Human arterial pulse
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

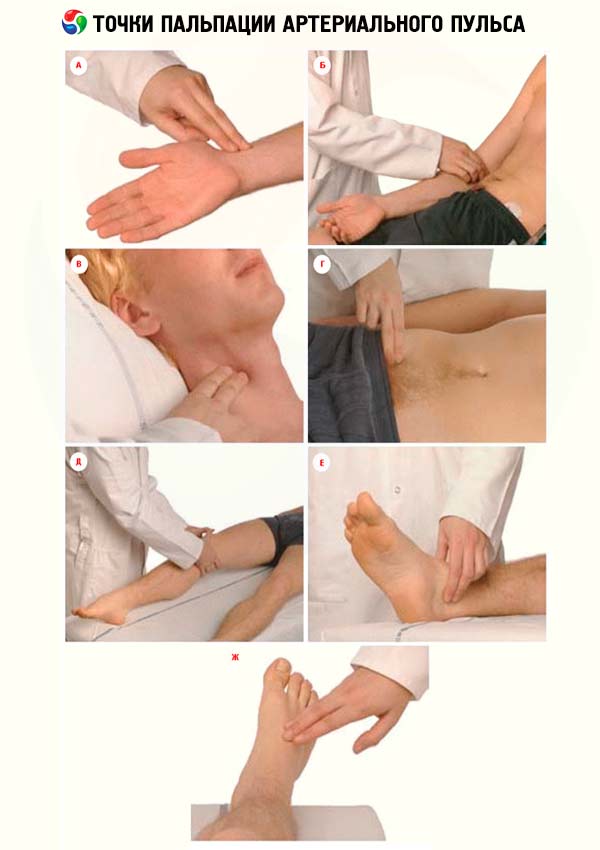
Examination of peripheral arteries usually begins with examination, during which a visible ripple can be detected, for example, carotid arteries on the neck. However, the palpation of the peripheral arterial pulse is the most important. Pulse is determined on the arteries of the carotid, humeral, radial, femoral, popliteal and arteries of the feet. It is generally accepted to evaluate the peripheral arterial pulse and its characteristics on the radial arteries.
Measurement of the arterial pulse
Pulse (pulsus) is a rhythmic oscillation of the artery wall, caused by a change in its blood filling as a result of cardiac contractions. The main clinical method for assessing the condition of the arteries and their pulsations is sensation. Investigation of the pulse is performed in the region of the radial artery in the distal part of it. This place is most convenient for assessing the pulse, because the artery lies right under the skin on the dense bone, although anomalies of its location are possible, but they are comparatively rare. When the pulse is felt, the muscles of the hands should not be strained. First, the pulsation of the radial arteries is simultaneously studied on both hands, if there is no asymmetry, the determination of the pulse is carried out on one arm. With the fingers of the right hand the doctor covers the forearm of the subject near the wrist joint in such a way that the thumb is located on the back of the forearm, and two or three others - on the front surface of the radial artery. Two or three fingers gently probing the area of the artery, squeezing it with varying strength, until the complete cessation of peripheral blood flow. Usually, the radial artery is probed as an elastic band. At an atherosclerotic lesion, the walls of the artery can be compacted, it becomes tortuous. The pulse study is performed in order to evaluate its main properties: frequency, rhythm, voltage, filling, magnitude, pulse wave form.
The pulse is normal
Normally, pulse oscillations are symmetrical on both corresponding arteries. Different characteristics of the pulse on the right and left radial arteries underlie a different pulse (p. Difference). This difference relates to the filling and tension of the pulse, as well as the time of its appearance. If, on the one hand, the pulse appears to be of lesser filling and tension, one should think about narrowing the artery along the path of the pulse wave. Significant impairment of the pulse on one side may be associated with a dissecting aortic aneurysm, peripheral embolism or vasculitis, including aortic lesions (most often aortic ) at different levels. In the latter case, the gradual destruction of the mouth of one of the major arteries leads to the disappearance of pulsations on the radial artery ( Takayasu's syndrome ).
In the period of lowering the pulse wave, a small new upswing can be felt. This double pulse is called dicrotic. Dicrotic recovery is inherent in the normal pulse, which is recorded on a sphygmogram. When you feel the pulse of dicrotia is rarely determined, the dicrotic wave is explained by the fact that at the beginning of the diastole some of the aortic blood makes a slight backward movement and, as it were, hits the closed valves. This blow creates a new peripheral wave, following the main one.

With the right rhythm, but significant fluctuations in the magnitude of cardiac output, the so-called alternating pulse (p. Alternans) is established, in which the filling of individual pulse waves fluctuates.
Thus, various changes in the properties of the pulse are noted. Among them, the most important, in addition to frequency and rhythm, are the filling and tension of the pulse. In typical cases, a healthy person is recorded a rhythmic rhythmic pulse of moderate (or satisfactory) filling and relaxed.
Evaluation of the properties and basic characteristics of the pulse
The pulse rate is determined by counting the pulse beat for 15-30 seconds, and multiplying the figure by 4-2. If the rhythm is wrong, the pulse should be considered for the entire minute. The normal pulse rate in men is 60-70 beats per minute, in women up to 80 beats per minute, in children and the elderly, the pulse is more frequent. When assessing the pulse rate, it should be borne in mind that its frequency increases with mental agitation, in some individuals - in communication with the doctor, with physical exertion, after eating. With a deep inspiration, the pulse becomes more frequent, with exhalation becomes less frequent. The pulse rate increases in many pathological conditions.
The rhythm of the pulse may be correct (p. Regularis) and incorrect (p. Irregularis). Usually, pulse waves follow through intervals of time that are close in duration. Thus pulse waves in norm are identical or almost identical is a uniform pulse (p. Aequalis). In pathological conditions, pulse waves can have different values - an unequal pulse (p. Inaequalis), which depends on the difference in the value of diastolic filling and systolic ejection of the left ventricle.
Systolic ejection with individual cardiac contractions can be so different that the pulse wave can not reach the radial artery when cutting with a small ejection, and the corresponding pulse fluctuations are not perceived palpably. Therefore, if we simultaneously determine the number of cardiac contractions in auscultation of the heart and in the palpation of the pulse on the radial artery, a difference will appear, i.e., a pulse deficit, for example, the number of heartbeats at auscultation of 90 per minute, and the pulse on the radial artery 72 per minute, i.e. A pulse deficit of 18. Such a pulse with a deficit (p., deficiens) occurs with atrial fibrillation with tachycardia. In this case, there are large differences in the duration of diastolic pauses and, consequently, in the magnitude of filling of the left ventricle. This leads to a significant difference in the magnitude of cardiac output during individual systoles. Heart rhythm disturbances can best be characterized and evaluated in electrocardiography.
The pulse voltage is characterized by the pressure that must be exerted on the vessel to completely interrupt the pulse wave at the periphery. The pulse voltage depends on the arterial pressure inside the artery, which can be roughly estimated by the pulse voltage. Distinguish between the pulse is intense, or hard (p. Durus), and the pulse is mild (p.mollis), or relaxed.
Filling of the pulse corresponds to fluctuations in the volume of the artery in the process of cardiac contractions. It depends on the magnitude of systolic ejection, the total amount of blood and its distribution. Filling of the pulse is assessed by comparing the volume of the artery with its complete compression and with the restoration of blood flow in it. The filling is distinguished by the pulse full (p. Plenus), or satisfactory filling, and pulse empty pp. Vacuus). The most striking example of reducing the filling of the pulse is the pulse in shock, when the amount of circulating blood decreases and simultaneously systolic ejection.
The pulse value is determined on the basis of a general evaluation of the voltage and filling of the pulse, their oscillations at each pulse stroke. The magnitude of the pulse is greater, the larger the amplitude of the arterial pressure. In magnitude, the pulse is large (p. Magnus) and the pulse is small (p. Parvus).
The shape of the pulse is characterized by the rapid rise and fall of pressure inside the artery. Lifting can occur more quickly, depending on the rate at which the left ventricle expels blood to the arterial system. Pulse, characterized by a rapid rise in the pulse wave and rapid fall, is called fast (p. Celer). Such a pulse is observed when the aortic valve is inadequate, to a lesser extent with significant nervous excitation. In this case, the pulse is not only fast, but also high (p. Celer et altus). The opposite form of the pulse is p. Tardus et parvus is characterized by a slow rise in the pulse wave and its gradual decrease. Such a pulse occurs in the stenosis of the aortic orifice.
Auscultation of arteries
Auscultation of the arteries is performed without significant pressure, as with high pressure artificially induced stenotic noise. The following main places of listening are noted: the carotid artery - at the inner edge of the sternocleidomastoid muscle at the level of the upper edge of the thyroid cartilage; subclavian - under the clavicle; femoral - under the ligamentous ligament; renal - in the podopupochnoy area on the left and right. Under normal conditions, tones are heard over the carotid and subclavian arteries: I tone depends on the pulse wave, the II tone is associated with the slamming of the aortic valves and the pulmonary artery. Noises in the arteries are heard when they expand or narrow, as well as when carrying out noises in the heart.
Of particular importance is the auscultation of the vessels in the ulnar fossa when determining blood pressure.


 [
[