Classification of breast cancer
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

The variety of morphological features, variants of clinical manifestations and reactions to therapeutic effects gives all grounds to define breast cancer as a non-uniform disease. Therefore for today there is not one classification of a cancer of a mammary gland, and a little. And each of them is based on its principles.
Classification of breast cancer by TNM
Defines the stages of breast cancer classification of TNM Classification of Malignant Tumours, adopted by the WHO for all malignant neoplasms. For oncological mammology, based on the recommendations of leading specialists, it is adapted with the introduction of detail.
The classification of breast cancer by TNM measures the anatomical extent of the tumor based on its size, prevalence of lymph nodes in the armpits, neck and chest, and also notes the presence of metastases. This international classification of breast cancer has been adopted by the International Association for Breast Cancer and the European Society for Medical Oncology (EUSOMA).
According to the TNM classification, breast cancer has the following stages:
- T0 - signs of breast cancer not detected (not proven).
- Tis (tumor in situ) designation refers to carcinomas and is interpreted as follows: abnormal cells are found in situ (there is no invasion), the localization is limited to the ducts (DCIS) or lobules (LCIS) of the mammary gland. Also there is the Tis Paget, that is, the Paget's disease affecting the nipple tissue and the areola of the breast.
- T1 - tumor diameter at the widest point of 20 mm or less:
- T1a - tumor diameter> 1 mm, but <5 mm;
- T1b - tumor diameter greater than 5 mm, but less than 10 mm;
- T1c - tumor diameter> 10 mm, but ≤ 20 mm.
- T2 - tumor diameter> 20 mm, but <50 mm.
- T3 - tumor diameter exceeds 50 mm.
- T4 is a tumor of any size and has spread: to the chest (T4a), to the skin (T4b), to the chest and skin (T4c), inflammatory breast cancer (T4d).
Indicators for lymph nodes:
- NX-lymph nodes can not be evaluated.
- N0 - the cancer was not found in the lymph nodes.
- N0 (+) - small areas of "isolated" tumor cells (less than 0.2 mm) are found in the axillary lymph nodes.
- N1mic - areas of tumor cells in the axillary lymph nodes are more than 0.2 mm, but less than 2 mm (can be seen only under a microscope and are often called micrometastases).
- N1 - the cancer spread to 1-2-3 axillary lymph nodes (or the same number of intrathoracic), a maximum size of 2 mm.
- N2 - the spread of cancer to 4-9 lymph nodes: only on the axillary (N2a), only on the internal thoracic (N2c).
- N3 - the cancer has spread to 10 or more lymph nodes: on the lymph nodes at hand, or under the clavicle, or over the clavicle (N3a); on the internal pectoral or axillary nodes (N3c); supraclavicular lymph nodes (N3c) are affected.
Indicators for distant metastases:
- M0 - there are no metastases;
- M0 (+) - clinical or radiographic signs of distant metastases are absent, but tumor cells are found in the blood or bone marrow, or in other lymph nodes;
- M1 - metastases in other organs are determined.
Histological classification of breast cancer
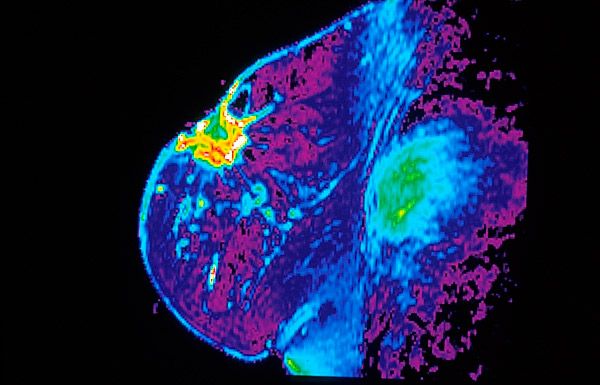
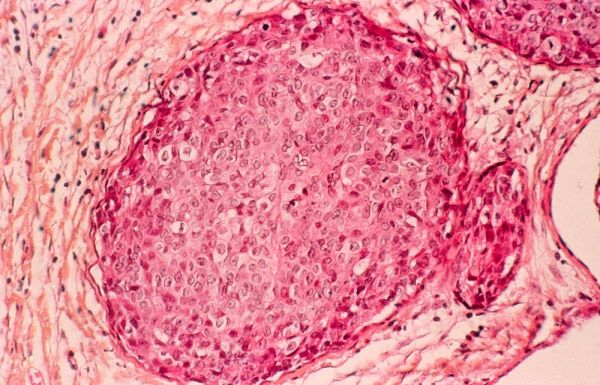
Current histopathological classification of breast cancer is based on the morphological features of neoplasia, which are studied in the course of histological studies of samples of tumor tissue - biopsy specimens.
In the current version, approved by WHO in 2003 and accepted worldwide, this classification includes about two dozen large types of tumors and almost as many less significant (less frequent) subtypes.
The following main histotypes of breast cancer are distinguished:
- non-invasive (non-infiltrating) cancer: intra-proton (protocol) cancer; lobular or lobular cancer (LCIS);
- invasive (infiltrating) cancer : protocol (intraluminal) or lobular cancer.
These types, according to the statistics of the European Society of Medical Oncology (ESMO), account for 80% of clinical cases of malignant tumors of the mammary glands. In other cases, less common types of breast cancer are diagnosed, in particular: medullary (soft tissue cancer); tubular (cancer cells form tubular structures); mucinous or colloidal (with mucus); metaplastic (squamous, glandular-squamous, adenocystic, mycoepidermoid); papillary, microsipillary); cancer of Paget (tumor of the nipple and areola), etc.
Based on the standard protocol of histological studies, the level of differentiation of normal and tumor cells is determined, and thus the histological classification of breast cancer makes it possible to establish the degree of malignancy of the tumor (this is not the same as the stage of cancer). This parameter is very important, as the level of histopathological differentiation of the neoplasia tissue gives an idea of the potential of its invasive growth.
Depending on the number of deviations in the structure of cells, degrees (Grade) are distinguished:
- GX - the level of discrimination of tissues can not be estimated;
- G1 - a tumor highly differentiated (low grade), that is, tumor cells and the organization of the tumor tissue are close to normal;
- G2 - moderately differentiated (middle grade);
- G3 - low-grade (high grade);
- G4 - undifferentiated (high grade).
Degrees G3 and G4 mean a significant predominance of atypical cells; such tumors grow rapidly, and the rate of their spread is higher than for tumors with differentiation at the level of G1 and G2.
The main drawbacks of this classification are seen by specialists in the limited ability to more accurately reflect the heterogeneity of breast cancer, because in one group there were tumors having absolutely different biological and clinical profiles. As a result, the histological classification of breast cancer has minimal prognostic value.
Immunohistochemical classification of breast cancer
Thanks to the use of new molecular tumor markers, the expression of the cellular receptors of the tumor to estrogen (ER) and progesterone (PgR) and the status of HER2 (EGFR transmembrane protein receptor of the epidermal growth factor, stimulating cell growth), a new international classification of breast cancer that has proven prognostic value and allows more precise determination of the methods of therapy.
Assuming the state of the estrogen and progesterone receptors, the activation of which leads to changes in the cells and tumor growth, the immunohistochemical classification of breast cancer distinguishes between hormone-positive tumors (ER +, PgR +) and hormone-negative (ER-, PgR-). Also, the status of EGFR receptors can be positive (HER2 +) or negative (HER2-), which has a profound effect on treatment tactics.
Hormone-positive breast cancer lends itself to hormonal therapy with drugs that lower the level of estrogen or block its receptors. As a rule, such tumors grow more slowly than hormone-negative ones.
Mammology notes that patients with this type of neoplasm (which are more likely to occur after menopause and affect the lining tissues) in the short term have a better prognosis, but cancer with ER + and PgR + can sometimes give relapses after many years.
Hormone-negative tumors are much more often diagnosed in women who have not yet gone through menopause; the data of neoplasia are not treated with hormonal drugs and increase faster than the hormone-positive cancer.
In addition, immunohistochemical classification of breast cancer reveals triple positive cancer (ER +, PgR + and HER2 +), which can be treated with hormonal agents and preparations with monoclonal antibodies designed to suppress the expression of HER2 receptors (Herceptin or Trastuzumab).
A triple negative cancer (ER-, PgR-, HER2-), which is classified as a molecular basal subtype, is characteristic of young women with a mutant BRCA1 gene; the main drug treatment is carried out by cytostatics (chemotherapy).
In oncology, it is decided to decide on the appointment of treatment on the basis of all possible characteristics of the disease, which provides the doctor with each classification of breast cancer.
Who to contact?


 [
[