Medical expert of the article
New publications
Types of toe ossicle surgery
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

A bone on the foot that causes pain and discomfort can be operated in more than 200 ways. Not all of them are gentle, so after each operation a different rehabilitation period is needed. Let's look at the most common methods of surgical intervention if an unpleasant bone is located on the big toe.
What surgeries are there to remove the bone?
To remove a bunion, you need to correct the deviation of the big toe, which, when deformed, begins to look outward, not inward. This is the goal of any operation, after which we want to see our legs beautiful and well-groomed. And even stand on a heel again.
These operations are conventionally divided into the following.
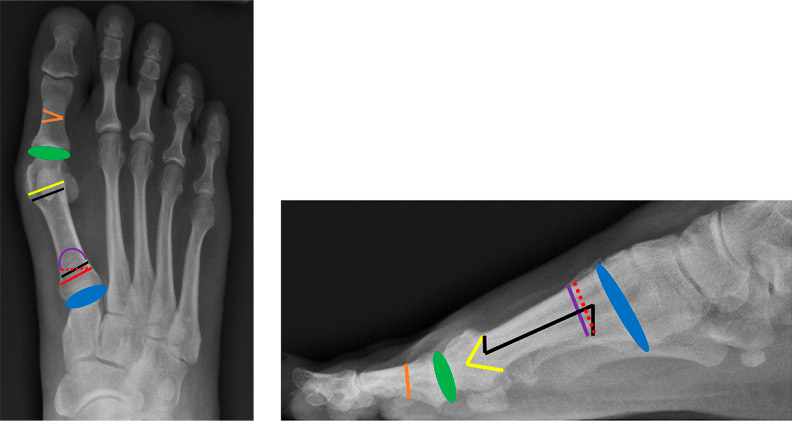
Anteroposterior and lateral views showing various surgical options for hallux valgus correction.
Shown are the Akin osteotomy (orange), metatarsophalangeal fusion (green), distal chevron osteotomy (yellow), scarf osteotomy (black), proximal foramen wedge osteotomy (red), proximal crescent osteotomy (purple), and modified tarsometatarsal osteotomy (TMT) (Lapidus; blue).
Soft tissue surgery
The modified McBride procedure is a distal soft tissue procedure that is primarily used as an adjunct to other hallux valgus correction surgeries such as proximal osteotomy and the Lapidus procedure. This procedure involves releasing the adductor hallux muscle and the lateral sesamoid suspensory ligament. Two surgical approaches have been described: one method involves a medial transarticular approach and the other involves an incision in the first dorsal space. The most common approach is through the first dorsal space due to better visualization and easier access to the lateral soft tissues. In moderate to severe deformities, the modified McBride prosthesis can be used as an adjunct to metatarsal osteotomy. Excellent patient satisfaction rates and significant improvements in AOFAS scores have been reported when combining the modified McBride method with a distal chevron osteotomy. However, the modified McBride technique should not be used in isolation for the treatment of hallux valgus, as data show inferior outcomes and high recurrence rates when used in isolation compared to distal metatarsal osteotomy.[ 1 ], [ 2 ], [ 3 ]
The Akin osteotomy is a closing wedge osteotomy of the first proximal phalanx with a medial base. The Akin osteotomy is usually performed as an adjunct to other procedures such as the distal Chevron osteotomy when the valgus interphalangeal (HVI) angle is > 10 degrees. A longitudinal medial incision is made along the first proximal phalanx and a small wedge of bone is removed. It is important to maintain the integrity of the lateral cortex; otherwise, there is a risk of destabilizing the osteotomy.[ 4 ]
Distal metatarsal osteotomy
Distal chevron osteotomy is indicated for mild to moderate hallux valgus. This procedure is performed by creating a V-shaped incision in the distal metatarsal head/neck with lateral displacement of the distal fragment. The advantage of this procedure is its inherent resistance to dorsiflexion and minimal shortening of the metatarsal. Favorable results have been reported in the literature with distal chevron osteotomy, especially in mild deformities [ 5 ]
The biplanar chevron osteotomy can simultaneously correct mild hallux valgus and reduce the DMAA. (The DMAA is the distal metatarsal joint angle, measured in the anteroposterior projection, and is the angle formed between the distal articular surface and the longitudinal axis of the first metatarsal.) Incisions are made similar to the standard distal chevron osteotomy; however, more bone is removed from the dorsomedial and plantar medial extremities. Additionally, an oblique medial wedge is excised. This allows for lateral movement of the metatarsal head and also restores congruence of the first metatarsophalangeal joint. [ 6 ] Evidence to support this procedure is limited, although patient satisfaction and functional outcomes are favorable. [ 7 ], [ 8 ]
Diaphyseal metatarsal osteotomy
Scarf osteotomy is commonly used to treat moderate to severe hallux valgus. The procedure is performed using 3 separate osteotomy incisions. The first incision involves a longitudinal oblique plantar incision of the proximal and distal diaphysis of the metatarsal bones. A chevron osteotomy is then performed distally in the dorsal cortex and proximally in the plantar cortex with laterally displaced head fragments. Good to excellent results have been obtained using scarf osteotomy. [ 9 ], [ 10 ]
Proximal metatarsal osteotomy is typically reserved for patients with moderate to severe hallux valgus. The most common proximal osteotomies include the proximal chevron, proximal opening or closing wedge, and proximal crescent wedge. A distal soft tissue procedure, such as the modified McBride procedure, is commonly used as an adjunct to proximal osteotomy.
Proximal chevron osteotomy: This procedure involves a medial approach to create a V-shaped incision in the proximal metatarsal with lateral rotation of the metatarsal shaft. The proximal chevron is considered more stable and less technically challenging than other proximal metatarsal osteotomies.[ 11 ] A Level I study of 75 patients with moderate to severe hallux valgus comparing proximal open wedge osteotomy with proximal chevron osteotomy found no significant differences in radiographic results or operative time. Similar clinical outcomes in pain, satisfaction, and function were also noted for both procedures. The study found that the proximal chevron osteotomy shortened the first metatarsal, whereas the proximal opening wedge osteotomy lengthened the first metatarsal.[ 12 ]
Proximal opening or closing wedge osteotomy. The proximal opening wedge osteotomy is a powerful technique for reducing HVA (hallux valgus) as well as increasing the length of the first metatarsal.[ 13 ] Depending on the size of the wedge, the first metatarsal can be lengthened by 2–3 mm. Because of this lengthening, the opening wedge osteotomy can result in tightening of the medial soft tissues and predispose to stiffness.[ 14 ] More recently, attention has shifted to the use of opening wedge plates due to their lower profile.[ 15 ],[ 16 ] The closing base proximal wedge osteotomy has fallen out of favor due to concerns about high recurrence rates, shortening of the metatarsals, osteotomy instability, and dorsal bone malunion.[ 17 ],[ 18 ]
Proximal crescent osteotomy: This osteotomy involves creating a crescent-shaped cut in the bone 1 cm distal to the first joint using a crescent saw, and then the distal fragment is laterally rotated and fixed with screws, Kirschner wires, or dorsal plates. High patient satisfaction and excellent results have been reported with significant improvement in HVA and IMA (intermetatarsal angle of the 1st–2nd bones) in patients with severe hallux valgus.[ 19 ],[ 20 ] The difficulty with this procedure is achieving stable fixation of the osteotomy site, as instability can lead to malunion of the dorsal bone. A Level I study comparing proximal crescent osteotomy with proximal chevron osteotomy in moderate to severe hallux valgus found no significant differences in IMA correction or functional outcomes between the two techniques. Shorter healing times were noted with proximal chevron osteotomy. In this study, proximal crescent osteotomy resulted in greater metatarsal shortening and greater dorsal union failure.[ 21 ]
Arthrodesis
First tarsometatarsal arthrodesis (TMT) (modified Lapidus) The modified Lapidus procedure is traditionally used to treat moderate to severe hallux valgus in patients with first ray hypermobility, in addition to hallux valgus with associated pes planus arthritis or first first tarsometatarsal arthritis. This procedure involves fusion of the first joint with angle correction and is usually combined with a distal soft tissue procedure. Patients are typically kept non-weight bearing for several weeks to prevent first ray elevation and nonunion, which is considered a disadvantage of the procedure.
First metatarsophalangeal joint arthrodesis. First metatarsophalangeal joint fusion is indicated for hallux valgus in patients with degenerative changes in the first metatarsophalangeal joint, as well as in patients with rheumatoid arthritis as part of forefoot reconstruction. First interdigital joint fusion is also a powerful corrective measure for elderly patients with hallux valgus or as a salvage procedure after previous hallux valgus surgery has failed.[ 22 ]
Rotational osteotomy
Recently, attention has been given to techniques that take into account the three-dimensional nature of hallux valgus, especially frontal plane rotation (pronation/supination). Various rotational osteotomies have been described, including the rotational scarf osteotomy, Ludlow osteotomy, and proximal hole wedge osteotomy.
Minimally invasive surgery
Percutaneous and minimally invasive surgical (MIS) techniques have emerged over the past decade due to the potential benefits of less soft tissue trauma, reduced operative time, and faster recovery. Percutaneous techniques are typically used in patients with mild hallux valgus. Several techniques have been described, such as the minimally invasive Chevron and Akin procedures, arthroscopic techniques, subcapital osteotomy technique, and the simple, effective, rapid, and inexpensive (SERI) technique. The SERI technique involves fixation of the osteotomy with a Kirschner wire. [ 23 ], [ 24 ], [ 25 ] Although early clinical and radiographic results of MIS are promising, most studies have a low level of evidence, and further long-term comparative studies are needed.
Physiotherapy
To strengthen the foot and restore blood flow, to prevent muscles, ligaments and tendons from stagnating, the doctor prescribes therapeutic exercise. They start doing it on the fourth day after the operation. First, the foot traction is removed, then gauze rolls are inserted between the toes - the first and second - to correct the position of the toes.
Orthopedic shoes
Approximately a week after the operation and physiotherapy, a person who has undergone surgery according to Schede-Brandes is recommended to wear shoes with special orthopedic insoles, made to order, taking into account the peculiarities of the foot. They are made quickly - in just half an hour. The insole should have a layout of the transverse arch and longitudinal arch of the foot. At the same time, for some time (a week or two) between the toes, the first and second, inserts remain to correct their position.

