Medical expert of the article
New publications
Types of moles on the body
Last reviewed: 08.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
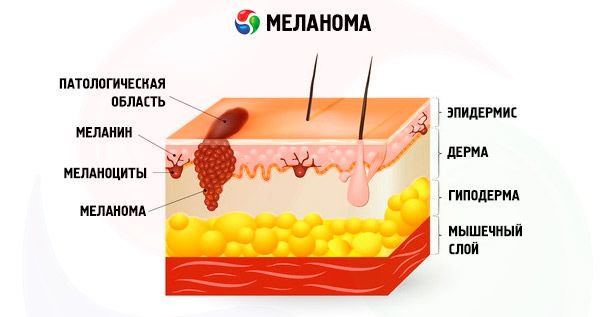
Before determining what types of moles exist, it is necessary to understand: what is a mole? It is a benign skin neoplasm that occurs when pigmented skin cells degenerate into melanocytes. In other words, a large accumulation of melanocytes in one place is that very mole.
A mole can be congenital or acquired, i.e., appearing after birth. The reason why ordinary cellular structures degenerate into melanocytes is not yet known for certain. The appearance of a larger number of skin growths during puberty and pregnancy suggests that this phenomenon may be associated with an increase in hormonal levels in the body. Factors such as ultraviolet radiation, trauma, and long-term treatment with hormonal drugs also influence the appearance of moles.
First of all, moles differ in size. They are:
- gigantic (spreading over the entire face, back or limb);
- large (more than 1 dm);
- medium (up to 1 dm);
- small (up to one and a half centimeters).
Based on the location of moles in the skin layers, they are divided into:
- epidermal (located in the upper layer of the skin);
- intradermal (located deep in the skin);
- borderline (located between the dermis and the epidermal layer).
The general classification of moles is as follows:
- vascular neoplasms (or so-called hemangiomas) are raised spots of a bluish, pink or red color;
- non-vascular formations are keratinized nodules, the color of which ranges from light gray to dark, almost black;
- Setton's moles are benign nevi located in a ring of unpigmented skin;
- blue neoplasms - are dense, protruding spots with a glossy bluish-blue surface;
- dysplastic neoplasms are multiple groups of nevi that differ in diameter and shape and are transmitted genetically;
- Lentigo are spots up to 1.2 cm in size, with jagged outlines, brown or brownish-red in color.
In addition to the above, in dermatology and oncology it is customary to divide moles into dangerous (which are potentially capable of degenerating into melanoma) and non-dangerous (which have an exclusively benign prognosis).
Types of dangerous moles
Dangerous birthmarks can degenerate into a malignant tumor as a result of trauma (both mechanical, chemical or radiation), as well as due to external exposure to ultraviolet light or certain cosmetic procedures.
The following neoplasms transform into melanoma:
- A blue mole is a compacted rounded node without hair follicles, up to 0.5 cm in diameter, with clearly defined edges, a bluish tint. It is located mainly on the arms and legs, in the facial and gluteal area;
- Nevus of Ota is a neoplasm in the facial area that looks like a pigmented bluish-gray spot with a smooth surface;
- pigmented borderline mole is a flat dark bump with a glossy surface, up to 1 cm in size, which is located on the palmar or plantar surfaces, near the nails and on the external genitalia;
- A giant pigmented mole is a growth with an uneven, cracked surface, dark gray in color, which grows as a person grows;
- Dubreuil's melanosis is a typical precancerous skin condition that appears as a separate pigmented spot with unclear borders and slow growth. The spot gradually darkens, acquiring a color from light brown to almost black. The spot is usually located on exposed areas of the body, in particular, on the face.

Types of malignant moles
There are several classifications of malignant birthmarks in the world. However, the most popular is the following clinical classification.
- A superficially spread mole is a spot that can develop on clean skin or grow out of other birthmarks. Such a formation is located on the shoulders and upper back, or on the legs, and has the appearance of a flat bulge with blurred and irregular outlines. The surface of the mole has a mosaic appearance - alternating areas of dark and flesh color. At the beginning of development, a superficially spread formation increases in size along the plane. Later, a node appears, which is damaged and bleeds quite quickly, moving to a new stage - a persistent ulcer with transparent exudate.
- Malignant lentigo is a disease typical for older people. The formation occurs in the face or neck area and looks like a flattened spot of a fairly large diameter (25-50 mm). The color is from dark brown to black.
- Acral lentigo is a tumor that occurs after the age of 50, mainly in men. There are subungual and palmoplantar forms of the disease, which are dark spots that gradually turn into nodes, papules and ulcerated surfaces.
- A nodular mole is the most malignant type of melanoma, rapidly growing deep into the tissues. Externally, the disease looks like a nodule or polyp of almost black color, with a clearly defined border. Formations are located in the upper part of the body or on the limbs.
Types of red moles
Red birthmarks are called angiomas. They are differentiated depending on the degree of deepening of the neoplasm, as well as the type of vessel that the birthmark consists of.
- Most often, a red mole is a capillary angioma, which occurs due to a change in capillary vessels. This pathology has the appearance of a bluish-purple or cherry spot located in any area of the skin.
- Sometimes there is a cavernous hemangioma, which consists of several different vessels that form a cavity. The red hemangioma rises above the skin surface, and its surface is covered by the epidermal layer. The most common location of such a tumor is the face.
- Another type of red mole is a branched angioma, a pulsating tumor with blood content. Usually, such angioma is a cluster of several ordinary moles. When pressing a finger on a branched tumor, you can notice its pallor.
Red moles can be pinpoint or spider-like (when small capillaries extend from the formation).
According to their tissue structure, moles can be branched, flat, cone-shaped or nodular.
Types of hanging moles
Hanging moles are initially benign formations that develop from epithelial tissue and look like a small nodule or papilla, as if hanging from the surface of the skin. The surface of hanging formations is often bumpy, reminiscent of a cauliflower inflorescence; the color is almost any, from light to brown.
Hanging moles are classified depending on their location:
- hanging birthmark in the neck area;
- mole in the armpit area;
- moles in the groin area;
- hanging moles on other parts of the body.
A hanging mole should not be confused with a tumor on a stalk. Hanging moles do not have an elongated tail from which a rounded formation hangs, this is the variant that is a mole on a stalk. A hanging nevus has a wide base, extending directly from the surface of the skin.
Types of convex moles
Convex moles develop in a deeper layer of the epidermis and look like smooth or nodular neoplasms up to 1 cm in diameter, often with hairs growing on the surface. The shades of the convexities are any, from pale yellow to dark.
Convex moles can be represented by the following types:
- epidermo-dermal moles – often rise above the skin of the soles, palmar surfaces and groin area;
- complex moles - are a small or large dark-colored bump located in the epidermis and dermis at the same time;
- Intradermal moles are a general name for all convex moles, regardless of color shade and location.
A neoplasm that rises above the skin surface is most easily injured, so convex moles can eventually transform into a malignant tumor. Because of this, it is necessary to constantly monitor the growth of the spot and record any changes in color, shape or structure.
It is quite difficult to independently determine the types of moles and the degree of their benignity. Therefore, when they appear or change, it is necessary to consult a doctor - a dermatologist or surgeon, who will assess the likelihood of degeneration of the formation.

