Condylomatosis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
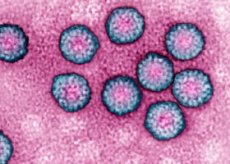
A common viral disease of condylomatosis is provoked by papillomavirus infection. It can be attributed to diseases that are sexually transmitted.
In the last decade, condylomatosis occurs more often: in diagnosis it can be taken for another disease, so a special role is assigned to specialists in differential diagnosis and prevention of this pathology.
Causes of condylomatosis
A large number of different varieties of papillomavirus is known, of which No. 6 and No. 4 are capable of provoking the appearance of condylomatosis.
Papillomavirus can be spread by contact method. The most common infection occurs sexually, including through oral or other contact with the genitals. However, contrary to some beliefs, infection through the use of a common toilet (toilet bowl) is not possible.
Most patients with papillomavirus may not have clear manifestations of condylomatosis, but, meanwhile, they can be spreaders of the infection. Even the treated disease is not a guarantee that the ill person will stop spreading the virus. For this reason, all patients in the sexually mature age should be considered as probable sources of the spread of the virus.
If the patient is the owner of the virus, but he does not have manifestations of the disease, then the corresponding symptoms can be detected already for a month or a year. Unfortunately, as a result, there is no way to accurately calculate the moment of infection with the infection.
Papillomavirus can enter the body even when using a condom during intercourse. Of course, the opportunity to catch using a condom is significantly less than without it. However, it does exist.
There are also known factors that favor the penetration of the virus into the body. These include:
- chronic diseases that have weakened the body's defenses;
- use of certain medicines, in particular, chemotherapeutic drugs, as well as drugs that depress immune defense;
- deficiency in the body of retinol and folic acid;
- smoking;
- immunodeficiency states.
 [7]
[7]
Symptoms of condylomatosis
Condylomatosis in men is most often found in the region of the coronary sulcus of the penis, near the external opening of the urinary tract, on the inner sheet of the preputial sac or along the circumference of the anus.
Condylomatosis in women can be found in the area of the external genitalia, in the perineum and near the anus. In the presence of excess weight, condylomas can be located in the folds of the skin between the inguinal zone and the femoral part, as well as underarms, in the peri-pooch zone, along the lower part of the mammary glands.
The disease is almost equally affected by both men and women. Very rarely condylomatosis is found in childhood and the elderly.
The duration of the incubation period can vary from several weeks to several months (most often about 2 or 3 months).
The disease begins with the appearance of insignificant single papillate villous growths resembling nodules of a pinkish hue. Over time, the growths merge into groups, becoming similar to the chicken comb or the cauliflower inflorescence, located on a thin base (stem). Single growths are found only in some patients. In the majority, there are combinational sprouting, which sometimes merge, acquiring significant dimensions. Often this variant of the disease occurs in patients with overweight, or during pregnancy.
The growths in time become bright red with a cyanotic shade, with signs of maceration, elements of erosion. They can be painful at feeling, sometimes bleed. In the intervals between the nodules accumulate serous-purulent discharge, which sooner or later begin to decompose and exude an unpleasant odor.
Running condylomas tend to malignant, so timely diagnosis is an important stage in the fight against the disease.
Diagnosis of condylomatosis
Condylomatosis has quite typical clinical symptoms, therefore it is often possible to establish a diagnosis based only on the results of an external examination, including examination of the genitals.
In order to detect proliferations of genital warts in the rectum, consultation with the proctologist may be required, with a finger examination. Such an examination is performed if the patient has uncovered the nodules with condylomas in the anus.
In some cases, an anoscopy can be used - examination of the internal surface of the rectum with a special device.
In patients with acquired immunodeficiency, the nodules of condylomas can increase to a considerable extent, forming accumulations that resemble the cauliflower inflorescences (Buschke-Levenshtein symptom). Such sprouting can at any time become a squamous cell carcinoma. In order to exclude this degeneration, a histological analysis of the elements of nodular growth is carried out.
If the doctor suspects the malignant nature of the sprouting, the patient is given a sigmoidoscopy. This procedure allows an assessment of the state of the intestinal wall to a depth of at least 30 cm from the anus.
Absolutely all patients with condylomatosis should pass tests for HIV infection and RW (syphilis).
As a rule, the diagnosis is established by the results of cytology and histology of seized elements of condylomatous growths. In addition, an enzyme-linked immunosorbent assay can detect antibodies to papillomavirus in the blood. It may be designated to remove the DNA of the viral cell from the elements of the pathological tissue using the PCR diagnostic method.
It may also be necessary to consult a venereologist or other narrow specialists.
 [8]
[8]
What tests are needed?
Who to contact?
Treatment of condylomatosis
As a treatment for condylomatosis, diathermocoagulation is prescribed at the base of the growths, freezing with liquid nitrogen (the procedure lasts about 30 seconds, after which the disinfecting and drying agent is applied). If necessary, the procedure can be repeated.
One of the most frequently used methods of treatment is treatment of the growths with an alcohol-containing solution of podophylline (once a day for about 4 days). Podofillin blocks the transport of intracellular nucleotides, thereby slowing down the multiplication of the virus in the cells of the epithelium.
Resorcinol possesses a cauterizing property, in the form of 50% of r-ra or powders.
A good effect also has the following: xeroform 5 g, resorcinol 5 g, tebrofen ointment 5% 10 g. The application of the mixture is combined with treatment of the affected area with novarsenol for 20-30 days.
A positive effect is observed from the administration of interferon (one thousand units per 1 ml of water for injection) into the base of the growths, and also from the lubrication of 5% fluorouracil.
If the growths are localized inside the urinary tract, an administration of fluorouracil is prescribed. It is allowed to use 1% bonaflone, 0.5% colhamine, 5% tebrofen, 3% oxolin ointment 2 to 3 times a day for 15-25 days.
In some cases, on the surface of the growths (in the region of the basement), pherezol is applied - a cauterizing bactericidal preparation. If necessary, the treatment is also carried out a week after the rejection of the scab.
A good effect is observed from the application of the following combination of agents: 0.2 g of prospirin, 1 ml of saline, 1 ml of 0.1% adrenaline, 8 ml of dimethoxide. This method of treatment can be used to treat condylomatosis in pregnancy.
The choice of method of treatment largely depends on the stage of the disease. In some cases, the doctor has to resort to complex treatment, combining radical methods to remove growths with their subsequent drug-induced destruction.
More information of the treatment
Prevention of condylomatosis
Specific prophylaxis of condylomatosis consists in the use of quadrivalent Gardasil vaccine, however this vaccine is effective against only certain types of papillomavirus. This vaccine is under development and can be further improved, creating in the body protection against other types of the virus. Nevertheless, already now there are positive aspects when using this preventive vaccine, which allows to hope for even greater effectiveness in the future.
Nonspecific prevention should be based on hygiene of the skin and mucous membranes, especially around the genitourinary sphere. All diseases of the external genitalia must be treated timely and fully, abstaining from sexual contacts until the moment of complete reconvalescence.
Of great importance is the general strengthening of immunity, adequate nutrition, the rejection of bad habits.
It is important to regularly undergo medical preventive examinations, periodically visit a doctor, even if at the moment there are no clinical manifestations of any disease.
Prognosis of condylomatosis
A significant role in the positive prognosis of condylomatosis is played by timely diagnosis and treatment of the disease. An extremely unpleasant consequence of condyloma in advanced stages may be malignancy. There are data on the degeneration of outgrowths in warty malignant tumors, squamous cell carcinoma.
Patients with condylomatosis should undergo a follow-up check. The doctor observes the general condition of patients, their reaction to ongoing therapy, dynamic indicators of recovery. Permanent monitoring of the doctor is also necessary to prevent a repeated exacerbation of the disease and to prevent malignant degeneration of the growth.
Unfortunately, even after radical removal of foci of the disease, the possibility of re-emergence of genital warts remains. For this reason, the methods of preventing relapses should be used at all times: for this purpose, antiviral and immunomodulating agents are used as prescribed by the doctor.
Condylomatosis is a disease that poses a certain danger to the body, so it is very important not to ignore the disease, but to pay as much attention to it as possible, and to comply with all the doctor's recommendations.

