Medical expert of the article
New publications
Thrombophlebitis of the upper extremities
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
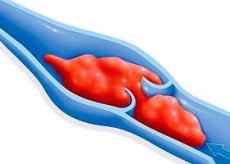
Inflammation of the venous wall, which is characterized by the formation of a thrombus, is called thrombophlebitis. It can develop in both the upper and lower extremities. The disease affects superficial or deep veins in any area. Thrombophlebitis of the upper extremities can develop in any area.
ICD-10 code
Thrombophlebitis is included in diseases of the circulatory system. It is classified according to ICD 10 code as I00-I99. I00-I02 Acute rheumatic fever. I05-I09 Chronic rheumatic heart diseases. I10-I15 Diseases characterized by high blood pressure. I20-I25 Ischemic heart disease. I26-I28 Pulmonary heart disease and disorders of pulmonary circulation. I30-I52 Other diseases of the heart. I60-I69 Cerebrovascular diseases. I70-I79 Diseases of arteries, arterioles and capillaries. I80-I89 Diseases of the veins, lymphatic vessels and lymph nodes, not classified elsewhere. I95-I99 Other and unspecified diseases of the circulatory system.
I80-I89 Diseases of veins, lymphatic vessels, and lymph nodes, not elsewhere classified. I80 Phlebitis and thrombophlebitis. This category includes deep vein thrombosis of the lower extremities, as well as superficial thrombophlebitis. I81 Portal vein thrombosis. This category includes portal vein thrombosis. I82 Embolism and thrombosis of other veins. I83 Varicose veins of lower extremities. This category includes varicose veins. I84 Haemorrhoids. I85 Varicose veins of esophagus. I86 Varicose veins of other sites. I87 Other disorders of veins. I88 Nonspecific lymphadenitis. I89 Other noninfectious diseases of the lymphatic vessels and lymph nodes.
I82 Embolism and thrombosis of other veins. I82.0 Budd-Chiari syndrome.
I82.1 Migratory thrombophlebitis. I82.2 Embolism and thrombosis of the vena cava.
I82.3 Embolism and thrombosis of renal vein. I82.8 Embolism and thrombosis of other specified veins. I82.9 Embolism and thrombosis of unspecified vein.
Causes of thrombophlebitis of the upper extremities
For a thrombus to form, several factors must be present at once. Classical medicine knows three main reasons why thrombophlebitis of the upper extremities occurs. The first factor is a sharp increase in the coagulation activity of the blood. This condition can be caused by: pregnancy, childbirth, diabetes, and genetic predisposition.
The second factor is trauma to the inner walls of the vessels. Thus, it can be subject to traumatization due to injections by people incompetent in this matter. Chemotherapy and radiation therapy can cause trauma.
The third and final factor is slow blood circulation. It occurs against the background of the development of pathological processes, such as varicose veins, immobility of the limbs, and excess body weight.
Thrombophlebitis can develop against the background of one or all factors at once. For example, when a bone is broken, not only does extensive bleeding occur, but the level of coagulation also increases. As a result, an inflammatory process can develop in the veins.
Pathogenesis
Most often, thrombophlebitis develops against the background of mechanical damage. It can be provoked by injuries, childbirth, surgical and gynecological operations. The basis of pathogenesis is the so-called Virchow's triad. It includes the endothelium of the vein wall, slow blood flow and increased blood coagulation activity.
The vascular endothelium plays an important role. This process is accompanied by damage to the extremities, as well as the release of interleukins. They, in turn, activate platelets and the coagulation cascade. The endothelial surface begins to acquire thrombogenicity. These factors lead to the development of a thrombus. Tissue thromboplastins can also lead to the formation of a thrombus. In excess, they enter the bloodstream from damaged tissues.
Compensatory mechanisms may occur simultaneously with these processes. These include: spontaneous, partial or complete thrombolysis and the development of collateral circulation.
Symptoms of thrombophlebitis of the upper extremities
Often, the inflammatory process is formed against the background of varicose veins. The inflammatory process of nearby tissues can lead to blockage of blood vessels. In this regard, symptoms of thrombophlebitis begin to manifest themselves, affecting the upper limbs.
As a rule, everything begins with pain, it can be both moderate and acute. Redness appears, in the place of redness the vein is easily palpated. It becomes rough and heavy. At the same time, body temperature can manifest itself. If this is superficial thrombophlebitis, there is no need to worry, there is no danger to a person. A thrombus cannot break off, which means there is no threat to life. It is important to organize therapy correctly and not allow deep veins to be drawn into the process.
The disease is characterized by the presence of enlarged lymph nodes, red stripes, painful palpation and the appearance of a body temperature of up to 38 degrees. Acute pain in the direction of the affected vein is often observed. It is recommended to start treatment in time, this will prevent the development of complications.
First signs
Thrombophlebitis of the upper extremities can develop due to an unsuccessful injection and even after an insect bite. In this case, the affected vein is very translucent and has a purple hue. This indicates its inflammation. It is painful and dense to the touch, because a so-called cord is formed there. Thus, the first signs begin to manifest themselves immediately. Sometimes the process has a rapid and unexpected course. Acute pain appears lightning fast.
The body temperature begins to gradually increase, but in some cases this symptom is absent. It is quite easy to notice an inflamed vein, it immediately begins to bother a person. Over time, the limb can swell due to impaired blood circulation. If you do not pay attention to this, there is a limitation of movement. If the vein becomes painful or red, you should go to the hospital. If deep veins are affected, there is a risk of developing serious complications.
Thrombophlebitis of the superficial veins of the upper extremities
The most typical signs of this disease are general inflammatory reactions, pain and swelling. Often, thrombophlebitis of the superficial veins contributes to the development of lymphadenitis in the upper limbs. Everything is accompanied by pronounced hyperemia and the presence of infiltrates along the thrombosed veins. The patient is bothered by elevated body temperature, in some cases its indicator is 39 degrees.
The limb does not change in size, but swells a little. Movements in the joints are free, but can be painful. The whole point is that there are zones of inflammation. At the site of thrombus formation, a painful infiltrate can be felt, which has clear boundaries. The lymphatic system does not participate in the inflammatory process, but only at the initial stage. When the thrombosed vein begins to suppurate, lymphadenitis is observed.
Sometimes the symptoms can manifest themselves abruptly. This indicates the presence of an acute form of the disease. The person feels severe pain. Within a few days, relief occurs, but the pain still remains when palpated.
If symptoms appear, you should seek help from a doctor. High-quality differential diagnostics will allow you to make the correct diagnosis. This, in turn, will affect the effectiveness of the prescribed treatment.
Deep vein thrombophlebitis of the upper extremities
Deep vein thrombosis usually occurs after intravenous administration of drugs that can cause irritation. Often, deep vein thrombophlebitis affecting the upper extremities is caused by an insect bite or local injury. Infiltration and hyperemia are observed along the vein. This process is visually similar to a crimson stripe, which is located at the site of the inflammatory process. Painful palpation and the presence of dense nodules are also noted here. There is a so-called cord, represented by a seal on the affected area.
If the lesion covers the cubital veins or vessels on the wrist, the mobility of the joints is impaired due to the presence of sharp pain. In addition, the process is accompanied by an increase in temperature. If adequate therapy is prescribed, thrombophlebitis will begin to recede after 12 days. During treatment, inflammatory phenomena gradually subside and the vein is restored.
Consequences
If the treatment was chosen correctly, then a positive result can be observed in a few days. Moreover, the inflammatory process gradually subsides and the vein begins to recover. All this is possible with timely treatment at the hospital and the appointment of high-quality therapy. In this case, the consequences cannot develop, because everything is under control. But not always everything goes so easily. Sometimes people do not pay attention to serious symptoms and do not begin treatment. This is fraught with not only the formation of a thrombus, but also its detachment.
In order to exclude possible complications, it is necessary to be observed by a phlebologist for a year after successful treatment. It is necessary to monitor the condition of the venous system and the affected limb itself. If surgery was performed, you will also have to visit a surgeon.
Correctly selected treatment will allow achieving maximum vein patency, which will lead to improved venous outflow. Despite this, the risk of developing post-thrombotic disease still remains. It can manifest itself after two to three years. In this case, a comprehensive study of the veins is carried out. If there is an urgent need, a surgical operation is performed.
 [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ]
[ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ]
Complications
The danger of the disease lies in the location of the inflammatory process and the thrombus itself. Superficial veins suffer much more often, because thrombophlebitis is a complication of varicose veins. This process does not pose a serious danger to human health. Everything is eliminated by medication and compression therapy.
More dangerous is thrombophlebitis, which can result in death. This probability remains when deep veins are affected. There are also a number of other serious complications. There is a risk of developing venous gangrene, which occurs due to the cessation of blood flow to the limb. This condition threatens complete amputation. Thrombophlebitis can lead to pulmonary embolism. This condition is characterized by the separation of a thrombus from the vessel wall and its movement into the pulmonary artery. Immediate surgical intervention is necessary here. Timely detection of venous diseases will help avoid all possible complications, including thrombophlebitis.
Diagnosis of thrombophlebitis of the upper extremities
Diagnostic measures are simple, thanks to them it is possible to determine the presence of the disease without any difficulties. Instrumental methods of diagnosing thrombophlebitis of the upper extremities are widely used. These include rheovasography or ultrasound Dopplerography. It is possible to obtain accurate information thanks to ultrasound duplex angioscanning. This process is characterized by color coding of blood flow.
Angioscanning allows one to assess the condition of the walls and lumen of the veins. Determine the presence of thrombotic masses in them, as well as the nature of the thrombus that has formed. In some cases, it is possible to roughly judge the "age" of the thrombus and the degree of its organization. Ultrasound scanning of the subcutaneous veins allows one to determine the extent of the thrombus.
Laboratory diagnostics do not play a special role. After all, it allows us to identify the presence of an inflammatory process, but does not record in which organ or system it arose.
Tests
Laboratory diagnostics are not as significant as instrumental examination. Previously, there were assumptions that changes in homeostasis may indicate the presence of a thrombus formation process, its attenuation or activity. However, coagulation tests have not proven their significance. These analyses do not provide complete information about the probability of thrombosis and its active development.
Previously, it was believed that an increase in the thrombosis index indicates the formation of a thrombus in the vein. This approach cannot provide accurate information, and therefore had to remain in the past. Today, there are sensitive markers of thrombus formation. But even their use does not allow us to determine the level of thrombophlebitis, or assess the likelihood of pulmonary embolism.
Clinical tests show only superficial signs of the inflammatory process. Increased white blood cell count, increased ESR, and a positive reaction to C-reactive protein. But they do not indicate where exactly the inflammatory process is developing. Therefore, they do not play a special role in diagnosing thrombophlebitis.
 [ 19 ], [ 20 ], [ 21 ], [ 22 ]
[ 19 ], [ 20 ], [ 21 ], [ 22 ]
Instrumental diagnostics
Many methods are used to diagnose the inflammatory process. One of them is ultrasound angiography of the extremities. This method of instrumental diagnostics is based on the ability of tissues to absorb and reflect ultrasound waves. To conduct the examination, it is therefore necessary to make a color mapping of the blood flow. The main disadvantage of the method is its strong dependence on the technical characteristics of the devices, as well as the qualifications of the person conducting the study.
- Ultrasound Dopplerography. This method will determine the direction and speed of blood flow in different areas of the vessel. This method is great for obtaining the general state of the functioning of the circulatory system. However, it does not provide data on the structure and anatomy of the veins.
- Phleboscintigraphy. To conduct the study, a special preparation containing a radioactive isotope with a short half-life must be injected into the vein. Then, the contrast agent is distributed throughout the system using a special device.
- Phlebography. This method evaluates the condition of the veins using a special contrast agent based on iodine. Finally, magnetic resonance imaging. It is one of the modern methods of research, but also the most expensive. Thanks to this method, you can get the most accurate results. The procedure is prescribed if all previous methods did not provide complete information about the person's condition.
Differential diagnostics
In addition to instrumental examination, laboratory tests are also carried out. However, they are not of particular importance. Thus, differential diagnostics is the delivery of blood tests. This concept is characteristic only for thrombophlebitis. In general, this method of research includes a lot of other tests.
An increased number of leukocytes can be detected in the blood, which indicates the presence of an inflammatory process. This can be indicated by a change in the ESR indicator, as well as increased blood clotting activity. Sensitive markers of thrombus formation play an important role. These include: thrombin-antithrombin complex, fibrinopeptide A, soluble fibrin-monomer complexes, and the level of D-dimer in plasma. However, their use will not allow determining the level of thrombus formation, as well as the likelihood of pulmonary embolism. Therefore, it is most advisable to conduct not only differential research methods, but also instrumental ones. Based on the data obtained, they are compared and a diagnosis is made.
Who to contact?
Treatment of thrombophlebitis of the upper extremities
Conservative treatment for thrombophlebitis is possible, but only if the affected area is small. When deep veins are affected, surgical intervention is used. Drug treatment for thrombophlebitis of the upper extremities is aimed at preventing possible complications, as well as preventing the development of a thrombus.
To eliminate inflammatory processes, they resort to the help of such drugs as Ibuprofen, Diclofenac and Aspirin. They can eliminate not only the inflammatory process, but also reduce swelling and relieve pain. Direct anticoagulants, which improve blood flow, are also widely used, including Heparin, Enoxaparin and Fraxiparin. They are prescribed if there is a risk of thrombophlebitis spreading to deep veins. They can also resort to the help of thrombolytics, such as Streptokinase and Alteplase. Heparin ointment, Ketoprofen gel and Troxevasin are used locally.
The person must stay in bed. The affected limbs must be elevated, this will normalize blood flow and reduce the risk of thromboembolism. The entire course of treatment should be carried out under the supervision of a specialist.
Medicines
Drug therapy is effective if the superficial veins are affected. It is aimed at reducing swelling, pain and restoring blood flow. To eliminate the inflammatory process and reduce pain, anti-inflammatory drugs such as Ibuprofen, Diclofenac and Aspirin are taken. To improve blood flow, Heparin, Enoxaparin and Fraxiparin are prescribed. Thrombolytics such as Enoxaparin and Fraxiparin are also widely used. Ointments and gels are also used: Heparin ointment, Ketoprofen gel and Troxevasin.
- Ibuprofen. The drug is used one tablet 2-3 times a day. Depending on the patient's condition, the dose can be adjusted. Patients with hypersensitivity, as well as severe liver and kidney dysfunction should not take the drug. During pregnancy and breastfeeding, taking is prohibited, but can be agreed with the attending physician. Can cause nausea, vomiting, diarrhea and allergic reactions.
- Diclofenac. The drug is used one tablet up to 4 times a day. Its active ingredient is diclofenac, so it cannot be used by people with increased sensitivity to it. The risk group includes pregnant girls, children and people with impaired liver and kidney function. The drug can cause allergic reactions in the body.
- Aspirin. The drug is used one capsule at a time, no more than 3 times a day. The exact dose is prescribed by the attending physician. The drug cannot be used by children, pregnant women, people with hypersensitivity, as well as those who have severe liver and kidney failure. It can lead to the development of allergic reactions in the body.
- Heparin. The dosage and method of administration are prescribed by the doctor on an individual basis. The drug should not be used in case of increased bleeding, bleeding of any localization, acute cardiac aneurysm, liver and kidney failure. May cause allergic reactions in the body.
- Enoxaparin. The drug is administered exclusively in the supine position, only subcutaneously in the anterior or posterolateral region. The average dosage is 20 mg per day, it can be adjusted by the attending physician. People with severe liver and kidney failure, as well as in the presence of hypersensitivity, should not take the drug. It can cause hemorrhagic manifestations.
- Fraxiparin. The dose is prescribed strictly on an individual basis. The drug cannot be used in case of gastric ulcer and duodenal ulcer, as well as acute infective endocarditis. May cause small hematomas and increased liver enzyme levels.
- Heparin ointment. Apply a thin layer of the product to the affected area. It can be used up to 4 times a day, depending on the severity of the situation. Do not apply the ointment to open wounds or to damaged skin. It can cause local allergic reactions such as itching, burning, redness, and swelling.
- Ketoprofen. The gel is applied in a thin layer to the affected area, 3-4 times a day. It cannot be used by people with increased sensitivity of the skin. It can lead to the development of allergic reactions.
- Troxevasin. The gel is applied in a thin layer, with light massaging movements 3 times a day. It cannot be used if the integrity of the skin is compromised. It can lead to the development of an allergic reaction, causing itching, burning and redness.
Folk remedies
Traditional medicine is rich in its effective recipes. In some cases, it is not worth resorting to traditional treatment. After all, if you want to eliminate thrombophlebitis, without special knowledge, you can cause serious harm to the body.
- Recipe #1. Take 15 grams of verbena leaves and pour a glass of boiling water over them. Then let it brew for a bit and take a tablespoon. Effectively helps with vein blockage.
- Recipe No. 2. To relieve inflammation and eliminate swelling, fresh lilac leaves can be applied to the limbs.
- Recipe #3. Take 20 grams of St. John's wort, string and licorice root. For effectiveness, add 15 grams of plantain and coriander leaves, dilute everything with 10 grams of immortelle. Mix all the ingredients together. Take only 2 tablespoons and pour boiling water over them. Heat the product in a water bath for 15 minutes. Then cool, strain and bring to a volume of 200 ml. Take 30 minutes before meals.
 [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ]
[ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ]
Herbal treatment
In folk medicine, there are many effective recipes using herbs. They help not only cope with the main symptoms of the disease, but also significantly improve the patient's condition. In general, herbal treatment has a positive effect, but only if all the recipes are approved by a doctor.
Silver wormwood has excellent properties. It is necessary to take fresh wormwood leaves and grind them thoroughly in a mortar. Then take a tablespoon of the resulting powder and combine it with sour milk. After that, everything is thoroughly mixed and applied to gauze. The resulting compress should be applied to the affected veins. The duration of treatment is 3-4 days.
Hops are quite helpful in dealing with the symptoms of thrombophlebitis. Take one tablespoon of hop cones and chop them finely. Then pour a glass of boiling water and heat in a water bath for 15 minutes. The resulting remedy is taken one glass 3 times a day before meals.
Horse chestnut should also be taken into account. You need to take 50 grams of the main ingredient and pour 500 ml of vodka over it. After that, it should be placed in a warm place for 2 weeks. After the specified period, the remedy is used 30-40 drops for a month.
Homeopathy
Homeopathic remedies have always been particularly popular. This is due to their natural composition, which does not contain any substances dangerous to the body. However, due to the fact that the drugs have not undergone clinical trials, their use can harm a person. Therefore, homeopathy is used if the doctor himself has prescribed this method of treatment.
To eliminate varicose veins and thrombophlebitis, the drug Iov-Venum is widely used. The drug should be taken for several months. The primary effect can be seen in the 3rd week of administration. In some cases, the drug can cause an increase in symptoms or a deterioration in the patient's condition. There is no need to be afraid of this, this process indicates that the healing processes in the body are beginning to actively proceed. If negative symptoms appear, you should stop taking the drug for a week, then continue taking it. 8-10 drops 2 times a day for 5-6 days are enough. The dose and regimen are prescribed by a doctor. You can learn about other drugs at an appointment with an experienced homeopathic doctor.
Surgical treatment
Patients with ascending thrombophlebitis or deep vein disease require surgical intervention. The decision on surgical treatment should be made by the attending physician. Such a verdict is made after conducting an ultrasound scan.
Depending on the severity of the disease, as well as its features, the doctor must decide on surgical intervention or a minimally invasive method of removing the thrombus. Surgical methods allow sclerosis or complete removal of the affected veins as the disease progresses. The minimally invasive method can be combined with conservative treatment. It allows you to remove the formed thrombus. This technique is less traumatic and practically does not cause any complications. Therefore, it is quite safe to resort to this method of removing the affected vein. This procedure is used even during pregnancy.
Prevention
Preventive measures are determined by timely treatment. Patients with varicose veins should undergo immediate surgical treatment. The main task of prevention during the prevention of thrombus detachment and its migration is the installation of a special trap. It must be installed in the vein. There it opens up and lets only blood through, and large thrombi remain in it. The method is effective, but has many disadvantages.
Thrombectomy will remove the thrombus without consequences. True, this method requires high surgical skills. The procedure allows you to remove the thrombus directly from the vein. In addition, it improves the long-term results of treating deep vein thrombosis. The effectiveness of the technique is that after its use, the development of post-thrombotic disease is not observed. Timely treatment will really help to cope with the problem. Moreover, timely elimination of varicose veins is the main preventive measure that will not allow thrombophlebitis to develop.
Forecast
Thrombophlebitis is a very dangerous disease. However, despite this, it is very treatable. If the treatment was started on time, the prognosis will be positive.
After surgery or conservative therapy, blood flow is normalized. But despite this, patients should still use compression hosiery and take medications prescribed by the attending physician. This will help avoid possible complications.
Treatment that was not started in time can lead to the development of ulcers, gangrene, and thrombosis of large veins. In this case, the prognosis becomes unfavorable. After the complications are eliminated, a person can return to work, of course, if his limb was not removed due to the development of gangrene. The quality of life of patients is significantly reduced. The prognosis depends entirely on the form of the disease, as well as the affected veins.

