Medical expert of the article
New publications
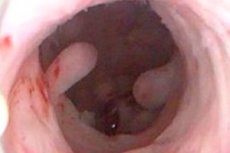
Types of endometrial polyps: simple, fibrous, cystic polyps
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The growth of tissue over the endometrial mucosa is a polyp. Let's consider the main reasons for its appearance, symptoms, types, diagnostic and treatment methods.
Endometrial polyp is a fairly common gynecological anomaly that affects about 10% of women at a young age and more than 40% after menopause. The endometrium is the mucous layer of the uterine cavity, abundantly supplied with blood vessels. It consists of several structures and performs the function of optimal implantation of the blastocyst in the uterus. It is also part of the placenta, which supplies the embryo with oxygen and nutrients.
The exact causes of neoplasia have not been established, but a number of factors have been identified that can cause it:
- Hormonal imbalance.
- Age over 35 years.
- Endometriosis, fibroids.
- Chronic inflammatory processes in the uterus and its structures.
- Endocrine pathologies.
- Frequent abortions, miscarriages.
- Obesity and hypertension.
- Long-term use of sex hormones, glucocorticosteroids.
- Incomplete removal of the placenta after abortion or childbirth.
- Long-term intrauterine device.
- Surgical interventions on the ovaries and uterus.
- Ectopic hormone-producing tumors.
- Diseases of the liver, intestines, bile ducts.
- Violation of the immune state of the body.
- Long-term stress conditions and psychological stress.
- Hereditary factor.
Local intrauterine neoplasm occurs due to pathological proliferation of cells of the functional or basal layer of the uterine mucosa. Growths can form on an unchanged membrane or against the background of hyperplastic processes.
Types of polyps by etiology:
- The functional layer of the endometrium is most susceptible to changes during the menstrual cycle. In the absence of fertilization, it is rejected from the basal layer. In case of incomplete rejection, a functional polyp is formed, which consists of glandular and stromal cells. During menstruation, the growth undergoes the same changes as the entire endometrial layer.
- Glandular and glandular-cystic growths with/without adenomatous changes are formed from the cells of the basal layer. If neoplasia occurs in the isthmic part of the uterus, it usually consists of cells characteristic of the mucous membrane of the internal os of the cervix of the organ, i.e. endometrial or epithelial tissues.
The main types of polyps according to histological (pathological and morphological) characteristics:
- Fibrous – formed from fibrous connective tissue cells. May contain collagen fibers, isolated glands or non-functional epithelial cells. Consists of vessels with thickened sclerotic walls.
- Glandular-fibrous – occurs very rarely and usually in women with stable menstruation. Consists of glands of different lengths and shapes, the lumens of which are unevenly expanded or stretched. In the upper layers of the tumor there is a large number of stromal cells. Closer to the base, the structure of the growth is denser and may consist of fibrous tissue. The walls of the vessels are thickened, sclerosed. There are circulatory disorders and inflammatory processes.
- Adenomatous – develops extremely rarely and is characterized by increased proliferation of glandular tissues throughout the polyp with focal ingrowths of epithelial cells with altered structure from the glands. May contain morphological structures of other types of polyps.
Despite the variety of forms, the clinical signs of the pathology do not have specific features. Based on this, the symptoms of the growth largely depend on its type, size and localization in the uterine cavity.
Common symptoms for all types of endometrial polyps:
- Whitish discharge from the genital tract.
- Menstrual cycle disorders.
- Bleeding after physical activity or sexual intercourse.
- Pain during intercourse.
- Spotting and heavy bleeding during postmenopause.
- Pain in the lower abdomen.
- Infertility.
The main method of diagnosing local intrauterine formations is abdominal and transvaginal ultrasound. The mandatory set of studies includes hysteroscopy with scraping. Diagnostic curettage is necessary for further pathomorphological examination of tissues. Treatment depends on the size and number of neoplasms. If this is a single neoplasm, it can be removed in a laboratory under local anesthesia.
Which endometrial polyp is the most dangerous?
Polyps are benign growths in the uterus caused by the growth of its inner layer. Such growths can be either single or multiple. Their sizes range from 1-2 mm to 80 mm or more, as a rule, this is an oval/round neoplasm on a stalk or a wide base. One of the features of growths is that they do not cause bright clinical symptoms. Their presence can only be confirmed using instrumental methods.
The danger of polyps of any kind is that over time they can degenerate into malignant tumors. That is why regular gynecological examinations are necessary. Degeneration of growths occurs under the influence of various factors:
- Metabolic disorders.
- Decreased immune system defenses.
- Acute and chronic diseases of the body.
- Various intoxications.
- Unfavorable environmental conditions.
- Emotional tension and more.
Any of the above factors, as well as their interaction, leads to the cells changing their characteristics. Tissues become atypical, undifferentiated and begin to actively grow. The presence of atypical cells indicates malignant degeneration. After a comprehensive diagnosis, the patient is prescribed long-term therapy according to the rules of oncology treatment.
Another danger of local intrauterine formations is infertility. Very often, growths appear due to hormonal disorders, which in turn cause problems with the menstrual cycle. If diagnosed in time, they are removed, and the woman is prescribed restorative hormone therapy. This allows normalizing reproductive functions.
It should also be noted that all types of endometrial polyps are accompanied by prolonged and frequent bleeding. This may be heavy periods after a long delay or intermenstrual bleeding, spotting. In any case, during blood loss, hemoglobin (protein and iron) leaves the body along with red blood cells.
Against this background, iron deficiency anemia may develop. The woman complains of constant weakness, headaches and dizziness, general malaise. Due to the lack of oxygen, all tissues and organs suffer. Treatment consists of hormonal correction, surgical removal of neoplasms in the uterus and fairly long-term therapy for anemia.
Simple endometrial polyp
The uterine cavity is lined from the inside with a mucous membrane, i.e. the endometrium. It consists of a basal and functional layer. During the menstrual cycle, the functional layer grows from the basal layer. If fertilization does not occur, it is rejected during the next menstruation.
A simple endometrial polyp is formed by incomplete rejection of the functional layer. Very often this occurs against the background of hyperplasia and polycystic ovary syndrome. The local intrauterine formation can consist of cells of both basal and functional structure.
- Functional growths are round or oblong, ranging in size from 1-2 mm to 8 mm or more. They can be rejected during menstruation, so they do not require treatment or removal.
- Growths from the basal layer are not rejected during menstruation and are not affected by medications, so they require surgical removal (hysteroresectoscopy).
Most often, tissue growth does not cause any symptoms. But in some cases, intermenstrual bleeding, prolonged periods, spotting and pain after intercourse or physical activity, and infertility appear.
A simple endometrial polyp is diagnosed using ultrasound. Ultrasound is performed before and after menstruation. This allows you to determine the type of growth: functional, basal. For treatment, drugs that improve the rejection of the endometrium can be prescribed. If the ultrasound does not reveal neoplasia, but there are signs of its presence, then aspiration biopsy and curettage are indicated. The obtained tissues are sent for histology, based on the results of which a plan for further therapy is made.
Fibrous polyp of the endometrium
This type of neoplasms refers to benign connective tissue tumors that grow from the inner lining of the uterine cavity. One of the features of the fibrous polyp of the endometrium is that it is formed by connective tissue. In rare cases, it contains glandular cells.
The growth can be on a stalk or a broad base, both single and multiple. Most often it is located at the bottom of the uterus or in the mouths of the fallopian tubes. The sizes vary from microscopic 1-2 mm to large 5-8 cm or more.
If the polyps are small, they are asymptomatic and can only be detected by ultrasound. With large growths, intermenstrual bleeding, prolonged irregular menstruation, and discharge during menopause and postmenopause appear. Cramping and nagging pain in the lower abdomen and a general deterioration in well-being are possible.
In most cases, fibrous growths are formed against the background of hormonal imbalances and due to low estrogen levels. The causes of the disorder also include:
- Chronic endometritis – inflammation of the mucous membrane provokes a disruption of tissue trophism and causes hyperplastic processes.
- Complications during the birth process and termination of pregnancy.
- Endometrial trauma caused by long-term use of an intrauterine device, after diagnostic or therapeutic procedures.
- Endocrine and vascular diseases.
- Reduced immunity.
Neoplasia is formed when humoral and cellular immunity is impaired. The pathological process is based on local inflammatory, atrophic and post-traumatic processes that ensure tissue growth.
Diagnostics begins with a gynecological examination of the patient and collection of anamnesis. After this, an ultrasound examination and contrast radiography of the uterus are performed. The complex of mandatory tests includes hysteroscopy with histology. Fibrous tissues are differentiated from other forms of neoplasms of the body and cervix.
Fibrous polyp is characterized by a low level of vascularization and proliferation. Such growths are insensitive to hormones, so hormonal correction is ineffective. For treatment, curettage of the uterine cavity and hysteroresectoscopy are performed.
The risk of their malignancy is about 0.5%. But without treatment, they can cause infertility. Necrosis is also possible, since under the influence of infectious agents or in the process of pinching, the tissue of the growth can die and decompose. The pathological process occurs with inflammation and acute intoxication.
Cystic endometrial polyp
The inner surface of the uterus is the endometrium. It is rejected during the menstrual cycle and comes out with bloody discharge. But due to the action of some factors, the mucous membrane does not come off completely, which leads to damage to its structure and intensive growth. Cystic growths of a benign nature are formed on it.
Such neoplasms are cystic polyps of the endometrium. The neoplasia contains mucous secretion, which accumulates in the lumens of the twisted glands and gradually increases in size.
Causes of pathology:
- Dysfunction of the adrenal and thyroid glands.
- Diabetes mellitus.
- Hypertension.
- Obesity.
- Genetic predisposition.
The main symptoms of the disease:
- Menstrual and ovulatory cycle disorders.
- Discharge from the genital tract before or after menstruation.
- Heavy uterine bleeding not associated with the menstrual cycle.
- Pain in the lower abdomen.
- Dizziness and general weakness.
- Discomfort and pain during sexual intercourse.
- Infertility.
The appearance of the above symptoms is a reason to see a doctor and undergo a comprehensive gynecological examination. The main diagnostic method is an ultrasound examination of the uterus.
The treatment is surgical, polyps are removed surgically (hysteroscopy). The site of their growth is treated cryosurgically using liquid nitrogen. Scraping of the mucous surface is also indicated to reduce the risk of relapse. The patient is prescribed hormonal therapy, which is aimed at restoring the normal functioning of the reproductive system.
 [ 1 ]
[ 1 ]
Adenomatous polyp of the endometrium
Another type of endometrial polyps is adenomatous local intrauterine formations. In addition to the uterus, such growths can form in the rectum and colon, on the mucous membrane of the stomach, intestines. Externally, the neoplasia can be in the form of a tubercle or stand on a leg.
The adenomatous type contains glandular epithelium with signs of proliferation, i.e. structural reorganization of the glands. One of the features of such a formation is that it has prerequisites for developing into endometrial cancer.
Causes of pathology:
- Complications of surgical intervention, abortions, miscarriages, curettage.
- Chronic inflammatory processes in the uterus.
- Hormonal imbalance.
- Venereal diseases.
- Reduced immune system.
- Hereditary predisposition.
- An intrauterine device that has been incorrectly installed or has been in place for a long time.
Symptoms of the pathology are manifested by menstrual cycle disorders, intermenstrual bleeding, and increased amount of discharge during menstruation. There may be pain in the lower abdomen that radiates to the intestines. During sexual intercourse, discomfort and painful sensations occur. Such symptoms are a reason for immediate medical attention.
Without timely diagnosis and treatment, an adenomatous polyp can cause infertility and malignant degeneration. Treatment is surgical. A gynecologist-oncologist evaluates the size of the growth; if its size is more than 2 cm, then the risk of developing cancer is about 10-20%. During the surgical intervention, the uterine cavity is scraped out, removing the neoplasm. After this, complex restorative therapy is prescribed.
Particular attention should be paid to preventive measures. It is recommended to undergo regular gynecological examinations, exclude casual sexual relations and bad habits. It is necessary to protect yourself from unwanted pregnancy and subsequent abortion with trauma to the uterus.
Functional endometrial polyp or functional type polyp
An endometrial polyp is a growth on the inner lining of the uterine cavity. It is formed due to abnormal tissue growth. A functional or pseudopolyp affects only the endometrial stroma. It is formed due to incomplete rejection of the mucous membrane during menstruation. The tissues of the neoplasm can change during the cycle. Its cells react to the action of sex hormones and surrounding tissues.
According to histological characteristics, the functional type growth has several types:
- Hyperplastic – originates from epithelial cells.
- Proliferative – active growth of mucous tissue due to the inflammatory process.
- Secretory – cell proliferation associated with increased production of secretory fluid.
The causes of neoplasia are associated with local and general hormonal disorders. One of the reasons is local estrogenia, i.e. increased estrogen activity against the background of progesterone deficiency. This deviation develops with endocrine disorders, stress, hypertension, excess body weight, gynecological diseases, inflammation or injury of the uterine mucosa, disorders in the process of tissue reparation.
About 10% of women do not suspect that the mucous membrane of the uterine cavity is affected. This is due to the absence of symptoms due to the small size of the growth. As its tissue grows, the following pathological signs appear:
- Pain during menstruation.
- Menstrual cycle disorders.
- Bloody discharge during the intermenstrual period, during menopause, postmenopause.
- Pulling pain in the lower abdomen.
- Pain during intercourse.
- Spotting bloody discharge after sex.
The appearance of the above symptoms is a reason to contact a gynecologist. The doctor conducts an examination and ultrasound of the uterus. For an accurate diagnosis and determination of the type of neoplasm, therapeutic and diagnostic laparoscopy is indicated. The patient is also prescribed a blood test for sex hormones (testosterone, progesterone, prolactin, estradiol). The tissues taken during laparoscopy are sent for histology to confirm their benign nature.
 [ 2 ]
[ 2 ]
Focal endometrial polyp
Local growth of the uterine mucosa is a polyp. The foci can be single or multiple. In most cases, neoplasia is small in size. At the same time, neoplasms that have formed again after resection can be encountered.
Focal endometrial polyp develops under the influence of various factors. Possible causes of the disease include:
- Hormonal disorders.
- Disorders of the ovaries.
- Endometrial trauma.
- Endocrine diseases.
- Inflammatory diseases of the reproductive system.
- Stress.
The size of the neoplasia most often does not exceed 10 mm, which is why the symptoms of the pathology are blurred. But as the tissue grows, the following symptoms appear:
- Various menstrual cycle disorders.
- Uterine bleeding not associated with menstruation.
- Bloody discharge and pain after intercourse.
- Increased amount of normal discharge (thick, white-tinged discharge).
If a neoplasm is suspected, a set of diagnostic studies is carried out with mandatory ultrasound of the uterus. If the growth is localized in the cervical canal, it is visible during examination of the cervical orifice. Histology of tissue scrapings is indicated to determine its structure.
If you delay visiting a doctor and getting a diagnosis, tissue proliferation can cause a number of complications: posthemorrhagic anemia, severe bleeding, uterine fibroids, strangulation of a neoplasm, hyperplasia, endometrial cancer, polyp necrosis with ischemic changes.
Treatment depends on the type of focal growth, the patient's age, and a number of other factors. The neoplasm may resolve on its own after menopause. In all other cases, surgical treatment, medication, and monitoring of the patient's condition are indicated.
Basal polyp of the endometrium, or basal type polyp
A local intrauterine formation affecting the basal layer of the endometrium is a polyp. In most cases, the growth is benign, but under the influence of certain factors it can develop into oncology. Basal polyps can be single or multiple. They are diagnosed in 5-25% of patients, regardless of age.
The neoplasm originates from the basal layer, but contains glandular cells, stroma and myometrial tissue. If the neoplasm size does not exceed 1-3 cm, the pathology is asymptomatic. But as it grows, menstrual cycle disorders, problems with conception, bloody discharge not associated with menstruation and other symptoms characteristic of all types of endometrial formations occur.
One of the features of the basal type is that, unlike the functional type, it is not rejected during menstruation, i.e. it is not sensitive to hormonal changes. The main method of treatment is surgery. The doctor removes the neoplasm, performs curettage of the uterine cavity and treats the growth site with liquid nitrogen. Subsequently, the patient is prescribed a set of medications to restore the menstrual cycle and reproductive function.
 [ 3 ]
[ 3 ]
Proliferative endometrial polyp, or proliferative type polyp
The endometrium is a mucous layer lining the inside of the uterus. Its functions include implantation and development of the embryo. The menstrual cycle depends on changes in the mucous membrane. One of the causes of disorders in the female body is the proliferation of the endometrium. This concept implies an active process of cell division of the organ tissue. During menstruation, the mucous membranes of the uterus become thinner and the tissues of the functional layer are rejected. This process is caused by proliferation.
The main phases of proliferation:
- Early – its duration is from the 1st to the 7th day of the menstrual cycle. During this period, the uterine mucosa changes. The endometrium contains epithelial cells, the blood arteries are not active, the stroma is similar in structure to a spindle.
- The middle stage is a short stage from the 8th to the 10th day of the cycle. Cell structures formed by indirect division are formed on the mucous membrane.
- Late – from the 11th to the 14th day of the cycle. Convoluted glands, multilayered epithelium, large and round cell nuclei appear on the endometrium.
Proliferative endometrium does not always indicate normal functioning of the reproductive system. In some cases, proliferation is a sign of pathology, when cells actively divide, thickening the mucous layer of the uterus. Against this background, a proliferative endometrial polyp may occur.
A proliferative neoplasm can be of two types - glandular and atypical. In the latter case, the growth contains adenomatous foci, which are localized in the branching of the glands. Transformation of glandular tissue into oncology occurs in 3 out of 100 women.
Signs of proliferative neoplasia:
- Disorder of the menstrual function of the uterus.
- Heavy uterine bleeding.
- Heavy discharge outside of the cycle.
- Breakthrough bleeding with clots.
- Anemia, general malaise, dizziness, weakness.
- Anovulatory cycle.
- Infertility.
To diagnose a pathological condition, the gynecologist collects anamnesis and studies the patient's complaints. A bimanual vaginal examination is performed, a smear is taken and examined microscopically. A transvaginal ultrasound examination is mandatory to determine the thickness of the mucous membrane and identify its pathologies. Hysteroscopy with histological examination of the scraping is also indicated.
Treatment depends on the type of proliferative neoplasm. Therapy can be either conservative or surgical. In the first case, the patient is prescribed drugs to correct the hormonal background. The operation means complete removal of deformed areas of the endometrium with scraping of the uterine cavity.
Hyperplastic endometrial polyp
Focal intrauterine neoplasms arise due to excessive growth of mucosal cells. The growths can be single or multiple, they vary in size, structure and localization in the organ. Hyperplastic endometrial polyp is associated with the following factors:
- Oncological diseases of the genital organs and mammary glands.
- Polycystic ovary syndrome.
- Insulin resistance syndrome.
- Uterine fibroids.
- Chronic endometritis.
Hyperplastic processes are accompanied by uterine bleeding that is not associated with menstruation. Bloody discharge is also observed during menopause. In some cases, the pathology is asymptomatic and can be diagnosed after long unsuccessful attempts to get pregnant.
To diagnose uterine neoplasms, transvaginal ultrasound and curettage of the uterine body mucosa are performed, followed by histology of the collected tissues. Curettage is done on the eve of menstruation. During the operation, the entire endometrium is removed, including at the bottom of the uterus and in the uterine tubal angles. Curettage is performed using hysteroscopy. Further treatment depends on the histology results. If atypical cells are not detected, hormonal correction is performed to restore the menstrual cycle and a number of other disorders.
Endometrial polyp of the cervical canal
The anatomical part of the female reproductive system in the internal genital organs is the cervical canal of the cervix. The success of pregnancy and the birth process depends on its health. One of the structural pathologies of the cervical canal is polyps. Such neoplasms grow from the cylindrical epithelium of the endocervix.
The main causes of cervical canal damage:
- Trauma during obstetric manipulations and during the birth process. Trauma is possible with an incorrectly installed intrauterine device.
- Sexually transmitted infections.
- Structural changes in the surface of the cervix – erosion, leukoplakia.
- Violation of vaginal microflora.
- Nonspecific infection – vaginitis, endomyometritis, vulvovaginitis, cervicitis.
- Ovarian dysfunction – polyposis, myoma.
- Endocrine pathologies – diabetes, obesity, chronic stress.
- Hormonal disorders.
The pathological condition manifests itself in bloody discharge and pain after intimacy. Many women experience menstrual irregularities, profuse leucorrhoea (if infected, it is mucopurulent). If the growth presses on the glands of the cervical canal, then profuse mucous discharge appears. With large neoplasia, nagging pains in the lower abdomen occur.
Without timely diagnosis and treatment, growths in the cervical canal pose a threat to women's health:
- Malignant transformation.
- Risk of uterine bleeding.
- Tumor necrosis and intoxication of the body.
- Hematometra.
- Pregnant women are at risk of spontaneous abortion, low-lying placenta and development of cervical insufficiency.
In most cases, a standard gynecological examination is sufficient to detect pathology. During the examination, thickened and hypertrophied walls of the cervix are determined. Focal tissue growth can block the canal.
Treatment is surgical. First of all, the entire cervical canal is scraped. There are also other surgical techniques used for neoplasia: diathermocoagulation, cryodestruction, laser polypectomy. In particularly severe cases, amputation of the cervix is indicated. The operation is performed in cases of frequent relapses and malignant degeneration of tissues. Such treatment allows preserving the patient's reproductive functions.
 [ 8 ]
[ 8 ]
Endometrial polyp with focal stromal fibrosis
Chronic inflammatory processes and ovarian dysfunction are the main causes of endometrial stromal fibrosis. Against this background, polypous neoplasms and other pathological changes in uterine tissues can form.
The disease has no specific criteria. Most often, patients complain of irregular periods, bloody discharge before or after menstruation, pain and discomfort in the lower abdomen. Diagnosis of endometrial polyp with focal stromal fibrosis is possible only with the help of transvaginal ultrasound examination with tissue sampling for histology.
Treatment is surgical. The growth is removed and the endometrium is scraped using hysteroscopy. The lesion is treated with liquid nitrogen. Drug therapy is used to restore the menstrual cycle and correct hormonal disorders.
Small endometrial polyps
Disruption of uterine endometrial cell proliferation triggers a number of pathological processes, one of which is the growth of polyps. Focal hyperplasia is manifested by abnormal growth of the uterine mucosa in the form of single and multiple growths on a stalk or broad base.
Single small endometrial polyps are asymptomatic, but their large number and gradual increase in size disrupts physiological processes in the uterus. Against this background, the following symptoms arise:
- Uterine bleeding.
- Menstrual cycle disorders.
- Pain in the lower abdomen.
- Pain, discomfort and bloody discharge after intimacy.
- Infertility.
Most often, small multiple neoplasia is localized on the back wall of the uterine cavity and tubal angles. As a rule, it does not go beyond the uterine cavity, but in some cases, the pathology affects the cervical canal.
To determine the problem, the patient is examined and an ultrasound examination is performed. During the diagnostics, submucous hemorrhages due to a large number of small neoplasms, pronounced inflammatory processes, and hyperemia of the basal layer of the endometrium can be detected.
Treatment is surgical. Small growths are removed with a curette using a hysteroresectoscope. The removed tissues are sent for histological examination to confirm their benign nature.
 [ 9 ]
[ 9 ]
Hormonal endometrial polyp
One of the reasons for the formation of endometrial polyps is hormonal imbalances in the body. The uterine mucosa is a target for sex hormones. Estrogens trigger proliferative processes in the endometrium, but with a deficiency of progesterone, this leads to hyperplastic changes. Therefore, in most cases, the disease is associated with hyperestrogenism. Estrogens stimulate active growth of normal, hyperplastic or malignant cells of the mucosa.
Hormonal changes can occur at any age. But most often it is the period of pregnancy and before menopause. Symptoms of intrauterine local neoplasms depend on their size, quantity and location.
Hormonal endometrial polyp has a tendency to active growth and most often refers to the functional type. Treatment of the pathology is surgical followed by drug therapy to restore the balance of estrogens and progesterone.
Secretory polyp of the endometrium
The growth of endometrial polyps is directly related to the menstrual cycle. The period between ovulation and the onset of bleeding is the luteal phase (corpus luteum phase). Its duration is 13-14 days. The corpus luteum secretes androgens, progesterone and estradiol. With increased levels of estrogen and progesterone, the layers of the mucous membrane change. The endometrial glands proliferate and begin to secrete, as the uterus prepares for implantation of the fertilized egg.
In the secretory stage, the endometrium increases significantly in size. Glandular cells that secrete mucus appear in its structure, and the membrane becomes saccular. The secretory endometrium is quite dense with a smooth surface and basal structure. Under the influence of certain factors, growths, so-called secretory (glandular) polyps, may appear on it.
A local intrauterine neoplasm can disrupt the implantation of a fertilized egg. Also, the symptoms of the pathology include changes in the menstrual cycle with prolonged and heavy bleeding, spotting and pain in the lower abdomen. For diagnosis, an intravaginal ultrasound and a set of laboratory tests are performed. Treatment of all types of polypous formations is surgical. The second stage of therapy is the correction of hormonal levels.
Retrogressive endometrial polyp
A local intrauterine formation can form against the background of an unchanged endometrium, as well as in its pathological conditions. Glandular-fibrous growths appear in the stage of atrophy, hyperplasia, proliferation or retrogression, which is characteristic of premenopause.
Retrogressive endometrial polyp is characterized by mosaic coloring. According to histological characteristics, it may contain atypical cells. Very often, such neoplasms occur against the background of inflammatory processes or circulatory disorders, which lead to dystrophic and necrobiotic changes in tissues.
False endometrial polyp
All polypous neoplasms are divided into true polyps and pseudopolyps. The latter include decidual (placental) growths, which are often diagnosed during pregnancy. According to the histological structure, a false endometrial polyp can be glandular, fibrous or adenomatous. The latter type is dangerous due to malignant degeneration.
True and false polyps are differentiated using ultrasound or colposcopy. The histological structure of pseudopolyps is similar to the decidual tissue of the endometrium, but their structure includes glandular components. Between the glands there are wide venous sinuses with different blood filling. Ulcers, absence of the covering epithelium, necrosis or inflammatory infiltration may also be observed.
 [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ]
[ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ]
Endometrial stromal polyp
Stroma is a loose connective tissue, which is represented by cellular structures with vascular tangles at the base. Stromal polyp of the endometrium is diagnosed using histological examination. This diagnosis indicates that stromal components predominate in the structure of the pathological neoplasm.
In its symptoms and cause of occurrence, this type does not differ from other types of polyps. Its treatment is surgical with subsequent correction of hormonal levels.
In glandular growths, the stromal component is poorly expressed, since glandular tissue predominates. If the neoplasm has focal fibrosis of the stroma, the glands are located at different angles, have different lengths and sizes, then such a polyp is stromal. Atypical hyperplasia also contains stromal elements, but in small quantities.
Atrophic endometrial polyp
According to medical statistics, in 95% of cases, polyps in the postmenopausal period develop against the background of atrophic processes of the uterine mucosa. The pathomorphological composition of such neoplasms corresponds to the endometrium. In this case, the highest degree of proliferation is observed with a combination of adenomatous and glandular structures.
Atrophic polyps are most often diagnosed in women over 50 years of age, in patients with chronic inflammatory lesions of the genitourinary system. According to histology, such formations have a greater tendency to malignancy, therefore they require surgical treatment.
Endometrial polyp in menopause, climacteric and postmenopause
The main cause of uterine and cervical polyps is a disruption in hormone production. With the onset of menopause, changes occur in the hypothalamic-pituitary system. The frequency and intensity of secretion of sex hormones are disrupted, and ovarian dysfunction develops. Various types of endometrial polyps can form against the background of physiological processes.
- Women with menopause often develop glandular-fibrous polyps, consisting of endometrial glands and stroma. Such neoplasms are accompanied by pain syndrome and bleed less, since they have a capsule.
- Glandular cystic formations grow rapidly. The polyp occupies most of the uterine cavity, and its capsule merges with the surrounding tissues. Because of this, differentiation is made with endometrial carcinoma.
- Glandular-angiomatous (containing an increased number of stromal elements) have an irregular capsule and shape, heterogeneous structure and increased blood flow.
Postmenopause is a period from the last menstruation, which lasts more than 5-8 years. It is characterized by a complete cessation of ovarian function. This entails serious changes in the female body, as the level of estrogens and progesterone is constantly decreasing. Against the background of such changes, ovarian pathologies, hyperplasia and neoplasms in the uterine cavity can develop. The latter include polyps. Their appearance is caused by atrophic processes of the endometrium and hormonal decline.
The disease manifests itself with spontaneous uterine bleeding and pain in the lower abdomen. Treatment of polyps during menopause and postmenopause is the same as for women of childbearing age. Surgical removal of the growth is performed with its subsequent histological examination. To prevent relapses, the mucous membrane of the uterine body is scraped out, and the foci of excess tissue growth are cauterized with a laser or liquid nitrogen. If it is established that the polyps contain atypical cells, then complete removal of the uterus is possible.
Endometrial polyp and pregnancy
As a rule, a polyp of the uterine mucosa and pregnancy are incompatible concepts, since neoplasia prevents the attachment of the fertilized egg to the uterine walls. But in some cases, polypous growths occur after conception. Their appearance is associated with hormonal changes in the female body and the following factors:
- General decrease in immunity.
- Infections of the genital tract.
- Trauma to the uterine mucosa.
- Weight loss.
- Complications from previous births.
Most often, pregnant women are diagnosed with decidual polyps, which do not pose a threat to the mother or child. They disappear on their own after childbirth and do not require treatment. But such neoplasms require constant monitoring. If the growth has formed in the cervical canal of the uterus, it can become a source of infection for the fetus, provoke premature opening of the cervix and childbirth. In this case, local antibacterial therapy is carried out.
In terms of symptoms, a local intrauterine formation may not manifest itself in any way. But in some cases, women note nagging pain in the lower abdomen, slight bloody or foul-smelling discharge from the vagina. Heavy bleeding may indicate trauma to the neoplasia.
In most cases, doctors do not touch polyps before childbirth, since they can come out on their own, and with surgical intervention there is a high risk of intrauterine and purulent-septic infection. If neoplasia has caused infertility, then after its removal and a course of hormonal therapy, a woman can become pregnant.
In any case, all types of endometrial polyps require timely diagnosis and treatment to minimize the risk of complications and their malignant transformation.

