Medical expert of the article
New publications
What does a flora smear show?
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The results of a microbiological or cytological examination can be given to the patient or sent to the doctor who prescribed the test (gynecologist, urologist, etc.). A special form for bacteriological or cytological examination is provided for recording the results.
Since female genitalia are structurally and functionally different from male genitalia, it is quite logical that the normal microflora of the penis in men and the vagina in women will be somewhat different, which will be reflected in the form with the results of the study.
So, normally a male smear may contain:
Leukocytes (Le) |
Up to 5 in sight |
Erythrocytes (Er) |
Up to 3 in field of view |
Eoinophils (Eo or E) |
Up to 10% of all cells |
Flat epithelium |
Up to 10 in sight |
Mixed opportunistic microflora |
The normal microflora of men may include epidermal, saprophytic and golden staphylococcus, neisseria, pseudomonas and intestinal bacteria, green streptococcus, fecal enterococcus, proteus, corynebacteria, and bacteroides. Some of the above-mentioned microorganisms are not capable of causing diseases, while others (opportunistic pathogens) become dangerous only in large quantities (with active reproduction).
Sometimes a man's smear may contain a small amount of mucus. This happens during sexual arousal the day before or during the smear, but it can also be a sign of an inflammatory process.
Now let's look at the composition of normal microflora during microscopic examination in women:
Indicators |
U |
V |
C |
Leukocytes (Le) |
≤ 10 |
≤ 10 |
≤ 30 |
Erythrocytes (Er) |
No |
No |
No |
Pl.epithelium |
≤ 10 |
≤ 10 |
≤ 10 |
Mucus |
No |
No (moderately) |
No (moderately) |
Other flora |
No (n/a, not found) |
Lactobacilli (high or moderate) |
No (n/a, not found) |
Key cells |
No |
No |
No |
Candida |
No |
No |
No |
Gonococci (Gn) |
No |
No |
No |
Trichomonas (Trich) |
No |
No |
No |
If a certain indicator is not detected in the biomaterial, the analysis form may contain a dash (-) or the words “no”, “n/a”, “not detected”, etc.
Sometimes the test results form contains the signs "+" or "-" instead of letters and numbers. The latter indicates a negative result for a certain indicator, i.e. the absence of a given type of bacteria or cells. The number of "+"s can be used to judge the prevalence of a given type of microflora in the material being tested.
Normal flora in a smear in women does not mean a complete absence of various representatives of opportunistic microflora, their quantity is simply insufficient for the development of inflammation, so it is not even mentioned. The presence of mucus is not a pathology if it is present in moderate quantities. Single leukocytes are also a normal variant, which only indicates the readiness of the immune system to fight off infection.
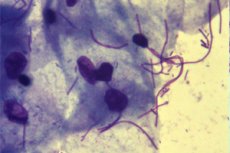
The comparative constancy of the vaginal microflora is supported by lactobacilli (Doderlein bacilli, which make up about 95% of the normal vaginal microflora), which should be present in large quantities in a mature woman's smear. They begin to be produced in girls' bodies as early as adolescence and are responsible for maintaining the acidic environment of the vagina. Feeding on glycogen, these beneficial bacteria produce lactic acid, which creates an environment in the vagina that is unsuitable for the reproduction of harmful microorganisms.
Sometimes you can see the incomprehensible word "lactomorphotypes" in the analysis form. This is another name for lactobacilli, and if lactomorphotypes are present in large quantities in a smear of vaginal flora (at least 90-95%), then a woman should not be afraid, but rejoice, since this indicates a good condition of the vagina. This is the only indicator for which high values are considered an advantage.
But a decrease in the number of lactobacilli is already an alarming symptom, because it indicates a violation of the vaginal microflora. Ideally, the share of other inhabitants of the vagina (coccal and rod-shaped microflora, fungi that constantly live in our body) should account for no more than 5% of the total number of microorganisms. If lactobacilli become less, then the number and composition of other bacteria that are not useful for humans increases, and this already indicates a violation of the health of the female reproductive system.
Lactobacilli are found only in the vagina, and are normally absent from the urethra and cervical canal.
A large amount of flora in a smear is considered a good sign if we are talking about lactomorphotypes, but not about other rod, coccal or other microflora. When microscopically examining the smear material, it is difficult to determine the content of individual types of bacteria in it, so only their total number is taken into account. And if it is more than 5% of the total number of vaginal inhabitants, a woman should pay attention to her health.
The absence of flora in a smear is an unpleasant symptom in any case. The reason for a false result may be careful hygiene of the genitals the day before the analysis, including douching and the use of antibacterial agents. But if a woman prepared for the smear according to all the rules, but the analysis still showed an almost complete absence or a noticeable decrease in beneficial microflora without an increase in pathogenic, this may be evidence of long-term antibiotic therapy in high doses, which simply destroyed the natural defense of the female body and the reproductive system in particular.
This situation is extremely rare. Usually, when lactobacilli are destroyed and vaginal acidity is reduced, fungal microflora begins to actively multiply, which does not die under the action of most antibiotics, and soor (fungi of the genus Candida) are detected in a smear on the flora.
What is vaginal cleanliness?
We are used to thinking that it is clean where there are no microbes. But in relation to the female body, such a definition of cleanliness is not applicable, because the absence of microflora in the smear is considered a violation, and such sterile cleanliness should only be alarming.
Gynecologists, speaking about the true purity of the vagina, which implies the presence of beneficial microflora and the absence of harmful ones, consider 4 degrees of such purity:
- 1st degree is every woman's dream. This is actually an ideal model of the internal vaginal environment, where beneficial lactobacilli (Doderlein's bacilli) dominate, no visible presence of other bacteria and fungi is detected, but the presence of single pure epithelial cells can be noted, the presence of single leukocytes is allowed. The complete absence of fungal mycelium and gram-negative microflora is characteristic. In women living a sexual life, such vaginal flora in a smear is extremely rare. Usually, such a result of smears is noted after sanitation or a short course of antibiotic therapy.
- Stage 2 – a variant of a clean vagina, closer to reality, although there is no need to talk about true cleanliness here. Characteristic is a slight decrease in the number of lactobacilli, an increase in the content of epithelial cells and leukocytes in the biomaterial. The presence of a small number of gram-positive cocci and gram-negative rods, macrophages is possible. This picture is often found in healthy women, rarely accompanied by any specific complaints.
- 3rd degree – here there is no need to talk about cleanliness. The biomaterial shows a significantly reduced content of lactobacilli, other possible inhabitants of the vagina are also found in moderate quantities: the anaerobic species Comma variabile, gram-negative rods and cocci in moderate quantities, gram-positive cocci, colibacilli, and individual trichomonads may also be found. Moderate leukocytosis is also noted, indicating the onset of an inflammatory process or a sluggish disease. In this case, unhealthy microflora prevails over beneficial microflora, which indicates female ill health, i.e. a violation of the biocenosis (vaginal dysbiosis, also known as bacterial vaginosis), which means that additional examination and restoration of the normal vaginal environment are required.
- Stage 4 is an alarming situation when beneficial lactobacilli are not detected in the smear, and the power belongs to opportunistic and pathogenic (gonococci, trichomonads, gardnerella) microorganisms. A moderate number of epithelial cells and an increased content of leukocytes indicate a pronounced inflammatory process. Here, a serious disease is already evident, which must be treated without delay.
Schematically, the assessment of the biocenosis (state of the microflora) of the female vagina can be presented in the form of a table:
Microscopic indicators |
I |
II |
III |
IV |
Lactobacilli |
+++ |
++ |
+ |
- |
Comma variabile |
- |
- |
++ |
++ |
Gram-negative cocci/rods |
- |
- |
++ |
++ |
Anaerobes, streptococci, colibacilli, etc. |
- |
- |
-/+ |
+++ |
Leukocytes |
- |
+ |
++ |
+++ |
Epithelial cells |
Single |
+ |
+ |
++ |
Detection of pathogenic microorganisms in a smear in combination with moderate or severe leukocytosis (increased number of leukocytes) is evidence of an existing disorder, one of the manifestations of which is inflammation, the cause of which is an infection. And if there is an active infection, then the measures to combat it must be serious: further examination with the definition of the pathogen (sometimes it is a combination of microorganisms) and its sensitivity to drugs (usually potent ones: antibiotics, antifungal drugs, combination drugs).

