Medical expert of the article
New publications
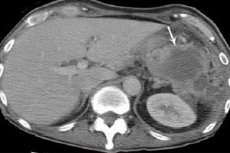
Subdiaphragmatic abscess.
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
When an internal infectious inflammation of tissues, accompanied by their destruction and purulent melting, is classified as a subdiaphragmatic abscess, this means that the abscess (a capsule-bound collection of pus) is located in the subcostal region of the abdominal cavity - in the space between the diaphragm separating the chest and abdominal cavities and the upper part of such abdominal organs as the liver, spleen, stomach and transverse colon.
Epidemiology
According to statistics, in more than 83% of cases, the formation of subdiaphragmatic abscesses is directly related to acute forms of diseases of the abdominal organs; and in two thirds of cases, this is the result of surgical intervention for these diseases.
In 20-30% of patients, a subdiaphragmatic abscess is formed after removal of a perforated purulent appendix; 50% - after operations related to the stomach, duodenum, gall bladder and bile ducts; in almost 26% - with purulent inflammation of the pancreas.
In less than 5% of cases, a subphrenic abscess develops without predisposing circumstances.
Right-sided subdiaphragmatic abscesses are diagnosed 3-5 times more often than left-sided ones; the proportion of bilateral foci of suppuration does not exceed 4-5% of cases.
Causes subdiaphragmatic abscess.
According to clinical surgery, in most cases the causes of subphrenic abscess are associated with surgeries: for perforated gastric ulcer or duodenal ulcer; acute perforated appendicitis; removal of cysts or gall bladder (cholecystectomy); removal of stones from bile ducts (choledocholithotomy) or reconstruction of ducts; splenectomy (removal of the spleen) or liver resection. The formation of subphrenic abscess is an extremely dangerous complication of such surgeries.
Also, a subdiaphragmatic abscess can be caused by combined injuries of the thoracoabdominal localization; acute inflammation of the gallbladder, bile ducts or pancreas ( purulent pancreatitis ). An abscess of this localization can be the result of a breakthrough of an intrahepatic pyogenic or amoebic abscess or a purulent echinococcal cyst. In rare cases, the suppurative process is caused by paranephritis or generalized septicopyemia.
As a rule, an abscess in the subdiaphragmatic zone is formed inside the abdominal cavity in the form of anterior, superior, posterior, pre-gastric, suprahepatic or perisplenic abscesses. They can also be median, right- and left-sided (more often - right-sided, that is, above the liver).
The location of the abscess behind the peritoneum is noted - in the tissue of the retroperitoneal space, which occupies a place below the diaphragm up to the lower pelvic organs. Such a retroperitoneal subdiaphragmatic abscess occurs due to an infection that gets here with the flow of lymph or blood during purulent inflammation of the appendix, pancreas, adrenal glands, kidneys or intestines.
Risk factors
Risk factors for the development of postoperative subphrenic abscess, as well as other infectious complications in surgery, include the presence of diabetes mellitus or severe renal dysfunction in patients; significant blood loss, childhood and old age, and the use of glucocorticosteroids or cytostatics that reduce general immunity. Chronic syndrome is more often observed in patients who have previously taken antibiotics.
Pathogenesis
The pathogenesis of the formation of a subdiaphragmatic abscess consists of an inflammatory reaction induced by a combination of aerobic and anaerobic bacteria (Staphylococcus spp., Streptococcus spp., Escherichia coli, Pseudomonas aeruginosa, Klebsiella spp., Bacteroides fragilis, etc.) present in the inflamed organ, as well as due to bacterial contamination - infection of the surgical area with hospital-acquired microbes.
As a result of the activation of macrophages and other immunocompetent cells at the site of bacterial penetration - around the pyogenic cavity with dead cells and leukocytes - a connective tissue capsule is formed, separating the suppuration zone from healthy tissues and constantly replenished with purulent exudate.
Symptoms subdiaphragmatic abscess.
Doctors point out that the symptoms of subdiaphragmatic abscess are typical for intracavitary inflammatory processes with purulent exudation, but their intensity depends on the course of the etiologically related disease and the localization of suppuration. And the clinical features of the manifestation of this pathology can vary from a severe acute disease to an insidious chronic process with intermittent fever, loss of appetite and weight, anemia and nonspecific symptoms.
The first signs are malaise and a state of general weakness. Very quickly, a sharp increase in body temperature (up to +38.5-40°C) during the daytime with some decrease at night joins in, that is, there is a long-term fever with attacks of chills and night hyperhidrosis.
Symptoms of subphrenic abscess also include: pain under the costal arch, above the 8-11 ribs (when palpating the abdomen - muscle tension and pain in the right upper quadrant), pain radiating to the shoulder and under the shoulder blade and intensifying with deep breathing; cough, frequent and shallow breathing (with the epigastric region often sinking during inhalation); hiccups, belching, bad breath, nausea and vomiting. Many patients adopt a forced semi-sitting position.
Blood tests show an increase in the number of leukocytes (leukocytosis) and an increase in the erythrocyte sedimentation rate (ESR). Radiography reveals pleural fluid in approximately 80% of patients, and gas bubbles above the fluid in a third of them.
Complications and consequences
Consequences and complications of subdiaphragmatic abscess: perforation of the pyogenic capsule through the diaphragm and penetration of purulent exudate into the lungs and pleural cavity (pulmonary empyema, pyothorax, reactive pleurisy), into the peritoneal cavity or pericardium (pericardium), as well as into the intestinal lumen. In the absence of treatment or an erroneous diagnosis, the consequences of subdiaphragmatic abscess are peritonitis, sepsis, septic shock and death.
 [ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ]
[ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ]
Diagnostics subdiaphragmatic abscess.
In order to diagnose subphrenic abscess in a timely manner, there is a rule in surgery: any patient with fever of unknown origin who has had abdominal surgery (even if the surgery was performed several months earlier) should be suspected of having a chronic intra-abdominal, primarily subphrenic, abscess.
The examination necessarily includes blood tests, and instrumental diagnostics - X-ray examination (in two projections), ultrasound examination and computed tomography of the abdominal cavity and diaphragm area.
What do need to examine?
How to examine?
Differential diagnosis
Differential diagnostics is of great importance due to the localization of suppuration in the intrathoracic part of the abdominal cavity. Existing diagnostic criteria (by blood composition and instrumental visualization) contribute to the correct identification of this type of purulent-inflammatory process.
Treatment subdiaphragmatic abscess.
Treatment of subphrenic abscess is surgical treatment, which is carried out in a hospital setting.
A transthoracic (transpleural) or transabdominal opening of the subdiaphragmatic abscess and removal of pus from its cavity (using suction) is performed. The cavity is then washed with antiseptic agents and drains are installed with suturing of the wound.
After this, drug treatment continues, and the main drugs here are antibiotics. First of all, drugs of the cephalosporin group are used by parenteral administration: Cefotaxime, Cefazolin, Ceftriaxone, etc., which are administered either intramuscularly or intravenously (drip) - 0.25-0.5 g every 8 hours (in severe cases, 1-2 g).
Flucloxacillin, Trimethoprim-sulfamethoxazole (Biseptol, Bactrim, Co-trimoxazole, Septrim and other trade names), Clindamycin (Dalacin, Clindacin, Klizimin) are also used.
The antibiotic lincosamide Clindamycin is prescribed in the form of injections - 2.5-2.8 g per day. Among its contraindications, the only ones noted are the presence of enteritis or colitis. However, like all antibacterial agents, this drug can cause side effects (changes in the blood, urticaria, decreased blood pressure, abdominal pain, nausea, diarrhea, intestinal dysbiosis).
Forecast
The prognosis of the outcome of an intra-abdominal abscess in the subdiaphragmatic region - with its average statistical mortality of 10-20% - is determined by specialists taking into account several factors. And the key condition for safety for the life of patients is the timely opening of the subdiaphragmatic abscess and adequate subsequent therapy.

