Labyrinthitis (inflammation of the inner ear)
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The labyrinth (otitis internal, inflammation of the inner ear) is an inflammatory disease of the inner ear that results from the penetration of pathogenic microorganisms or their toxins into it and manifests itself as a combined disturbance of the functions of the peripheral receptors of the vestibular and auditory analyzers.
Epidemiology
According to summary statistical data, by the end of the 50th year of the 20th century, the maze labyrinthites were 1.4-5.4% of the total number of purulent otitis media. Given that the greatest number of cases of labyrinthitis is associated with inflammation of the middle ear, prevention is the timely diagnosis and effective treatment of otitis media, which affects mainly children. Middle otitis in the gums is the result of the transition of the inflammatory process from the nasopharynx and pharynx through the auditory tube into the middle ear cavity. Thus, a thorough sanitation of the nose, nasopharynx and pharynx is a measure of prevention among their otitis and otogenic complications.

Causes of the labyrinthite
Labyrinthitis can be caused by various viruses, bacteria and their toxins, trauma. The source of infection is most often located in the immediate vicinity of the maze of inflammation in the middle ear cavity or skull (acute and chronic otitis media, mastoiditis, cholesteatoma, petrositis). With purulent inflammation of the middle ear, the infection penetrates into the labyrinth.
The dominant role belongs to bacteria - streptococcus, staphylococcus. Mycobacteria of tuberculosis. The causative agent of the meningogenic labyrinthitis is meningococcus, pneumococcus, tuberculosis mycobacterium, pale treponema, influenza and mumps viruses.

Pathogenesis
Various factors are important for the development of the labyrinthitis: general and local reactivity of the organism, the nature and degree of virulence of the pathogen, the features of the inflammation in the middle ear and the cranial cavity, the pathways of infection into the inner ear. There are the following types of penetration of the infection into the inner ear: tympanogenic (from the middle ear cavity through the windows of the labyrinth, fistula), meningogenic (from the subarachnoid space of the brain), hematogenous (by vessels and lymphogenous pathways in patients with common infectious diseases of the viral etiology).
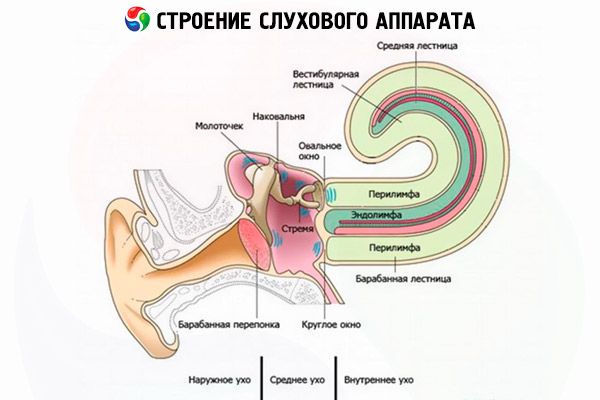
Transition of the inflammatory process from the middle ear is possible on any part of the labyrinth wall, but occurs, as a rule, through the membranous formations of the labyrinth windows and the lateral semicircular canal. In acute purulent inflammation of the middle ear and chronic purulent mesotympanitis, the inflammatory process spreads through the windows without breaking their integrity or by breaking through, which leads to the development of an acute diffuse serous or purulent labyrinthitis. With chronic purulent epitimanitis, the spread of inflammation proceeds by destroying the wall of the bone labyrinth by the pathological process, often in combination with the breakthrough of membranous window formations, the infection can pass through "reformed ways (vessels, seals).
In the pathogenesis of labyrinthitis, which has developed as a result of trauma, the integrity of the bone and membranous labyrinth, the degree of edema, hemorrhage in the peri- and endolymphatic space is important. If, in addition to labyrinthitis, a circulatory disturbance occurs in one of the terminal branches of the internal auditory artery (compression, stasis of the blood), then a necrotic labyrinthitis develops. The reduction of such small arteries, as internal auditory, is promoted by endolymphatic edema, which is especially often manifested in serous inflammation. Limited labyrinthitis is observed only in chronic purulent epitimpanitis with caries and cholesteatoma. With chronic purulent infection, the destruction of the wall of the bone labyrinth occurs under the influence of the inflammatory process or cholesteatoma, which by means of pressure promotes the creation of the fistula of the labyrinth.
Most often, the fistula is localized in the region of the lateral semicircular canal, but it can form in the region of the base of the stapes, promontories, other semicircular canals. During exacerbation of inflammation in the middle ear there is exudate, in connection with which the limited labyrinthite passes into diffuse. With syphilis, any pathway of the transition of a specific inflammatory process to the labyrinth, including hematogenous, is possible.
From the cranial cavity from the side of the meninges, the infection penetrates into the inner ear through the aqueduct of the cochlea and the internal auditory canal.
In the pathogenesis of labyrinthitis, which has developed as a result of trauma, disruption of the integrity of the membranous and bony labyrinth, concussion, hemorrhage in the peri- and endolymphatic space is important.
Morphological changes in the inner ear with serous, purulent and necrotic labyrinthitis are different.
In serous labyrinthitis, endolymphatic edema, swelling, vacuolization, and decay of the neuroepithelium are observed. With a purulent labyrinthite, a polymorphonuclear leukocyte and bacteria accumulate in the periphery of the perilymphatic space against the background of dilated blood vessels. Then these changes occur in the endolymphatic space, the edema progresses, necrosis of membranous, and later also the bone walls of the labyrinth is added. With a favorable outcome, fibrosis and the formation of a new tissue are possible, which leads to the destruction of all receptor, nervous elements. Necrotic labyrinthitis is characterized by an alternation of areas of purulent inflammation and necrosis of soft tissues and a capsule of the labyrinth. The inflammatory process can capture the entire labyrinth, or confine itself to one of its parts. The process ends with labyrinth sclerosis.
With a specific infection, the labyrinthite has some morphological features. So changes in tuberculous labyrinthitis are manifested in two forms: proliferative and exudative-necrotic. The defeat of the inner ear with syphilis manifests itself as meningoneurolabirintitis, while osteitis of the temporal bone is observed with the involvement of the membranous labyrinth. The morphological picture is characterized by edema, growing dystrophy of the membranous labyrinth, areas of proliferation of fibrous tissue, along with bone resorption.
 [5]
[5]
Symptoms of the labyrinthite
In typical cases, the acute labyrinthitis is manifested by a labyrinthine attack with a sudden difference in severe dizziness and a combination with nausea and vomiting, a violation of optical and dynamic balance, noise in the ear and a decrease in hearing. Vertigo is systemic, strongly pronounced; the patient can not lift his head, turn it aside; the slightest movement increases nausea and causes vomiting, profuse sweating, discoloration of the facial skin. With serous labyrinthitis, the symptoms persist for 2-3 weeks, and gradually lose their severity, disappear. With a purulent maze, after the acute inflammation subsides, the disease can take a prolonged course.
Sometimes the labyrinthitis develops as a primary chronic and is characterized by periodic obvious or less pronounced symptoms of labyrinthine disorders, which makes it difficult to timely accurately diagnose. Currently, in such cases, the study of the temporal bone helps with the help of high-resolution neuroimaging methods.
Cochlear symptoms - noise and hearing loss down to deafness - are observed both in diffuse serous and purulent labyrinthitis. Persistent deafness often indicates a purulent inflammation in the labyrinth.
When meningococcal infection, as a rule, two labyrinths are affected, which is accompanied by unexpressed peripheral vestibular disorders; violation of equilibrium prevails. Simultaneous bilateral complete loss of vestibular excitability is often accompanied by a sharp decrease in the auditory function,
The tubercular labyrinthitis is characterized by chronic latent flow. Progressive violation of labyrinth functions.
The clinical picture of syphilitic labyrinthitis is diverse. Typical cases are characterized by fluctuating episodes of hearing loss and dizziness. With acquired syphilis, three forms of labyrinthitis are distinguished:
- apoplectiform - there is a sudden and irreversible combined or isolated loss of labyrinth functions in one or both ears. Often there is a simultaneous lesion of the facial nerve (process in the region of the bridge-cerebellar angle). It occurs in all stages of syphilis, but more often in the second.
- acute form (with syphilis) - unstable noise in the ears and dizziness - sharply intensified toward the end of the 2-3 nd week, rapid onset of severe inhibition of the functions of the labyrinth. It is observed in the second and third stages of syphilis.
- chronic form - noise in the ears, inconspicuous for the patient gradual decrease in hearing and vestibular excitability, which can be diagnosed only with additional examination of the patient. It is observed in the second stage of the disease.
Where does it hurt?
What's bothering you?
Forms
Labyrinthites are distinguished.
- On the etiologic factor - specific and nonspecific.
- According to the pathogenesis - tympanogenic, meningogenic, hematogenous and traumatic.
- Labyrinth thympanogenic is due to the penetration of the pathogen of infection into the inner ear from the middle ear cavity through the windows of the labyrinth.
- Labyrinthitis meningogenic develops with meningitis due to the penetration of pathogens of infection from the sub-pawtine space through the aqueduct of the cochlea or internal auditory canal.
- Labyrinthite hematogenous is due to the penetration of pathogens into the inner ear with blood flow: occurs more often in viral infectious diseases.
- Labyrinthitis is traumatic caused by trauma (for example, with a fracture of the base of the skull, gunshot wound).
- By the nature of the inflammatory process - serous, purulent and necrotic.
- Labyrinthine serous is characterized by an increase in the amount of perilymph, swelling of the labyrinth endosteum, the appearance of fibrin and blood elements in the endo- and perilymph.
- Labyrinthitis purulent is caused by pathogens of purulent infection and is characterized by leukocyte infiltration of peri- and endolymph, the formation of granulations.
- Labyrinthitis necrotic is characterized by the presence of areas of necrosis of soft tissues and bone maze, alternating usually with foci of purulent inflammation.
- According to the clinical course - acute and chronic (obvious and latent).
- Labyrinthitis is an acute serous or purulent labyrinthitis, manifested by sudden development of symptoms of impaired internal ear functions (dizziness with nausea and vomiting, violation of static and dynamic body balance, ear noise, hearing loss); with serous labyrinthitis the symptoms gradually disappear after 2 weeks, with a purulent disease can take a chronic course.
- Labyrinthitis is chronic, characterized by a gradual development of violations of the inner ear (dizziness with nausea and vomiting, noise in the ear, a violation of static and dynamic balance of the body, hearing loss), the presence of a fistulous symptom, spontaneous vestibulo-vegetative, vestibulosensory and vestibulomatic reflexes.
- By prevalence - limited and diffuse (generalized).
- Labyrinthite limited - lesion of a limited area of the wall of the bone labyrinth; It is observed in chronic otitis media and is caused by granulating osteitis or pressure of cholesteatoma.
- Labyrinthite diffuse - purulent or serous labyrinthitis, spread to all parts of the bone and membranous labyrinth.
- Labyrinthitis viral often develops against the background of herpes zoster oticus begins with pain in the ear and behind the ear, vesicular eruptions in the external auditory canal. The combination of auditory and vestibular disorders is often accompanied by paresis of the facial nerve. Viral infection extends to the vestibular nerve, posterior semicircular canal and sacculus.
Diagnostics of the labyrinthite
At the heart of the timely diagnosis of the labyrinthitis is a reliable and carefully collected anamnesis.
The tympanogenic labyrinthitis is most common. For its diagnosis it is necessary to perform otoscopy, vestibulometry and audiometry, radiography or CT of temporal bones. If a patient has acute or chronic otitis media, a fistulous symptom is examined.
The pathognomonic sign of a limited labyrinthitis with a fistula, but against the background of the preserved function of the inner ear neuroepithelium, is a fistulous symptom, that is, the appearance of dizziness and nystagmus towards the diseased ear with air compression in the external auditory canal.
Significant diagnostic signs of labyrinthitis are spontaneous vestibular reactions proceeding along the peripheral type. A decisive diagnostic value is the correct evaluation of spontaneous nystagmus in combination with a gently flowing vestibulospinal reflex. The direction and intensity of the nystagmus varies according to the severity of the inflammatory process, the stage of the disease.
In the initial stages of both serous and purulent labyrinthitis, spontaneous nystagmus is directed toward the affected labyrinth and has I, II, III degrees of severity. This nystagmus is combined with the deviation of the arms and trunk and the side of the slow component, observed for several hours, sometimes days, gradually changing its direction to the opposite (towards the healthy labyrinth). The appearance of spontaneous nystagmus in the opposite direction is the result of the development of compensatory mechanisms in the central sections of the vestibular analyzer aimed at aligning the functional state of the two labyrinths. This kind of nystagmus is observed and is rarely detected, since it remains for a short time.
Often absent in the visual assessment of spontaneous nystagmus is recorded by the method of electrostemagmography. After 2-3 weeks spontaneous nystagmus disappears. Conducting experimental vestibular reactions during this period of labyrinthitis is contraindicated and impractical, as it can cause increased dizziness and does not help the diagnosis. However, in the following, carrying out experimental vestibular samples allows us to reveal the nystagmus assimetry in the labyrinth, the phase of depression, and evaluate the development of central vestibular compensatory responses. Initially, the decrease in vestibular excitability on the side of the affected labyrinth is accompanied by hyperreflexia from the healthy labyrinth, and in the recurrent period of the disease, vestibulometry reveals a symmetrical hyporeflexia, the absence of spontaneous nystagmus. In addition to spontaneous nystagmus, another labyrinth symptomatology is revealed: a gait disturbance and a deviation of the head and trunk to a healthy side. It is important to know that turning the head to the sides of a patient with a labyrinthitis is accompanied by a change in the direction of the spontaneous nystagmus, which leads to a change in the direction of the patient's torso deviation. At a cerebral pathology the patient always deviates towards the center of a lesion.
In the study of hearing in patients with labyrinthitis, hearing loss is of a mixed type, often with a predominance of neurosensory.
With congenital syphilis, the course and symptoms depend on the severity of the infection and the specific changes in the body. The disease begins in childhood and manifests itself as symptoms of impairment of the functions of the inner ear. In late congenital syphilis, an atypical fistula symptom is often detected with an intact tympanic membrane and no fistula in the lateral semicircular canal. In contrast to the typical fistula symptom, nystagmus, when compressed in the external auditory canal, is directed towards the healthy side, and in decompression - toward the irritated ear.
The traumatic labyrinthitis is characterized by the nature and severity of the injury itself.
Screening
Not done.
 [8]
[8]
Indications for consultation of other specialists
Depending on the etiology of the disease in some cases, a consultation of a neurologist, a neurosurgeon, a dermatovenerologist is required.
What do need to examine?
Differential diagnosis
With tympanogenic and traumatic labyrinthitis purulent infection can penetrate into the cavity of the skull, causing intracranial complications - meningitis and abscess. Diagnosis of intracranial complications is difficult. Characteristic deterioration of the general condition, fever, the emergence of headaches, increased dizziness, the emergence of cerebellar symptoms. To recognize complications, CT scan of the brain, consultation of a neurologist, neurologist.
Thus, to recognize the labyrinthite, it is necessary:
- to establish the fact of the disease of the inner ear (anamnesis);
- to verify the infectious nature of the disease;
- specify the ethnological factor;
- To determine the prevalence of the process in the labyrinth.
The diagnosis is not difficult, if there are characteristic vestibular and auditory disorders due to infection. Includes anamnestic data, results of otoscopy, hearing and vestibulometry studies, positive results of the fistula test. At present, radiography of temporal bones, as was the case before, is of great importance, but CT and MRI of the brain and inner ear. High-resolution MRI and CT with visualization of the structures of the inner ear have become the most important diagnostic methods of investigation in the pathology of the inner ear, including labyrinthitis of inflammatory genesis.
Audiometry and vestibulometry help to identify the peripheral nature of auditory and vestibular disorders. It is characteristic that in the pathology of the inner ear of the non-genic origin, deafness is rarely noted (myocardial infarction). Successful diagnosis of labyrinthitis is facilitated by a comprehensive evaluation of the results of all methods of patient research. Differential diagnosis should also be performed with limited otogenic pachymeningitis (arachnoiditis) of the posterior cranial fossa and the cerebellar angle, with acute thrombosis of the auditory artery. Otogenous arachnoiditis is characterized by otoneurological symptoms that reveal the combined damage of the root of VIII, V and VII cranial nerves. Acute thrombosis of the internal auditory artery is characterized by acute symptoms of loss of function of auditory and vestibular receptors on the background of vascular pathology (arterial hypertension, atherosclerosis).
Who to contact?
Treatment of the labyrinthite
The treatment is carried out in the hospital taking into account the etiology and pathogenesis of the disease,
Medical treatment of labyrinthitis
Conservative treatment includes the use of antibiotics, taking into account the sensitivity to the pathogen and their penetration through the hematolabyrinth barrier. Patients with labyrinthitis are prescribed medications that have an anti-inflammatory, hyposensitizing effect, normalizing metabolic processes in the inner ear and brain. During the labyrinth attack, vestibolitics. Drugs that improve blood flow to the inner ear.
Surgical treatment of labyrinthitis
Surgical treatment of the otogenous labyrinthitis consists in the obligatory removal of the purulent focus from the cavities of the middle ear and careful revision of the promontorial wall. Sane surgery on the ear is performed in any form of labyrinthitis. Operative interventions on the labyrinth are shown with purulent labyrinthite, sequestration of the labyrinth. When labyrinthotomy is limited to drainage of a purulent focus in the inner ear by opening it and removing pathological contents. Mastoidectomy in acute uncomplicated labyrinthitis is performed only in cases involving the mastoid process. With labyrinthogenic intracranial complications, a labyrinthectomy is performed: the entire labyrinth is removed, the hard medulla of the posterior cranial fossa are exposed, and a good drainage of the cranial cavity is created.
Prevention
Sanitation of foci of infection in the middle ear cavity.

Forecast
Approximate terms of incapacity for work from 3 weeks to 3 months. The timing is due to the slow recovery of the vestibular function.


