declining. At the same time, due to the formation of immunity, strains of the virus with a modified antigenic structure, primarily hemagglutinin and neuraminidase, are selected; these viruses continue to cause outbreaks until antibodies appear to them. Such antigenic drift and maintains the continuity of the epidemic. However, in the influenza A virus, another form of variability has been discovered, called the shift, or shear. It is associated with a complete change of one type of hemagglutinin (less often - and neuraminidase) to another.
All influenza pandemics were caused by influenza A viruses that underwent schiltosis. The pandemic of 1918 was caused by a virus with the phenotype H1N1 (about 20 million people died), the pandemic of 1957 - the h3N2 virus (over half the world's population had been ill), 1968 - the H3N2 virus.
To explain the reasons for the sharp change in the types of influenza A viruses, two main hypotheses have been proposed. According to the hypothesis of A. A. Smorodintsev, the virus that has exhausted its epidemic possibilities does not disappear, but continues to circulate in the team without noticeable outbreaks or persistently persist in the human body for a long time. In 10-20 years, when there will be a new generation of people who do not have immunity to this virus, it becomes the cause of new epidemics. This hypothesis is supported by the fact that the influenza A virus with the H1N1 phenotype, which disappeared in 1957 when it was replaced by the h3N2 virus, reappeared after a 20-year absence in 1977
According to another hypothesis, developed and supported by many authors, new types of influenza A virus arise from the reassociation of genomes between human and avian influenza viruses, between avian influenza viruses, between avian and mammalian (swine) viruses, facilitated by the segmental structure of the viral genome (8 fragments ).
Thus, the influenza A virus has two ways of changing the genome.
Point mutations causing antigenic drift. First of all, genes of hemagglutinin and neuraminidase, especially in the H3N2 virus, are susceptible to them. Thanks to this, the H3N2 virus caused 8 epidemics during the period from 1982 to 1998 and remains epidemic until now.
Reassociation of genes between human influenza viruses and avian and swine influenza viruses. It is believed that the reassociation of the genomes of influenza A viruses with the genomes of the avian and swine influenza virus is the main reason for the emergence of pandemic variants of this virus. Antigenic drift allows the virus to overcome the existing immunity in humans. Antigenic shift creates a new epidemic situation: most people do not have immunity to the new virus, and an influenza pandemic occurs. The possibility of such reassociation of the genomes of influenza A viruses has been proved experimentally.
It is established that epidemics of influenza in humans are caused by type A viruses of only 3 or 4 phenotypes: H1N1 (H0N1); h3N2; H3N2.
However, a chicken (avian) virus is also a significant threat to humans. Outbreaks of chicken flu have been observed repeatedly, in particular the chicken H5N1 virus caused a millionth epizootic among domestic and wild birds with 80-90% mortality. People got infected from chickens; so in 1997 from hens 18 people got infected, a third of them died. A particularly large outbreak was observed in January-March 2004. It affected almost all the countries of Southeast Asia and one of the US states and caused enormous economic damage. 22 chickens were infected and killed. To eliminate this outbreak, the most severe and decisive measures were taken: strict quarantine, elimination of the entire number of birds in all outbreaks, hospitalization and isolation of patients and all people with fever, and persons in contact with patients, banning the import of chicken meat from these above the countries, strict medical and veterinary supervision of all passengers and vehicles arriving from these countries. The wide spread of influenza among people did not occur because there was no reassociation of the genome of the chicken flu virus with the genome of the human influenza virus. However, the danger of such a reassociation remains real. This can lead to the emergence of a new dangerous pandemic human influenza virus.
In the name of the detected strains of influenza viruses, the serotype of the virus (A, B, C), the host species (if it is not a human), the place of isolation, the strain number, the year of its isolation (last 2 digits) and the phenotype (in parentheses). For example: "A / Singapore / 1/57 (h3N2), A / Duck / USSR / 695/76 (H3N2)".
Laboratory diagnosis of influenza A
The material used for the study is a detachable nasopharynx, which is obtained either by flushing, or using cotton-tampons, and blood. Methods of diagnostics apply the following:
- Virological - infection of chick embryos, cultures of kidney cells of green monkeys (Vero) and dogs (MDSK). Cell cultures are particularly effective for the isolation of A (H3N2) and B viruses.
- Serological - the detection of specific antibodies and the increase of their titre (in paired sera) with the help of RTGA, RSK, immunoassay method.
- As an accelerated diagnosis, the immunofluorescence method is used, which allows to quickly detect the viral antigen in smears-prints from the nasal mucosa or in washings from the nasopharynx of patients.
- To detect and identify the virus (viral antigens) suggested methods of RNA probe and PCR.
Treatment of influenza A
Treatment of influenza A, which should be started as soon as possible, as well as the prevention of influenza and other viral ARI is based on the use of dibazol, interferon and its inducers amixin and arbidol according to special schemes, and for treatment and prevention of influenza in children older than 1 year - algirem (remantadine ) by special schemes.
Specific prevention of influenza A
Every year in the world, hundreds of millions of people suffer from the flu, which causes enormous damage to the health of the population and the economy of each country. The only reliable means of combating it is the creation of collective immunity. For this purpose, the following types of vaccines are proposed and used:
- live from an attenuated virus;
- killed whole-virion;
- Subvirion vaccine (from split virions);
- subunit-vaccine, containing only hemagglutinin and neuraminidase.
In our country, a trivalent polymer-subunit vaccine ("influenza") is created and applied in which a sterile conjugate of the surface proteins of viruses A and B is linked to a polyoxidonium copolymer (immunostimulant).
Children from 6 months. Up to 12 years, according to WHO recommendations, should be vaccinated only subunit vaccine as the least reactogenic and toxic.
The main problem in increasing the effectiveness of influenza vaccines is to ensure their specificity against the actual virus, that is, the version of the virus that caused the epidemic. In other words, the vaccine must contain specific antigens of the actual virus. The main way to improve the quality of the vaccine is to use the most conserved and common for all antigenic variants of the virus A epitopes that have the maximum immunogenicity.


 [
[