Chronic Synovitis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
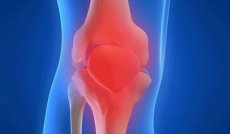
Chronic synovitis is one of the forms of the disease, which is characterized by an inflammatory process in the synovial membrane of the joints. Consider the main causes of the disease, symptoms, diagnostic methods, as well as methods of treatment, prevention and prognosis for recovery.
Chronic synovitis is diagnosed very rarely. Because of inflammation in the synovial membrane of the joint, there is an accumulation of effusion. Most often, this pathology occurs in the knee, ankle, wrist and carpal joints. The disease develops in one joint, but if it develops into polyarthritis, both joints are affected.
The chronic form entails pathological changes in the capsule of the joint and the composition of the blood. At an early stage, diagnosing the disease is problematic. To confirm chronic inflammation, the patient is taken for a punctate examination, biochemical and a number of other studies are performed. If you do not start therapy on time, it increases the risk of sprains, dislocation, or subluxation of the joint. In addition, the ailment causes very unpleasant sensations when trying to bend an arm or leg in a joint that is inflamed, and there is also an external deformation.
Causes of chronic synovitis
The causes of chronic synovitis are diverse and they fall into such groups:
- Aseptic synovitis includes traumatic, neurological and endocrine-related inflammatory disorders.
- Infectious inflammation of joints occurs due to the impact of pathogenic microorganisms (staphylococci, pneumococci, streptococci), which come from the environment (through wounds, lymphogenous or hematogenous from infectious foci of the body).
- Allergic synovitis - occurs due to the action of allergens (infectious and non-infectious nature). The effect is directed to the synovial tissue sensitive to irritants.
Consider the common forms of synovitis and the causes of their occurrence:
- Traumatic
Response to intraarticular damage. As a result of trauma in the synovial membrane, effusion occurs. The disease can appear without apparent cause, as a result of irritation of the synovial membrane, due to the torn meniscus, instability of the joint and other causes.
- Acute traumatic
With this form of pathology, there are changes in the shape of the joint within a few hours or days after the injury. There is a fever, limited movement, tenderness in palpation. The patient suffers from general weakness and ailments. An untreated form of acute inflammation recurs, causing serious complications.
- Purulent
It causes a severe general condition: severe pain, high fever. The skin around the joint is smoothed, there is considerable hyperemia and soreness, movements are difficult. With this form, regional lymphadenitis can develop. With a purulent synovitis, the inflammatory process extends to the fibrous membrane of the joint, provoking the development of purulent arthritis and damage to surrounding tissues. If the cartilage, the ligamentous apparatus of the joint or the bones are involved in the pathological process, this leads to panartriitis.
- Chronic
This form is rare and is characterized by mild symptomatology. Patients complain of restriction of movements in the affected joint, soreness, aching pain, rapid fatigue and fatigue when walking. In the joint cavity, the effusion accumulates, which leads to hydratrosis (dropsy of the joint), with prolonged development, the ligament and ligament of the ligaments develop. Because of this, dislocation and subluxation may occur. Chronic synovitis is divided into serous-fibrinoid, vizle-hemorrhagic and vylezny.
- Chronic villous synovitis
Characterized by sclerotized and hypertrophied villi, which are ligated and form rice bodies and chondromic bodies.
Chronic forms of synovitis, regardless of the cause of their occurrence, are characterized by an increase in pathological changes, a violation of lymph and blood circulation in the capsule of the joint and its fibrous degeneration.
Symptoms of chronic synovitis
Symptoms of chronic synovitis are very similar to those of arthrosis. The disease causes visual changes in the shape of the joint, difficulty in moving and painful sensations. At the initial stage, the pathology causes swelling, which does not resolve due to the constant irritation of the synovial capsule. Because of the inability of the joint elements to perform their functions, they begin to deteriorate. The patient appears a vascular network on the surface of the skin and constant pain.
The acute form of synovitis is characterized by constantly increasing symptoms. The first sign of inflammation is an increase in the affected area in volumes and the formation of puffiness. The fluid within the joint deforms its contours, which significantly complicates the movement. Another pronounced symptom of the disease is inflammation of the internal membranes and pain syndrome. Pain of medium intensity, but not sharp.
If the disease takes a purulent form, then the symptomatology is clearly pronounced. The patient suffers from severe weakness, chills and ailments. In the area of the affected joint, redness of the skin is observed, when pain is experienced, sharp pain occurs.
Chronic synovitis of the knee joint
Chronic synovitis of the knee joint is a disease, inflammatory in nature, affecting the synovial cavity of the knee. By the time of the course of pathology, two forms are distinguished: acute and chronic, each of them has a pronounced symptomatology.
With chronic synovitis, painful sensations occur only during a period of exacerbation of the disease, and pathogenic exudate accumulates gradually. If the disease has a secondary nature, it is a reactive synovitis of the knee joint. This form is considered the most dangerous, because immediate treatment is required, but additional medication can significantly aggravate the patient's condition. Usually, it occurs against the background of allergic reactions or diseases, such as gonarthrosis.
- Serous and serous-fibrinous - arises from the long and intense action of the stimulus in the joint. Exudate has a yellow tinge with characteristic fibrin flakes.
- Purulent - is formed due to the action of various microorganisms that penetrate into the joint cavity. The danger of a purulent synovitis is that the effusion can pass into other tissues and organs through the blood. It is because of this that patients are often diagnosed with delusions, high fever and general ailments.
- Hemorrhagic - another form of chronic synovitis, which refers to benign neoplasms of connective tissue synovial bags, tendons and joints. From this pathology, most often young women suffer.
Where does it hurt?
Diagnosis of chronic synovitis
Diagnosis of chronic synovitis depends on the form and stage of the disease, the age of the patient, the presence of concomitant diseases and other characteristics of the body. If suspected of a synovitis, the following studies should be performed: cytology, arthroscopy, biopsy, synovia research, arthopneumography and others. To confirm inflammation, always use a diagnostic puncture. The obtained materials are examined under a microscope and serological reactions are carried out. This is necessary to determine specific antibodies to a particular pathogen.
In addition to laboratory studies, special attention is paid to the collection of anamnesis. The doctor asks the patient about the onset of the disease, symptoms and other features of the pathology. If the chronic synovitis has arisen against a background of secondary inflammation, then the diagnosis is aimed at identifying the underlying joint disease.
If the diagnosis of chronic synovitis has been confirmed, then first of all it is necessary to ensure complete rest and immobility of the joint. This will prevent further tissue trauma. In addition, you can impose a cold to eliminate puffiness or a tight bandage. Depending on the severity of the ailment, the doctor makes the treatment. All patients are waiting for drug therapy, wearing a knee or bandage, and in particularly difficult cases, surgery.
What do need to examine?
How to examine?
What tests are needed?
Who to contact?
Treatment of chronic synovitis
Treatment of chronic synovitis is a complex of measures aimed at restoring the joint. If the disease has a traumatic nature, first of all it is necessary to eliminate the broken anatomical connections and correct the metabolic shifts in the joint. Depending on the severity of the lesion and the nature of intraarticular changes, treatment can be conservative and surgical. If there are all indications for surgery, then this is considered as the initial stage of treatment, followed by a long course of drug therapy and restoration of metabolic disorders of the joint.
- Of the primary measures for synovitis, the patient is given an early joint puncture with a synovium fence for examination. After that, a tire or bandage is applied to the joint in order to immobilize it for 5-7 days and regularly apply cold to relieve swelling. But prolonged immobilization is undesirable, since it can lead to complications such as stiff joint stiffness.
- With frequently relapsing inflammation, patients are prescribed medications to neutralize the factors that cause synovitis. Most often appointed: Heparin, Indomethacin, Brufen, Glucocorticoids and others. On 3-4 days of taking medications, the patient is prescribed physical methods of treatment: magnetotherapy, electrophoresis, UHF and others.
- With prolonged forms of chronic synovitis for which conservative treatment has proved ineffective, surgical intervention is indicated. Since, most likely, there are irreversible changes in the synovial membrane of the joint: the formation of hypertrophic villi, sclerosis or the formation of petrification.
Surgical treatment of synovitis implies partial, subtotal or total synovectomy. The operation depends on the severity and spread of the inflammatory process. The operation is necessary for irreversible processes in the joints, for example, with the accumulation of crystals of calcium salts. During the operation, a cut of the joint bag is made and it is cleaned of various foreign bodies: deformed menisci, cartilage fragments or salts. After the operation, a plaster is applied to the limb for a couple of days, in order to immobilize it. The patient is prescribed antibiotics and anti-inflammatory drugs. But surgical treatment is used only in the case when all possible methods of conservative therapy have proved ineffective.
Prophylaxis of chronic synovitis
Prevention of chronic synovitis is carried out both after medication, and after surgical treatment. This allows you to prevent relapses of the disease and reduce the negative impact on the body. So, after the surgical intervention the patient is waiting for a long period of rehabilitation. If the patient had a chronic synovitis of the knee joint, then to restore the normal operation of the limb appoint a series of non-complex exercises, which at first performed under the supervision of a doctor.
- Walking - for quick recovery it is recommended to walk at least 3-5 km in average tempo daily. This will speed up the process of joint repair and improve overall health.
- Bicycle - to perform the exercise you need to lie on your back, raise your legs up and do rotational movements (like when riding a bike).
- Squats - this exercise perfectly strengthens the ligaments and muscles could, especially the knee joints.
- Running - small jogging is recommended for patients who have successfully completed the above rehabilitation exercises. Running is best in the morning, to maintain the normal operation of the joints, it is sufficient to run 1-2 km at an average pace every day.
Any restorative exercises can be performed only after the permission of the attending physician. Such caution is fully justified, so the decision on the need for preventive and restorative physical education is taken only by a doctor.
Prevention should include measures to eliminate and prevent inflammatory processes in the joints. To reduce the risk of developing synovitis, it is necessary to treat infectious diseases in a timely manner, to lead a healthy and physically active lifestyle. Avoid joint damage, as this is the best prevention of synovitis. If after a trauma there was a pain or a small puffiness, it is necessary to consult a doctor. Since without proper medical care, the trauma can take the form of a chronic synovitis.
Prognosis of chronic synovitis
The prognosis of chronic synovitis completely depends on the state of the organism and the effectiveness of the treatment. Often against a background of full recovery, stiffness of the joint arises. With the treatment of acute purulent synovitis, a high risk of developing sepsis, so the prognosis depends on the treatment chosen. Without timely access to medical care, the disease takes on a chronic form and causes a number of serious complications. Synovitis can cause purulent arthritis, periarthritis and phlegmon soft tissues or pan-arthritis.
But with early diagnosis and successful treatment, chronic synovitis has a positive prognosis. Observing all the recommendations of doctors, and performing preventive measures, the patient has every chance of a full recovery of an earlier damaged joint.


 [
[