Medical expert of the article
New publications
Testicular MRI
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Testicular MRI (testicular magnetic resonance imaging) is a medical procedure that uses magnetic fields and radio waves to create detailed images of the testicles and surrounding tissues within the male pelvic region. Testicular MRI has become a valuable adjunctive method of examining testicular pathology. [1], [2], [3] It is a non-harmful and non-invasive study that can aid in the diagnosis and evaluation of various conditions and diseases of the testicles and surrounding structures.
MRI of the testicles may be performed for a variety of reasons:
- Diagnosis of testicular diseases and injuries: MRI helps to detect the presence of tumors, cysts, inflammation, trauma and other testicular abnormalities.
- Investigation of testicular pain and discomfort: If a patient is experiencing pain or discomfort in or near the testicles, an MRI may help determine the cause of these symptoms.
- Evaluation of pathology of the scrotum and surrounding structures: MRI may also be useful to evaluate the scrotum and vessels that run through the pelvic region.
The testicular MRI procedure is performed using a specialized machine called an MRI scanner and may require the administration of a contrast agent to improve the quality of the images. It is important to note that before undergoing an MRI, the doctor may recommend that the patient follow certain instructions, including restricting food and fluid intake in some cases. [4]
Testicular MRI is an important diagnostic modality that helps physicians identify and evaluate a variety of testicular and male reproductive conditions and pathologies. MRI findings can narrow the differential diagnosis, helping to plan a more accurate treatment strategy and reducing the need for unnecessary surgical exploration. [5], [6]
Indications for the procedure
MRI (magnetic resonance imaging) of the testicles may be ordered for a variety of medical conditions, including:
- Pain and discomfort in the testicles or scrotum: If a patient experiences pain, discomfort, or swelling in the testicular area, an MRI may help identify the cause of these symptoms, such as inflammation, injury, or tumor.
- Testicular incontinence (testicular incontinence): MRI can be used to assess the position of the testicle in the scrotum, especially in children or in patients with developmental abnormalities.
- Diagnosis of testicular tumors and cysts: MRI can determine the size, location, and nature of tumors, cysts, and other masses in the testicles.
- Infertility and reproductive health: MRI can be used to evaluate the testicles and surrounding structures in patients with fertility problems and reproductive disorders.
- Follow-up after surgical procedures: MRI can be used to evaluate the results of testicular or scrotal surgery.
- Evaluation of trauma and traumatic injuries: MRI may be ordered after testicular trauma to determine the nature and extent of the injury.
- Vascular and bleeding studies: MRI can help visualize the vessels that run through the pelvic region and determine if there are bleeding or other vascular problems.
These are just a few common indications for testicular MRI. The ultimate decision to order an MRI is made by the physician based on the clinical findings and symptoms of each patient.
Preparation
Preparation for MRI (magnetic resonance imaging) of the testicles is usually minimal and does not require major measures. Here are some general guidelines for preparing for testicular MRI:
-
Clothing: Come in comfortable clothing without metal items such as zippers, buttons, or metal rivets. Metal objects can distort the image during the MRI.
- Removal of metal objects: You may need to remove jewelry, glasses, dental braces, removable dentures, and other metal objects that may interfere with the procedure.
- Food and Fluids: In most cases, there are no specific fasting requirements for testicular MRI. You can eat and drink as usual before the procedure.
- Medications: If you are taking any medications, continue taking them on your regular schedule unless your doctor has given other instructions.
- Consultation with your doctor: If you have any medical contraindications or allergies, be sure to discuss this with your doctor and the MRI technician before the procedure.
- Special Cases: In rare cases, your doctor may require special preparations, such as injecting a contrast agent into a vein. In such cases, your doctor and medical staff will provide you with additional instructions.
The device for carrying out the procedure
Magnetic resonance imaging (MRI) of the testicles is performed using a specialized MRI machine. Testicular MRI uses MRI machines of strong magnetic fields and radiofrequency pulses to create detailed images of the internal structures of the testicles and surrounding tissues. The MRI machine for this procedure usually consists of the following components:
- Magnet: This is a strong magnetic field created inside the MRI machine. The patient will be inside this magnet during the procedure.
- Radiofrequency coils: These coils are placed around the patient's body and are used to transmit radiofrequency pulses and record the signals that occur in response to the magnetic field.
- Computer and software: The signals received are processed by a computer that creates images of internal structures.
The testicular MRI procedure is usually performed in a specialized MRI department or center that has the appropriate equipment and experienced medical staff. During the procedure, the patient will lie on a table that moves inside the magnetic machine. It is important to follow the instructions of the medical staff and remain still during the procedure to get quality images.
Testicular MRI may be ordered by a doctor to diagnose various conditions such as tumors, inflammation or other pathologies and is usually performed without the use of contrast agents.
Technique of the testicular MRI
Here is the general technique for performing a testicular MRI:
- Preparation: In most cases, no special preparation is required before a testicular MRI. However, your doctor may require you to follow certain recommendations, such as not eating for several hours before the procedure, especially if you will be given an intravenous contrast agent.
- Positioning: The patient lies down on the MRI table, which will move around inside the MRI machine. It is important to remain still during the procedure to avoid blurring of the images.
- Injection of contrast agent (as needed): Sometimes it may be necessary to inject a contrast agent into a vein for better visualization of certain structures. This can be particularly useful when evaluating blood vessels or certain pathologies.
- Scanning: The procedure begins by turning on the magnetic field and sending radio waves inside the body. As the table moves inside the CT scanner, a series of images of the testicles and surrounding tissues are created. The doctor or radiologist controls the process of extracting the images to get the data you need.
- Completion of the procedure: After the scan is completed, the patient may be asked to remain lying down for some more time to process the data and make sure there is no discomfort.
- Results and interpretation: The findings are analyzed by a physician or radiologist who evaluates the condition of the testicles and surrounding structures and makes an appropriate diagnosis.
A testicular MRI is a safe procedure that is usually not accompanied by much discomfort. After the procedure, the patient can return to daily activities.
Contraindications to the procedure
MRI (magnetic resonance imaging) of the testicles is generally a safe and minimally invasive procedure, and contraindications to testicular MRI are quite rare. However, there are some circumstances in which MRI may be limited or require additional precautions:
- Presence of metal implants or metal internal devices: The presence of metal objects in the patient's body, such as stents, pacemakers, orthopedic implants, etc., may cause interference with MRI. Patients with such devices may require other diagnostic techniques.
- Pregnancy: MRI may be limited in the first trimester of pregnancy due to potential fetal exposure to magnetic fields and radio waves. However, in the second and third trimesters, MRI may be performed for acute medical indications when the benefits outweigh the potential risks.
- Claustrophobia: People who suffer from claustrophobia (fear of confined spaces) may experience discomfort or anxiety inside the MRI scanner. In such cases, additional measures may be required to ensure patient comfort.
- Allergic reaction to contrast agent: In rare cases, the contrast agent used to enhance MRI images may cause an allergic reaction. Patients with known allergies to components of the contrast agent should inform their physician.
- Age: In infants and young children, MRI scans may require general anesthesia, and physicians should evaluate the indications and risks in such cases.
Patients should always discuss their medical and anamnestic information in detail with their doctor before undergoing an MRI to ensure that the study is safe and appropriate for their situation. Physicians will evaluate the patient and consider all risk factors and contraindications before scheduling an MRI.
Normal performance
Normal findings on testicular MRI may include the following characteristics:
- Size and shape: The testicles are usually oval in shape and symmetrical in size. The normal size of the testicles can vary depending on age and other factors, but they are usually about 4-5 centimeters long, 3 centimeters wide, and 2 centimeters thick.
- Consistency: On MRI, testicles usually have a uniform texture and density.
- Vascularity: MRI may allow visualization of the vessels in the testicular area. Normal vessels allow normal blood flow and supply of oxygen and nutrients to the testicles.
- No tumors: MRI can be used to detect the presence of tumors, cysts, masses, or other abnormalities in the testicular area. Normal testicles usually have no visible tumors or masses.
- No signs of inflammation: MRI can also help rule out signs of inflammatory processes such as acute or chronic epididymitis.
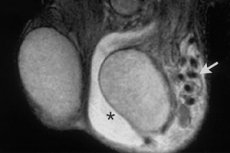
Normal testes appear as well-defined, homogeneous structures with a T1 signal similar to that of skeletal muscle and a high T2 signal. [7], [8] The internal architecture of the testis is clearly visible on T2-weighted images. The white coat is visible around the testis as a thin hypointense rim on both T1 and T2 pulse sequences, better defined on T2-weighted images. Thin septa with low T2 signal are usually seen passing through the testicular parenchyma to the testicular mediastinum, which is detected as an area of low signal intensity in the posterior parts of the testis.

Normal testes have high and slightly low signal on DWI maps with high b value and apparent diffusion coefficient (ADC), respectively, due to the histologic complexity of the normal parenchyma. [9], [10] Normal testicular parenchyma is moderately and homogeneously enlarged. [11], [12]
The testicular appendage is slightly heterogeneous, with a T1 signal similar to that of the testis. It has a lower signal intensity than the adjacent testicular parenchyma on T2-weighted imaging. The scrotal wall typically has low signal intensity in both pulse sequences. The seminal tubules are revealed predominantly hyperintense due to the presence of fat, with hypointense vessels running through them, better visualized on coronal T2-weighted imaging. A frequent small hydrocele is normal. [14]
It is important to note that interpretation of MRI images and establishment of normal values should always be performed by a qualified radiologist or MRI technician. Results and norms may vary depending on the medical facility, equipment used, and individual patient characteristics.
Complications after the procedure
Magnetic resonance imaging (MRI) of the testicles is generally considered a relatively safe procedure, and complications from it are rare. However, some complications can occur:
- Allergic Reactions: If a contrast agent is used during an MRI (rarely required for testicular MRI), some patients may have an allergic reaction to the agent. Symptoms of allergy may include itching, skin rashes, difficulty breathing, or anaphylaxis. This is a rare but serious complication.
- Discomfort and Anxiety: Some patients may experience discomfort or anxiety during the procedure due to the limited space inside the MRI machine and the length of the procedure (usually 30-60 minutes). It is important to let the medical staff know if you feel discomfort so they can provide support and comfort.
- Claustrophobia: People who suffer from claustrophobia (fear of confined spaces) may experience stress and anxiety during an MRI because of the need to lie inside the narrow MRI tube.
- Incorrect diagnostic imaging: In some cases, if the patient is unable to remain still during the MRI scan, this can distort the images and reduce the quality of the diagnosis.
Be sure to tell the medical staff about all of your allergies, medical conditions and fears prior to your MRI. This will help them take precautions and ensure that the procedure is performed safely. If you experience any unusual symptoms after your MRI, contact a medical professional for further consultation and evaluation.
Care after the procedure
No special care is usually required after a testicular MRI procedure because it is minimally invasive and safe. However, you may be given the following general recommendations:
- Return to normal activities: After a testicular MRI, you can immediately return to your normal activities, including driving, work, and physical activity. The procedure does not require a separate recovery time.
- Nutrition and hydration: The MRI procedure is not usually associated with food or fluid restriction. You can naturally continue to eat food and drink water after the scan.
- Continuing Treatment: If you are prescribed any treatment or therapy based on your MRI results, be sure to follow your doctor's instructions. You may be prescribed medications or other medical procedures.
- Maintain a healthy lifestyle: Maintain a healthy lifestyle, including eating right, being physically active, and following testicular and men's health care guidelines.
- Increasing your comfort: If you experience any temporary discomfort after your MRI (e.g., mild dizziness due to contrast agent treatment), just give yourself time to recover. If the condition does not improve or worsens, contact your doctor.
- Following recommendations: If your doctor has given you any specific instructions or recommendations, be sure to follow them. This may include scheduling additional tests, counseling, or treatment.
A list of authoritative books and studies related to the study of testicular MRI
Books:
- "MRI of the Male Pelvis" (Author: Jean-Nicolas Dacher, 2010) - This book covers various aspects of MRI of the male pelvis, including testicular MRI, and methods for diagnosing various pathologies.
- "MRI and CT of the Female Pelvis" (Author: R. Brooke Jeffrey, 2017) - Although the book focuses on the female pelvis, it also includes information on MRI of the male pelvis and may be useful for a general understanding of MRI techniques.
Research and articles:
- "MRI of the scrotum: Recommendations of the ESUR Scrotal and Penile Imaging Working Group" (authors: Authors' Collective, 2016) - Recommendations and review of MRI techniques for examining the seminal canal and testicles.
- "MRI of the scrotum" (authors: G. Poznikhov, P. Kirsner, 2014) - An article discussing MRI and its application in the study of the male genital organs, including the testicles.
- "MRI of testicular and scrotal disorders" (Author: Chia-Hung Kao, 2013) - A review of MRI in the diagnosis of various testicular and seminal tubal disorders.
Literature
- Fundamentals of Radiation Diagnosis and Therapy. National Manual on Radiation Diagnostics and Therapy. Edited by S.K. Ternovoy, GEOTAR-Media, 2013.
- Lopatkin, N. A. Urology: National Guide. Brief edition / Edited by N. A. Lopatkin - Moscow: GEOTAR-Media, 2013.

