Restenosis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
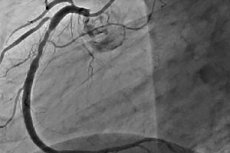
Restenosis is the development of a repeated narrowing of 50% or more at the site of percutaneous coronary intervention. Restenosis is usually accompanied by a relapse of angina, which often requires repeated interventions. As the PCI evolved, the incidence of restenosis decreased, in addition, its character changed.
Restenosis after transluminal balloon coronary angioplasty (TBA)
After carrying out TBA, the incidence of restenosis in the first 6 months. Is 30-40%. The main mechanism of its development is a local negative remodeling of the vessel, which, in essence, is an elastic collapse of the artery lumen enlarged by the balloon during the procedure. A relative role is also played by local thrombosis and neointimal growth. Clinical (type 2 diabetes, acute coronary syndrome, restenosis in the anamnesis), angiographic (PNA lesion, small vessel diameter, chronic total occlusion (HTO), long lesion, degenerated venous shunts) and procedural (large residual stenosis, a small increase in the diameter of the vessel as a result of inflation of the balloon) risk factors for restenosis after TBA. In the case of restenosis, as a rule, repeated intervention is performed. The success of repeated TBA in the place of restenosis is comparable with the first procedure. However, with every subsequent TBCA for restenosis, the risk of recurrence of restenosis increases significantly. After the third attempt, it reaches 50 -53%. In addition, with each conducting of repeated TBA, developing restenosis is more pronounced than the first. The risk of restenosis after the second TBCA for restenosis is the early appearance of the first restenosis (60-90 days after the procedure), PNA lesions, multivessel lesions, the presence of type 2 diabetes, arterial hypertension, unstable angina, and multiple inflations of the balloon at the first procedure. Given the high incidence of restenosis and the mechanism of its development, coronary stents were introduced into clinical practice, which theoretically had to eliminate the negative remodeling of the vessel after TBA.
The first studies that showed the effectiveness of the use of stents were published in 1993, the study of STRESS and BENESTENT. BENESTENT included 516 patients with newly diagnosed stenosis in coronary arteries larger than 3 mm in diameter, which were randomized into two groups: conventional TBA (n = 257) and TBCA with stent placement (n = 259). After 3 years, the rate of restenosis with angiography in the conventional TBCA group was 32%, and in the stent group - 22%. The relative decrease in the incidence of restenosis was 31% (p <0.01). The need for repeated myocardial revascularization was also lower in the stenting group (10 vs 20.6% in the usual TBCA group, p <0.01), which was associated with a lower incidence of angina recurrence in the stent group.
According to the STRESS study (n = 407), in the stenting group (n ~ 205) the restenor frequency was also lower than in the usual TBCA group (n = 202), 31.6 vs 42.1% (p <0.01 ). The advantage of using stents over conventional angioplasty in the event of restenosis development at the site of TBA was demonstrated in the REST study, in which 383 patients with restenosis were randomized to stenting groups or repeated percutaneous transluminal coronary angioplasty. Angiographically revealed repeat restenosis was lower by 18% in the stenting group (18 vs 5.32%, p <0.03). Repeated myocardial revascularization, which is an indicator of clinically significant restenosis, was also required significantly less in the group of patients subjected to stenting (10 vs 27%, p <0.001). Thus, the best results with the use of stenting were proved not only on the native arteries, but also in the case of intervention for restenosis that developed after TBA.
Restenosis after implantation of uncovered stent (NPC)
Although uncoated coronary stents reduced the incidence of restenosis compared with TBA by 30-40%, in 17-32% of patients even after stenting, restenosis is already developing within the stent, which requires repeated revascularization. The mechanism of development of intrinsic stenosis (HRV) differs from that in TBA. After stenting, the main contribution to restenosis is caused by the formation of neointima, and not by negative remodeling, as in TBA, which is practically absent at the stent implantation site. Neointima is formed by the migration and proliferation of smooth muscle cells that produce an extracellular matrix, which together with the cells constitutes neointima. In addition, the persistence of a thrombus in the site of stenting is also important in diabetic patients.
The main classification of intraventricular stenosis is the classification proposed by Mehran, which includes four types depending on the extent and severity of the lesion: I type of VRS is local (<10 mm in length), type II is diffuse (> 10 mm in length), type III - proliferative (> 10 mm and extending beyond the stent) and IV type - HRV leading to occlusion. The first type is subdivided into subtypes depending on the location in the stent: 1a - on the bend or between the stents, 1b - edge, 1c - inside the stent, 1d - multifocal.
The risk factors for the development of HRV are the interventions of venous shunts, chronic occlusions, aperture lesions, small vessel diameter, the presence of residual stenosis, stenting for BPV, a small post-procedural vessel diameter, a PNA lesion, a large stent length, the presence of DM, the implantation of several stents in one lesion . There are indications of the influence of genetic factors, in particular polymorphism of the glycoprotein IIIa gene and the mutation of the gene for methylenetetrahydrofolate reductase, a gene that codes for interleukin-1. In the case of development of marginal stent restenosis, the main risk factor is a pronounced atherosclerotic lesion in the stented segment.
Predominantly, restenosis occurs within the first 6-8 months. After percutaneous coronary intervention. In most patients around the same time, there are clinical symptoms. Usually, HRV manifests itself as a relapse of angina pectoris. Less frequent (11-41% of cases) there is unstable angina. In 1-6% of patients, AMI develops. Thus, the most common cause of angina in 1-6 months. After stenting is the development of HRV, which, as a rule, requires a repeated revascularization. There are several methods of treatment of HRV. Conventional TBA can be performed, which leads to further opening of the stent (56% contribution to the final increase in vessel diameter), and also pushes the neointima through the stent cells (44% contribution to the final diameter increase). However, for the most part, residual restenosis is observed at the site of intervention (an average of 18%). In addition, after TBA, repeated revascularization is required in 11% of cases, more often in patients with multivessel lesions, low LVEF, in the case of interventions on venous shunts or the early occurrence of the first HRV. The risk of developing recurrent HRV after TBCA also depends on the type of lesion and ranges from 10% in the case of local restenosis to 80% with an invasive occlusion. Implantation of the NPC in place of HRV does not reduce the risk of its recurrence in comparison with only TBA.
The second method of treatment of HRV is brachytherapy, which consists in introducing into the lumen of the coronary artery a radioactive source that prevents the proliferation of smooth muscle cells and accordingly reduces the risk of restenosis. Nevertheless, the high cost of equipment, the technical complexity of the procedure and the increased frequency of late stent thrombosis (TC) almost completely excluded brachytherapy from clinical use.
The revolutionary moment of treatment of VRS was the introduction of drug-eluting stents. Compared with the NPS in the case of native arteries, they reduce the risk of developing HRV by 70-80%. The first data on the effectiveness of SLP in patients with already developed HRV were obtained in the register of patients TAXUS III, in which LNG1 in such patients after 6 months. The recurrence rate of HRV was only 16%, which is lower than in the previously mentioned studies with TBA. In the TRUE register, which included patients after implantation of ATP for restenosis of the NPC, after 9 months. Repeated revascularization was required by less than 5% of patients, mainly with diabetes and ACS. In the study, TROPICAL compared the incidence of restenosis in patients after implantation of SLP at the site of restenosis with data from the GAMMA I and GAMMA II studies, in which brachytherapy was used as a method of treatment. After 6 months. The incidence of restenosis was significantly lower in the ATP group (9.7 vs 40.3%, p <0.0001). It is important to note that the incidence of stent thrombosis, myocardial infarction, was also lower in the ATP group (TS 0.6 vs 3.9%, p = 0.08, MI 1.8 vs 9.4%, p = 0.004). The benefit of ATP before brachytherapy was confirmed in a randomized SISR study in which 384 patients with advanced HRV in HSP were randomized to brachytherapy or implantation of ATP. After 9 months. The need for re-revascularization was higher after brachytherapy (19.2%) than in the ATP implantation group (8.5%), which reflected a more frequent relapse of restenosis. After 3 years, the advantage of ATP in terms of reducing the need for repeated revascularization for the relapse of stent restenosis persisted (19 vs 28.4%). There was no significant difference in the incidence of thrombosis between the groups.
The main factors of the recurrence of HRV in patients with NPCs in the case of implantation of ATP are a small vessel diameter (<2.5 mm), a diffuse type of restenosis, and the presence of chronic renal failure requiring hemodialysis. In a randomized trial of TAXUS V ISR, SPP also demonstrated high efficacy in the treatment of HRV, reducing the rate of restenosis recurrence by 54% compared with brachytherapy.
Randomized studies have also been performed comparing the efficacy of TBA for HRV and SLP implantation. In a randomized study of RIBS-II after 9 months. Repeated restenosis was 72% less common after implantation of SLP than after TBA, which reduced the need for repeated revascularization from 30 to 11%. In the ISAR DESIRE study, the efficacy of TBA in HRV was compared with implantation of SPP or ATP. After 6 months. It was found that both SLPs more effectively prevented restenosis than TBAA (its incidence was 44.6% with TBA, 14.3% in the ATP group, and 21.7% in the NGN group), which reduced the need for repeated revascularization. In direct comparison of PPS and ATP, it turned out that ATPs reduce the need for re-revascularization significantly more effectively than PPS (8 vs 19%). Thus, implantation of SLP reduces the frequency of development of recurrent HRV NPS compared to both TBA and brachytherapy, which reduces the number of repeated PCI and therefore makes their implantation a procedure of choice in such patients.
Restenosis after implantation of a drug-eluting stent (SLP)
Despite a 70-80% reduction in the incidence of intra-stenal stenosis when using SLP in comparison with NPCs, they could not completely rule out the development of this iatrogenic effect of stenting. Its overall frequency remains on average less than 10%. In addition to quantitatively reducing the incidence of restenosis, they also significantly altered the type of restenosis that forms. So, after SLP implantation, restenosis, as a rule, is focal. Clinically, as in the case of NPS, it most often manifests itself as a relapse of stable angina pectoris (77%), less often (8%), it is asymptomatic. In 5% of cases, it manifests unstable angina, and in 10% - the first symptom is non-Q-myocardial infarction. The main factors for the development of restenosis SLP are type 2 diabetes, a small diameter of the vessel, as well as the extent of the lesion. Clear recommendations regarding the management of such patients do not. Alternatives are repeated implantation of SLP (of the same type or another type), conduction of TBA or brachytherapy. The average frequency of development of restenosis during implantation of the second SLP is 24%, while it is the same in the case of implantation of the same type of SLP or another.


 [
[