Medical expert of the article
New publications
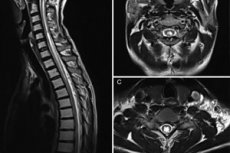
Syringomyelia of the cervical and thoracic spine
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Translated from Greek, the term "syringomyelia" literally means "emptiness in the spinal cord." The pathology is a chronic disorder of the central nervous system, characterized by the formation of fluid-filled cavities in the spinal cord. Less often, the disease affects the medulla oblongata.
Syringomyelia is caused by damage to glial tissue, or is the result of malformations of the craniovertebral junction. The disease is one of a number of incurable pathologies, diagnosed using magnetic resonance imaging. [ 1 ]
Epidemiology
Syringomyelia is classified as a chronic progressive pathology of the nervous system. This disorder is characterized by the formation of peculiar cavities in the spinal cord (usually in the lower cervical or upper thoracic segment), which entails the loss of certain types of sensitivity in the corresponding zones. The problem can also spread to the medulla oblongata. If the pons is involved in the process, the patient is diagnosed with syringobulbia. Lesions of the lumbar region, as well as complete lesions of the spinal column, are extremely rare.
Syringomyelia affects mostly men (approximately 2:1). Clinical symptoms are usually detected at a young age (around 25 years), less often at 35-40 years.
More than half of cases of the disease are associated with Arnold-Chiari syndrome. [ 2 ], [ 3 ]
True syringomyelia is usually accompanied by congenital deformities and developmental defects of the spinal column, such as curvatures, abnormal chest configuration, malocclusion, asymmetry of the facial part of the skull and other skeletal segments, ear dysplasia, bifurcation of the tongue, extra fingers or nipples of the mammary glands, etc. The true form of the disease occurs in more than 30% of cases and is familial, and is diagnosed mainly in males. In all other cases, syringomyelia is associated with defects of the craniovertebral junction, which entail widening of the spinal canal. In the area of maximum expansion, the gray matter is destroyed, which causes the characteristic symptoms. Less common causes are spinal injuries, hemorrhages, and spinal cord infarction.
The prevalence of syringomyelia is approximately 3 cases per hundred thousand people. Some studies have shown that the prevalence of syringomyelia ranges from 8.4 per 100,000 to 0.9 per 10,000, taking into account ethnic and geographic differences. [ 4 ], [ 5 ] In approximately 75% of cases, limitation or loss of ability to work occurs in young and middle age (20-45 years). [ 6 ]
Causes syringomyelia
Syringomyelia can be congenital or acquired:
- The congenital form is a consequence of the abnormal development of the spinal column and spinal cord during the embryonic period. Glial cells, designed to protect the nerve structures, mature too slowly, and some of them continue to grow after the formation of the central nervous system is complete.
- The acquired form is the result of tumor processes, spasms, traumatic injuries to the spine, and acute infectious and inflammatory diseases.
Any of the above forms is accompanied by the formation of an excessive number of additional neuroglia. Against the background of their constant dying off, cavities with an internal lining of glial tissue are formed. Liquid easily penetrates through such a barrier, so the cavities quickly fill with cerebrospinal fluid: cystic elements are formed, which gradually increase. The next stage is an increase in pressure on nearby structures, which leads to pain syndrome, loss of various types of sensitivity in the limbs and body. [ 7 ]
The main causes of this pathology are considered to be the following:
- congenital anomalies of the central nervous system;
- tumors with spread to the spinal cord structures and lower part of the brain;
- traumatic injuries and developmental anomalies of the spinal column;
- pathological narrowing of the spinal canal;
- damage to the transition zone of the base of the skull to the spinal column;
- excessive physical exertion.
Today, experts continue to study risk factors that can lead to the development of syringomyelia.
Risk factors
Among the factors contributing to the development of syringomyelia, the most significant role is played by:
- acute and chronic infectious and inflammatory pathologies of the respiratory system;
- heavy physical exertion;
- injuries, inflammatory and tumor processes affecting the spinal column; [ 8 ]
- unsatisfactory professional and living conditions.
Additional factors include:
- Smoking significantly increases the risk of problems with the spinal column, as it contributes to a decrease in the level of oxygen in the blood, which leads to the appearance of trophic disorders in the tissues.
- Excess weight puts additional strain on the spine. Sometimes, the symptoms of the disease can be alleviated only by eliminating the extra pounds.
- Too tall (for men – over 180 cm, for women – over 175 cm).
Pathogenesis
Syringomyelia develops as a result of a disorder occurring in the spinal cord structures. Microscopic cystic areas form in the spinal cord of patients. Connective tissue grows around them (instead of nerve tissue), which leads to compression and disruption of the sensory channels through which pain and temperature sensation are transmitted. [ 9 ]
Even with a congenital etiology of the disease, the appearance and further development of pathological changes in the spinal cord are caused mainly by external stimuli. External influences contribute to the manifestation of an internal disorder, which entails the development of syringomyelia. [ 10 ]
Scientists have noted that the majority of patients develop the disease in people who systematically experience heavy physical exertion. This was confirmed by the fact that the introduction of mechanization of labor in production led to a decrease in the incidence of syringomyelia. [ 11 ]
Currently, the following factors are increasingly noted as the cause of the disease in patients diagnosed with syringomyelia:
- past trauma, back bruises;
- hypothermia, prolonged exposure to cold conditions;
- smoking, alcohol abuse;
- lack of attention to one's own health, ignoring the first signs of pathology, self-medication, untimely visit to the doctor.
In medicine, the following types of disease pathogenesis are distinguished:
- disruption of cerebrospinal fluid circulation in the area of the posterior cranial fossa and spinal cord, which occurred as a result of a failure at the embryonic stage of development;
- incorrect closure of the medullary tube with the formation of a posterior suture, which occurs as a result of bone defects and gliomatosis with subsequent decay and the formation of cystic and fissure changes.
Genetic-constitutional disorders are detected in the form of specific dysraphic features that are transmitted in an autosomal dominant manner and represent a predisposition to pathology. Defects in the formation of the medullary tube and craniovertebral junction provide only favorable conditions for the development of pathology. [ 12 ]
Pathogenetic role is played by injuries of the spine and spinal cord, physical microtraumas. The problem most often affects the cervical and upper thoracic region of the spinal cord, less often - the lower thoracic and lumbosacral region. [ 13 ]
In some patients, the pathological process spreads to the medulla oblongata (in the form of syringobulbia), less often to the pons and internal capsule. [ 14 ]
Symptoms syringomyelia
In most patients suffering from syringomyelia, the cavitary areas are formed in the area of the posterior horns of the spinal cord. This is where the sensitive nerve cells responsible for pain and temperature sensations are located. On the skin of a sick person, entire zones can be identified where sensitivity is not determined. Most often, they are found on the arms and body - like a "half-jacket" and "jacket", which corresponds to unilateral and bilateral damage.
Read more about the symptoms and types of syringomyelia here.
Complications and consequences
Complications of syringomyelia may include:
- muscle atrophy, contractures;
- secondary infection, development of pneumonia, bronchopneumonia, cystitis, pyelonephritis;
- infection entering wounds and damage to the skin, development of purulent processes, up to septic complications;
- development of bulbar paralysis, which may result in respiratory failure and death of the patient.
Experts note that syringomyelia most often takes a sluggish nature and rarely leads to the development of severe conditions. An exception is the aggressive progressive form of the disease, in which the formation of spinal cavities continues. Such a pathology already poses a danger not only to the health, but also to the life of the patient: urgent surgical treatment is required.
In general, the course of syringomyelia is difficult to predict: the disease occurs with alternating periods of stable and progressive dynamics. Progression can be observed over a period of several weeks to several years, with sharp deteriorations and equally sharp slowdowns in development. Under the influence of provoking factors (severe cough, intense head movement, etc.), an acute clinical picture can develop in a previously asymptomatic patient.
The quality of life of patients is comparable to that of people suffering from heart failure or malignant tumor processes.
Possible postoperative complications include:
- cerebrospinal fluid leakage (liquorrhea);
- pseudomeningocele;
- shunt displacement;
- transient neurological deficiency.
The incidence of such complications after surgery is relatively low.
The main consequence of syringomyelia is myelopathy, which can progress to paraplegia and tetraplegia, cause spasms, the formation of bedsores, ulcers, relapses of pneumonia, and also lead to disturbances of intestinal and genitourinary functions. [ 15 ]
Diagnostics syringomyelia
Diagnostic measures begin with questioning the patient. It is important for the doctor to pay attention to signs that characterize such symptomatic groups as spinal cord damage and craniovertebral pathology. Suspicious signs are:
- sensory disturbances (paresthesia, pain, analgesia, dysesthesia, decreased temperature sensations);
- aching pain in the arms, neck, back of the head, chest;
- a feeling of cold or chilliness in some areas, numbness;
- persistent headaches, otoneurological and visual disorders (eye pain, photophobia, diplopia, loss of visual acuity, dizziness, vestibular disorders, pressure and noise in the ears, hearing loss, vertigo).
During the survey, it is necessary to clarify with the patient about the hereditary factor, previous pathologies and injuries, and the degree of physical activity. Since the acute onset of syringomyelia is very rare, and the disease is predominantly of a sluggish, protracted nature, it is necessary to try to determine the approximate period of the onset of the disorder.
When examining a patient, it is necessary to pay attention to the presence of a typical clinical picture of syringomyelia: paresis, sensitivity disorders, vegetative-trophic changes.
Laboratory tests are non-specific and are prescribed as part of general clinical studies:
- general blood and urine analysis;
- biochemical blood test.
Instrumental diagnostics is primarily represented by MRI. This procedure allows us to evaluate the parameters of cystic formations, describe their size and configuration. It is optimal to use a sagittal projection in T1 mode, which is due to its lower sensitivity to fluid movement. Typical MRI signs of syringomyelia are as follows:
- spinal cord signal change, such as a longitudinal, central or paracentral region, the intensity of which is similar to that of the cerebrospinal fluid;
- the transverse volume of the spinal cord may be increased;
- the most common location of the pathological cavity is the cervicothoracic region;
- the distribution of the cavity is from 2 segments to the entire length of the spinal cord;
- cavity diameter – 2-23 mm;
- when the cavity size is more than 8 mm, spinal cord enlargement is observed.
It is recommended to perform MRI along the entire length of the spinal column.
The cavity shapes are of the following types:
- symmetrical, centrally located, round-oval;
- irregular in shape, localized in the central or paracentral spinal cord areas.
The second type of cavity, located in the area between the anterior and posterior spinal arteries, without connection to the subarachnoid space, is most often associated with external damage - for example, trauma.
Magnetic resonance imaging is performed not only at the diagnostic stage, but also during dynamic monitoring of the effectiveness of therapy:
- MRI signs of incomplete cavity formation (the so-called "presyrinx"): spinal cord expansion without neoplasm, associated with the presence of interstitial edema;
- MRI signs of cavity collapse: vertically flattened cavity, stretched in horizontal size, with spinal cord atrophy.
A repeated magnetic resonance imaging procedure is performed according to indications. If the pathology is relatively stable, then repeated studies can be performed once every 2 years.
- X-ray of the skull, craniovertebral zone, spinal column, upper limbs, joints is performed depending on the location of the pathology and its clinical characteristics. With syringomyelia, it is possible to identify skeletal development defects, neurodystrophic processes, osteoporosis foci, arthropathies, bone anomalies, etc. The degree of expression of pathological changes allows us to assess the severity and prognosis of the disorder.
- Computer tomography is not as informative as MRI or X-ray. The appearance of a pathological cavity can only be detected in combination with myelography and water-soluble contrast. [ 16 ]
- Electromyography helps to clarify the presence of damage to the motor neurons of the anterior spinal horns and to identify the problem even in the preclinical period of the anterior horn process.
- Electroneuromyography allows us to see the initial pyramidal disturbances and axonal degeneration.
- Electroencephalography is necessary to determine the impaired function of the brain stem structures and the first signs of syringobulbia.
- Echoencephalography is used to detect syringoencephaly and helps to identify an enlarged ventricular system in the brain.
- Esthesiometric diagnostics is used to clarify the location and intensity of sensitivity disorders.
Differential diagnosis
Differential diagnostics are carried out with the following pathologies and conditions:
- Intramedullary tumor (especially when affecting the cervical spine) and tumors of the medulla oblongata are determined based on the results of magnetic resonance imaging.
- Hematomyelia – characterized by an acute onset of symptoms immediately after injury, with a subsequent regressive course. Diagnosis is complicated by hemorrhage into the syringomyelic cavity.
- Amyotrophic lateral sclerosis is characterized by a rapid rate of development and features of pathological changes that are noted during visualization of the spinal cord.
- Cervical ischemic myelopathy has a specific etiology of development, is characterized by sensitivity disorders according to the dynamic principle and characteristic signs in spondylography and MRI.
- Spinal cord cysts, tumors, post-traumatic or cystic myelopathy, spinal arachnoiditis, tuberculous spondylitis.
- Craniovertebral defects (hypoplastic processes in the atlas and axis, platybasia, basilar impression, etc.) are accompanied by neurological symptoms, without the formation of cystic formations. The main method of differentiation is MRI.
- Raynaud's disease, angiotrophopathy.
- Compression-ischemic neuropathies (carpal or cubital tunnel syndromes). [ 17 ]
Do Arnold Chiari malformation and syringomyelia require differentiation? These two pathologies often accompany each other: the formation of spinal cord cavities is combined with the displacement of the cerebellar tonsils and sometimes the trunk and the fourth ventricle below the level of the foramen magnum. Often the “culprit” of the pathology is a genetic factor, and treatment is possible only with the help of surgical intervention. [ 18 ]
Syringomyelia and hydromyelia require mandatory differentiation. The so-called hydrocele of the spinal cord is characterized by a significant increase in the volume of cerebrospinal fluid and an increase in its pressure. Hydromyelia often coexists with syringomyelia, but it is important to know that these two terms are not identical and mean two different pathologies. The diagnosis is established on the basis of clinical, radiological and tomographic data. [ 19 ]
Syringomyelia and syringobulbia are not quite synonymous. Syringobulbia is said to occur when the pathological process in syringomyelia extends to the brainstem area, which is accompanied by characteristic symptoms: nystagmus, bulbar disorders, and dissociated anesthesia of part of the face.
Who to contact?
Treatment syringomyelia
However, the most effective treatment for syringomyelia is considered to be surgical intervention. Surgery is unconditionally prescribed when neurological insufficiency progresses, in particular, when central paresis of the lower extremities or peripheral paresis of the upper extremities develops. The intervention consists of dissecting the central spinal canal with subsequent drainage. The operation is truly effective: most patients experience a cessation of the development of the pathology and a reduction in neurological disorders. Post-traumatic and post-infectious linear syringomyelia is corrected by performing a shunt between the cystic formation and the subarachnoid space. If the underlying cause of the pathology is an intramedullary tumor, the neoplasm is removed. Cerebellar herniation is an indication for decompression of the posterior cranial fossa.
Prevention
The main preventive action to prevent the development of syringomyelia is to avoid actions that can disrupt the dynamics of the cerebrospinal fluid. It is important to minimize the likelihood of increased intra-abdominal and intracranial pressure: do not lift heavy objects, avoid excessive physical exertion (including strong static stress), intense coughing and sneezing, straining, etc. You should also avoid spinal and head injuries, lead a healthy and moderately active lifestyle. Physical inactivity is not welcome.
If the diagnosis of syringomyelia has already been made, then prevention of the worsening of the disease should be carried out. The following are considered mandatory:
- dispensary neurological registration;
- systematic diagnostic procedures to monitor the dynamics of the pathology (magnetic resonance imaging – once every 2 years or more often, depending on the indications);
- regular examinations by a neurologist (1-2 times a year).
Syringomyelia is considered a dynamic pathology, and constant clinical observation and diagnostic measures will help to determine the deterioration of the pathological process in time and take appropriate therapeutic measures. This is necessary, in particular, in case of syringomyelia in childhood, when it is important to correctly assess the indications for surgical treatment: there are cases of spontaneous healing of such a disorder if its development was associated with rapid growth of the skeletal system.
Forecast
Syringomyelia causes damage to the spinal structures, resulting in impaired motor abilities and sensitivity in the body and limbs. Loss of pain and temperature sensations can lead to serious injuries and burns. Motor dysfunction is accompanied by muscle weakness and atrophy.
In turn, syringomyelia can cause the appearance and worsening of spinal column deformations: patients often develop scoliosis. Rarely, but it happens that the pathology is not accompanied by any symptoms and is discovered accidentally during MRI.
The prognosis for syringomyelia is determined by the severity and extent of clinical manifestations, the duration of the disease and its cause. For most patients, the only effective treatment is surgery, which stabilizes the circulation of cerebrospinal fluid. The type of surgical intervention is determined by a neurosurgeon.
Approximately every second patient with competent treatment tactics shows only mild pathological changes. There is information about spontaneous recovery, but such an outcome was noted only in isolated cases - mainly in pediatrics. Such cases were caused by intensive bone growth and natural spatial expansion for brain structures. More often, syringomyelia becomes a cause of disability.
In most patients, irreversible spinal cord disorders develop against the background of a prolonged course of pathology, which worsens the postoperative prognosis: many symptoms remain even after surgery. However, this does not mean that the operation is pointless and inappropriate: thanks to such treatment, it is possible to stop further progression of the disease.

