Medical expert of the article
New publications
Vitiligo
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Vitiligo is a disease characterized by the loss of skin color in patches. The extent and rate of color loss are unpredictable and can affect any part of the body. The condition is not life-threatening and is not contagious. Treatment for vitiligo is to improve the appearance of the affected areas of skin. The disease cannot be cured completely.
Risk factors
At present, a number of antecedent factors can be identified that contribute to the development of depigmentation. These include: psychological, local physical trauma, pathology of internal organs, intoxication (acute or chronic), childbirth, exposure to ultraviolet (or ionizing) rays, burns, etc.
Pathogenesis
In addition, a number of internal and external factors have been identified that play an important role in the development of dermatosis: cytokines and inflammatory mediators, antioxidant protection, oxidative stress, etc. External factors such as ultraviolet radiation, viral infections, chemicals, etc. are also of no small importance.
However, one should also remember the independent or synergistic influence of the above factors, i.e. the multifactorial nature of vitiligo. In this regard, some authors adhere to the convergence theory in vitiligo.
The neurogenic hypothesis is based on the location of depigment spots along the nerves and nerve plexuses (segmental vitiligo), the occurrence and spread of vitiligo often begins after nervous experiences, mental trauma. When studying the condition of the nerves of the dermis in patients, thickening of the basal membrane of Schwann cells is found.
The question of the immune system's involvement in the pathogenesis of vitiligo has been debated for a long time. Analysis of changes in immunological parameters in patients with vitiligo has shown that the immune system plays a certain role in the occurrence and development of the pathological process. The presence of a certain deficit in the T-cell (reduction in the total population of T-lymphocytes and T-helpers) and humoral links (reduction in immunoglobulins of all classes), weakening of non-specific resistance factors (phagocytic reaction indicators) against the background of unchanged or increased activity of T-suppressors indicate disturbances in the functioning of the immune system, weakening of immunological surveillance, which, ultimately, can be one of the triggers in the occurrence and development of the pathological process.
The frequent combination of vitiligo with various autoimmune diseases (pernicious anemia, Addison's disease, diabetes, focal alopecia), the presence of circulating organ-specific antibodies and antibodies against melanocytes, as well as the deposition of the C3 component and IgG in the basement membrane zone of vitiligo skin, an increase in the level of soluble interleukin-2 (RIL-2) in the blood serum and skin confirm the involvement of an autoimmune mechanism in the development of this disease.
The frequent combination of vitiligo with diseases of the endocrine glands has suggested the involvement of the latter in the development of vitiligo.
Increased lipid peroxidation (LPO) processes, decreased catalase and thioredoxyreductase activity in vitiligo skin suggested the involvement of LPO in melanogenesis. The presence of vitiligo in family members and close relatives of patients indicates hereditary factors in the development of vitiligo. Analysis of the author's own material and literature data on family cases of vitiligo suggested that individuals with a burdened family history are at risk and may develop vitiligo spots under the influence of certain trigger factors.
Scientists have not yet come to a consensus on the type of inheritance in vitiligo.
Of particular interest is the study of the relationship between vitiligo and the main histocompatibility genes (HLA system). In studies, the most frequently detected HLA haplotypes were DR4, Dw7, DR7, B13, Cw6, CD6, CD53 and A19. However, the frequency of occurrence of haplotypes may vary depending on the population being examined.
Symptoms vitiligo
A vitiligo spot is a white or milky-white depigmentation with clear borders, oval shape, and various sizes. The spots can be separate or multiple and are usually not accompanied by subjective sensations. In the normal course, the surface of the vitiligo lesion is even, smooth, and there is no atrophy, telangiectasia, or peeling. This is a general definition of vitiligo.
The color of the vitiligo spot depends on the skin type and the preservation of the melanin pigment in the lesion. The depigmented lesion is usually surrounded by a normally pigmented zone.
In trichrome vitiligo, there is a light brown zone where the central depigmented zone transitions into the surrounding brown (or dark brown) normally pigmented zone. This intermediate zone varies in width and is clearly visible under a Wood's lamp. The trichrome vitiligo spot is often located on the trunk and is usually found in people with dark skin.
In some patients, the depigmented spot may be surrounded by a hyperpigmented zone. The presence of all these colors (depigmented, achromic, normal and hyperpigmented) allowed this type of vitiligo to be called quadrichrome vitiligo (four-color)
In punctate vitiligo, small, pinpoint depigmented spots are visible against a background of hyperpigmented or normally pigmented skin.
Inflammatory vitiligo is rare. It is characterized by redness (erythema), usually at the edges of the vitiliginous spot. It is noted that its presence is a sign of progression of vitiligo.
Under the influence of various irritants or solar insolation, vitiligo spots (when localized on open areas of the skin - chest, back of the neck, back of the hands and feet) infiltrate, thicken, the skin pattern changes, which leads to lichenification of the lesion, especially its edges. This variant of the disease is called vitiligo with raised borders.
It should be remembered that foci of depigmentation can also appear at the site of long-standing inflammatory skin diseases (psoriasis, eczema, lupus erythematosus, lymphoma, neurodermatitis, etc.). Such foci are usually called postinflammatory vitiligo and are quite easy to distinguish from primary vitiligo.
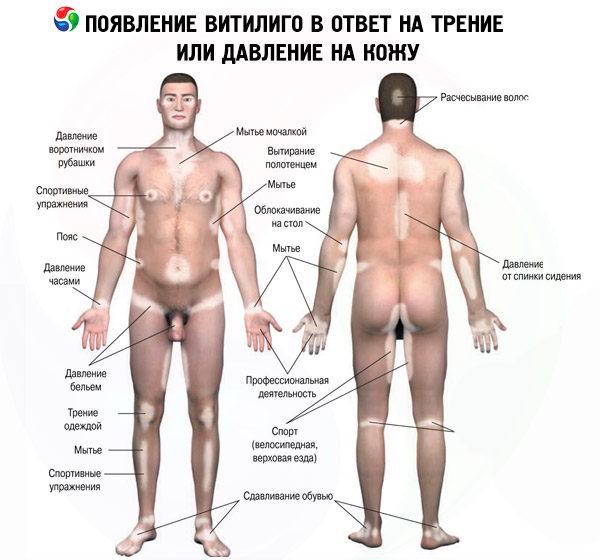
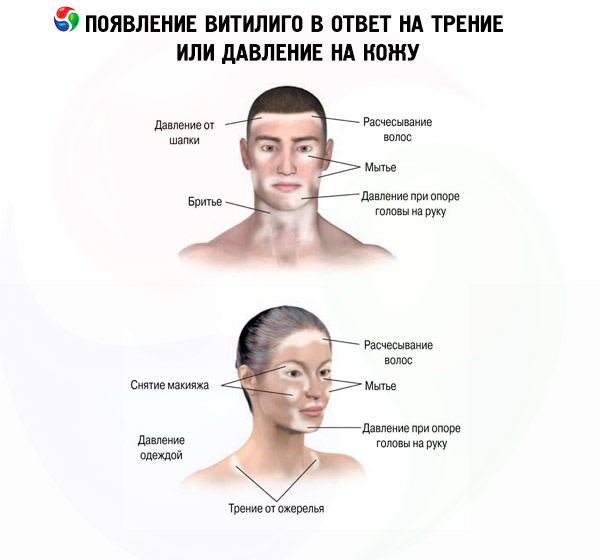
Depigmented spots may be located symmetrically or asymmetrically. Vitiligo is characterized by the appearance of new or an increase in existing depigmented spots in the area of exposure to mechanical, chemical or physical factors. This phenomenon is known in dermatology as an isomorphic reaction, or the Koebner phenomenon. In vitiligo, after skin changes, the most common is hair discoloration, called leukotrichia ("leuko" - from the Greek white, colorless, "trichia" - hair). Usually, the hair located in vitiligo spots on the head, eyebrows and eyelashes is discolored when depigmented spots are localized on the head and face. Damage to the nail plates in vitiligo (leukonychia) is not a specific symptom and its frequency of occurrence is the same as in the general population. Vitiliginous spots at the onset of the disease in most patients have a round or oval shape. As the lesions progress, increase in size or merge, the shape of the lesion changes, taking the form of figures, garlands or a geographic map. The number of spots in vitiligo ranges from single to multiple.
Stages
In the clinical course of vitiligo, the following stages are distinguished: progressive, stationary and the repigmentation stage.
Most often, a single localized spot is observed, which may not increase in size for a long time, i.e. be in a stable state (stationary stage). It is customary to speak of the activity or progression of vitiligo when new or old foci of depigmentation appear within three months before the examination. However, with the natural course of vitiligo, after a few months, new depigmented spots appear near the primary or on other areas of the skin, i.e. vitiligo begins to progress slowly. In some patients, an exacerbation of the skin pathological process occurs within a few days or weeks after the onset of the disease, or several depigmentations appear one after another on different areas of the skin (head, torso, arm or leg). This is a rapidly progressing stage, the so-called vitiligo fulminans (lightning vitiligo).
All the above clinical symptoms (leukotrichia, Koebner phenomenon, family cases, hair and mucous membrane lesions, duration of the disease, etc.) in most cases predetermine the progression of vitiligo or are often found in patients with an active skin pathological process.
Forms
The following clinical forms of vitiligo are distinguished:
- localized form with the following varieties:
- focal - there are one or more spots in one area;
- segmental - one or more spots are located along the course of nerves or plexuses;
- mucous - only mucous membranes are affected.
- generalized form with the following varieties:
- acrofascial - damage to the distal parts of the hands, feet and face;
- vulgar - a multitude of randomly scattered spots;
- mixed - a combination of acrofascial and vulgar or segmental and acrofascial and (or) vulgar forms.
- universal form - complete or almost complete depigmentation of the entire skin.
In addition, there are two types of vitiligo. In type B (segmental), depigmented spots are located along the course of nerves or nerve plexuses, as in herpes zoster, and are associated with dysfunction of the sympathetic nervous system. Type A (non-segmental) includes all forms of vitiligo in which dysfunction of the sympathetic nervous system is not observed. Vitiligo of this type is often associated with autoimmune diseases.
Repigmentation in a vitiliginous lesion can be induced by sun rays or medical treatment (induced repigmentation) or appear spontaneously, without any action (spontaneous repigmentation). However, complete disappearance of lesions as a result of spontaneous repigmentation is very rare.
The following types of repigmentation are distinguished:
- peripheral type, in which small pigment spots appear along the edge of the depigmented lesion;
- perifollicular type, in which small pinhead-sized dots of pigment appear around the hair follicles on a depigmented background, which then increase centrifugally and, if the process proceeds favorably, merge and cover the lesion;
- solid type, in which a barely noticeable light-brown solid shadow first appears on the entire surface of the depigmented spot, then the color of the entire spot becomes intense;
- marginal type, in which the pigment begins to creep unevenly from the healthy skin into the center of the depigmented spot;
- mixed type, in which a combination of several of the above-described types of repigmentation can be seen in one lesion or in adjacent lesion. The most common combination is the perifollicular marginal type of repigmentation.
What do need to examine?
How to examine?
Differential diagnosis
In practice, it is often necessary to differentiate vitiligo from secondary depigment spots that arise after the resolution of primary elements (papules, plaques, tubercles, pustules, etc.) in diseases such as:
However, depigmented spots can be primary elements in other diseases ( non-pigmented nevus, syphilis, albinism, leprosy, etc.) and syndromes (Vogt-Koyanogi-Harada, Alszandrini, etc.).
Who to contact?
Treatment vitiligo
There are two fundamentally opposite methods of treating vitiligo, aimed at creating uniform skin pigmentation. The essence of the first method is to bleach small normally pigmented areas of the skin, located against the background of continuous depigmentation. The second method is more common and is aimed at enhancing pigmentation or using various cosmetics to mask the skin color defect. This method of treatment can be carried out both surgically and non-surgically.
In the treatment of vitiligo, many dermatologists use a non-surgical method, which includes phototherapy (PUVA therapy, short-wave ultraviolet B-ray therapy), laser therapy (low-intensity helium-neon, Eximer-lazer-308 im), corticosteroids (systemic, local), therapy with phenylalanine, khellin, tyrosine, melagenin, local immunomodulators, calcipatriol, pseudocatalase, herbal preparations.
In recent years, with the development of microsurgery, microtransplants of cultured melanocytes from healthy skin into the vitiligo lesion have become increasingly common.
A promising direction is the use of a combination of several non-surgical, as well as surgical and non-surgical methods of treating vitiligo.
In PUVA therapy, 8-methoxypsoralen (8-MOP), 5-methoxypsoralen (5-MOP), or trimethylpyropene (TMP) are often used as photosensitizers.
In recent years, there have been reports of high efficiency of phototherapy with a wavelength of 290-320 nm. However, such (Broad-band UVB Phototherapy) UVB therapy turned out to be less effective than PUVA therapy, which is the reason for the unpopularity of this treatment method.
Local FTX is used in cases where the patient has a limited form of vitiligo or lesions occupy less than 20% of the body surface. A 1% solution of oxaralen is used as a photosensitizer abroad, and in Uzbekistan (and in the CIS countries) - ammifurin, psoralen, psoberan in the form of a 0.1% solution.
There are many reports on the effectiveness of topical corticosteroids, immunomodulators (elidel, protopic), calcipatriol (daivopsx) in the treatment of the disease.
Bleaching (or depigmentation) of normally pigmented skin in vitiligo is used when the patient's depigmented lesions occupy significant areas of the body and it is practically impossible to cause their repigmentation. In such cases, to color the patient's skin in one tone, small islands (or areas) of normal skin are bleached or depigmented using 20% monobenzoyl ether hydroquinone (MBEH) ointment. First, 5% MBEH ointment is used, and then the dose is gradually increased until complete depigmentation is achieved. Before and after using MBEH, patients are advised not to expose their skin to sunlight.


 [
[