Medical expert of the article
New publications
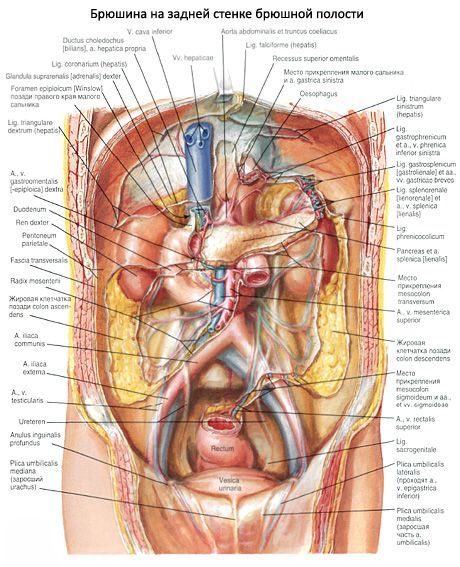
Bruchina
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The peritoneum is a thin serous membrane that lines the abdominal cavity and covers many of the organs located within it.
The peritoneum adjacent to the internal organs, partially or completely covering many of them, is called the visceral peritoneum (peritoneum viscerale). The peritoneum lining the walls of the abdomen is called the parietal peritoneum (peritoneum parietale).
The abdominal cavity space limited by the peritoneum - a narrow gap between the peritoneal layers is called the peritoneal cavity (cavitas peritonei). At the bottom, the peritoneal cavity descends into the pelvic cavity. In men, the peritoneal cavity is closed, in women it communicates with the external environment through the abdominal openings of the fallopian tubes, the uterine cavity and the vagina. The peritoneal cavity contains a small amount of serous fluid, which moistens the peritoneum and ensures free sliding of the organs in contact with each other.
The peritoneum, passing from organ to organ, forms ligaments (folds). Two sheets of peritoneum, going from the back wall of the peritoneal cavity to the organ, form the mesentery of this organ.
Between the mesenteric layers are located vessels and nerves. The line of the beginning of the mesentery on the back wall of the abdominal cavity is called the root of the mesentery.
The peritoneum is formed by several alternating layers of collagen and elastic fibers covered on the side of the peritoneal cavity by flat (mesothelial) cells. The surface area of the peritoneum is 1.7 m. The peritoneum performs covering and protective functions, contains immune structures (lymphoid nodules), adipose tissue (fat depot). The peritoneum fixes the internal organs by means of ligaments and mesenteries.
The relationship of the peritoneum to the internal organs is not the same. The kidneys, adrenal glands, ureters, most of the duodenum, pancreas, abdominal aorta, and inferior vena cava are located retroperitoneally (retro- or extraperitoneally). These organs are covered by the peritoneum on one side (in front). Organs covered by the peritoneum on three sides are located mesoperitoneally in relation to it (ascending and descending colon, middle third of the rectum). Organs that are covered by the peritoneum on all sides occupy an intraperitoneal (intraperitoneal) position. This group of organs includes the stomach, jejunum and ileum, transverse and sigmoid colon, upper part of the rectum, spleen, and liver.
Covering the anterior abdominal wall, the parietal peritoneum passes onto the diaphragm at the top, onto the lateral walls of the abdominal cavity at the sides, and onto the lower wall of the pelvic cavity at the bottom. There are 5 folds on the anterior abdominal wall in the pelvic area. The unpaired median umbilical fold (plica umbilicalis mediana) goes from the apex of the urinary bladder to the navel, it contains an overgrown urachus covered with peritoneum. The paired medial umbilical fold (plica umbilicalis medialis) at its base (each) contains an overgrown umbilical artery. The paired lateral umbilical fold (plica umbilicalis lateralis) is formed by the inferior epigastric artery, also covered by the parietal peritoneum. Between the folds there are pits - weak spots in the anterior abdominal wall (areas of possible formation of inguinal hernias). Above the urinary bladder, on either side of the median umbilical fold, are the right and left supravesical fossae (fossae supravesicales dextra et sinistra). Hernias do not form here. Between the medial and lateral umbilical folds, there is a medial inguinal fossa (fossa inguinalis medialis) on each side. Each such fossa corresponds to the superficial ring of the inguinal canal. Outside of the lateral umbilical fold, there is a lateral inguinal fossa (fossa inguinalis lateralis). In the lateral inguinal fossa, there is a deep ring of the inguinal canal.
The parietal peritoneum of the anterior abdominal wall above the navel forms a fold - the falciform ligament of the liver (lig.falciforme, s.hepatis). From the abdominal wall and diaphragm, this ligament goes down to the diaphragmatic surface of the liver, where both of its leaves pass into the visceral cover (peritoneum) of the liver. In the free lower (anterior) edge of the falciform ligament is the round ligament of the liver, which is an overgrown umbilical vein. The leaves of the falciform ligament diverge to the sides at the back and pass into the coronary ligament of the liver. The coronary ligament (lig.coronarium) is located frontally and represents the transition of the visceral peritoneum of the diaphragmatic surface of the liver into the parietal peritoneum of the posterior wall of the peritoneal cavity. At the edges, the coronary ligament expands and forms the right and left triangular ligaments (ligg.triangularia dextra et sinistra). The visceral peritoneum of the lower surface of the liver covers the gallbladder from below. From the lower surface of the liver, from the area of its gates, the visceral peritoneum in the form of two sheets goes to the lesser curvature of the stomach and the initial section of the duodenum. These two sheets of the peritoneum form the hepatogastric ligament (lig.hepatogastricum), located on the left, and the hepatoduodenal ligament (lig.hepatoduodenale), located on the right. In the thickness of the hepatoduodenal ligament, from right to left, are the common bile duct, the portal vein (slightly behind) and the proper hepatic artery, as well as lymphatic vessels and nodes, nerves. The hepatogastric and hepatoduodenal ligaments together form the lesser omentum (omentum minus).
The sheets of the visceral peritoneum of the anterior and posterior walls of the stomach in the area of its greater curvature continue (hang down) to the level of the superior aperture of the lesser pelvis (or slightly higher), and then fold back and rise upward, to the posterior wall of the abdomen (at the level of the pancreas). The four sheets of the visceral peritoneum formed below the greater curvature of the stomach form the greater omentum (omentum majus). At the level of the transverse colon, all four sheets of the greater omentum fuse with the omental band of the anterior wall of the transverse colon. Then the posterior sheets of the greater omentum lie on top of the mesentery of the transverse colon, go to the posterior abdominal wall and pass into the parietal peritoneum of the posterior wall of the abdominal cavity. Approaching the anterior edge of the pancreas, one leaf of the peritoneum (the posterior plate of the greater omentum) passes onto the anterior surface of the pancreas, the other goes down and passes into the superior leaf of the mesentery of the transverse colon. The part of the greater omentum between the greater curvature of the stomach and the transverse colon is called the gastrocolic ligament (lig.gastrocolicum). The greater omentum covers the small intestine and parts of the colon in front. Two leaves of the peritoneum, going from the greater curvature of the stomach to the hilum of the spleen, form the gastrosplenic ligament (lig.gastrolienale). The leaves, going from the cardiac part of the stomach to the diaphragm, form the gastrophrenic ligament (lig.gastrophrenicum). The phrenic-splenic ligament (lig.phrenicolienale) is a duplication of the peritoneum, going from the diaphragm to the posterior end of the spleen.
The peritoneal cavity is divided into upper and lower floors, the boundary between which is the transverse colon and its mesentery. The upper floor of the peritoneal cavity is limited from above by the diaphragm, on the sides by the lateral walls of the peritoneal (abdominal) cavity, and from below by the transverse colon and its mesentery. The mesentery of the transverse colon passes onto the posterior wall of the abdominal cavity at the level of the posterior ends of the 10th ribs. The stomach, liver, and spleen are located in the upper floor of the peritoneal cavity. At the level of the upper floor are the retroperitoneal pancreas and the upper sections of the duodenum (its initial part, the bulb, is located intraperitoneally). In the upper floor of the peritoneal cavity, three relatively limited receptacles are distinguished - bursae: hepatic, forestomachic, and omental.
The hepatic bursa (bursa hepatica) is located in the right hypochondrium and contains the right lobe of the liver. This bursa has a suprahepatic fissure (subdiaphragmatic space) and a subhepatic fissure (subhepatic space). The hepatic bursa is bounded by the diaphragm above, by the transverse colon and its mesentery below, by the falciform ligament of the liver on the left, and by the coronary ligament behind (in the upper sections). The hepatic bursa communicates with the forestomachic bursa and the right lateral canal.
The pregastric bursa (bursa pregastrica) is located in the frontal plane, in front of the stomach and the lesser omentum. The right border of this bursa is the falciform ligament of the liver, the left border is the phrenic-colic ligament. The upper wall of the pregastric bursa is formed by the diaphragm, the lower wall by the transverse colon, and the anterior wall by the anterior abdominal wall. On the right, the pregastric bursa communicates with the subhepatic fissure and the omental bursa, and on the left, with the left lateral canal.
The omental bursa (bursa omentalis) is located behind the stomach, lesser omentum and gastrocolic ligament. The omental bursa is bounded above by the caudate lobe of the liver, and below by the posterior plate of the greater omentum, fused with the mesentery of the transverse colon. Behind, the omental bursa is bounded by the parietal peritoneum covering the aorta, inferior vena cava, upper pole of the left kidney, left adrenal gland and pancreas. The cavity of the omental bursa is a frontally located slit with three depressions (pockets). The superior omental recess (recessus superior omentalis) is located between the lumbar part of the diaphragm behind and the posterior surface of the caudate lobe of the liver in front. The splenic recess (recessus splenius lienalis) is bounded in front by the gastrosplenic ligament, behind by the phrenic-splenic ligament, and on the left by the hilum of the spleen. The inferior omental recess (recessus inferior omentalis) is located between the gastrocolic ligament above and in front and the posterior plate of the greater omentum, fused with the mesentery of the transverse colon, behind. The omental bursa communicates with the hepatic bursa (subhepatic fissure) through the omental foramen (foramen epiploicum, s.omentale), or vinsloy foramen. This opening, 3-4 cm in size, is limited in front by the hepatoduodenal ligament, containing the portal vein, hepatic artery and common hepatic duct. The posterior wall of the opening is formed by the parietal peritoneum covering the inferior vena cava. Above, the omental foramen is limited by the caudate lobe of the liver, below - by the upper part of the duodenum.
The lower floor of the peritoneal cavity is located under the transverse colon and its mesentery. From below, it is limited by the parietal peritoneum lining the bottom of the small pelvis. In the lower floor of the peritoneal cavity, there are two paracolic grooves (two lateral canals) and two mesenteric sinuses. The right paracolic groove (sulcus paracolicus dexter), or right lateral canal, is located between the right abdominal wall and the ascending colon. The left paracolic groove (sulcus paracolicus sinister), or left lateral canal, is limited by the left abdominal wall and the descending colon. On the posterior wall of the peritoneal cavity, between the ascending colon on the right and the descending colon on the left, there are two mesenteric sinuses, the border between which is formed by the root of the mesentery of the small intestine. The root of the mesentery extends from the level of the duodenojejunal junction on the left on the posterior wall of the peritoneal cavity to the level of the sacroiliac joint on the right. The right mesenteric sinus (sinus mesentericus dexter) is limited on the right by the ascending colon, above by the root of the mesentery of the transverse colon, on the left by the root of the mesentery of the jejunum and ileum. Within the right mesenteric sinus, the retroperitoneal terminal section of the descending part of the duodenum and its horizontal part, the lower part of the head of the pancreas, part of the inferior vena cava from the root of the mesentery of the small intestine below to the duodenum above, as well as the right ureter, vessels, nerves, and lymph nodes are located. The right mesenteric sinus contains part of the ileal loops. The left mesenteric sinus (sinus mesentericus sinister) is limited on the left by the descending colon and the mesentery of the sigmoid colon, and on the right by the root of the mesentery of the small intestine. Below, this sinus widely communicates with the pelvic cavity. Within the left mesenteric sinus, the ascending part of the duodenum, the lower half of the left kidney, the terminal section of the abdominal aorta, the left ureter, vessels, nerves, and lymph nodes are located retroperitoneally; the sinus contains mainly loops of the jejunum.
The parietal peritoneum, lining the posterior wall of the peritoneal cavity, has depressions (pits) - possible sites for the formation of retroperitoneal hernias. The superior and inferior duodenal recesses (recessus duodenales superior et inferior) are located above and below the duodenojejunal flexure.
The superior and inferior ileocaecal recesses (recessus ileocaecalis superior et inferior) are located above and below the ileocaecal junction. Under the dome of the cecum there is a retrocecal recess (recessus retrocaecalis). On the left side of the root of the sigmoid mesentery there is an intersigmoid recess (recessus intersygmoideus).
In the pelvic cavity, the peritoneum, passing onto its organs, also forms depressions. In men, the peritoneum covers the anterior surface of the upper part of the rectum, then passes onto the posterior and then onto the upper wall of the urinary bladder and continues into the parietal peritoneum of the anterior abdominal wall. Between the urinary bladder and the rectum there is a rectovesical recess (exavacio recto vesicalis) lined with peritoneum. It is bounded on the sides by rectovesical folds (plicae recto vesicales), running in the anteroposterior direction from the lateral surfaces of the rectum to the urinary bladder. In women, the peritoneum from the anterior surface of the rectum passes onto the posterior wall of the upper part of the vagina, rises further upward, covers the uterus and fallopian tubes from behind and then from the front and passes onto the urinary bladder. Between the uterus and the urinary bladder there is a vesicouterine recess (exavacio vesicoutenna). The deeper rectouterine pouch (exavacio rectouterina), or Douglas's pouch, is located between the uterus and the rectum. It is also lined with peritoneum and is bounded on the sides by the rectouterine folds (plicae rectouterinae).
The peritoneal lining of the intestine is largely associated with the transformation of the mesenteries of the primary intestine. In the first month of embryogenesis, the trunk intestine (below the diaphragm) is suspended from the anterior and posterior walls of the embryo by means of the ventral and dorsal mesentery, derivatives of the splanchnopleura. The ventral mesentery below the umbilical opening disappears early, and the upper part is transformed into the lesser omentum and the falciform ligament of the liver. The dorsal mesentery changes its position as a result of increased growth (expansion) of the greater curvature of the stomach and its rotation downwards and to the right. As a result of the rotation of the stomach from the sagittal position to the transverse position and increased growth of its dorsal mesentery, the dorsal mesentery emerges from under the greater curvature of the stomach, forming a pocket-like protrusion (the greater omentum). The posterior part of the dorsal mesentery continues onto the posterior wall of the abdominal cavity and also gives rise to the mesenteries of the small and large intestines.
From the anterior wall of the forming duodenum, paired ectodermal protrusions grow into the thickness of the ventral mesentery - the rudiments of the liver and gall bladder. The pancreas is formed from the fused ventral and dorsal protrusions of the endoderm of the future duodenum, growing into the dorsal mesentery. As a result of the rotation of the stomach and the growth of the liver, the duodenum and pancreas lose mobility and acquire a retroperitoneal position.
Age-related features of the peritoneum
The peritoneum of a newborn is thin and transparent. Subperitoneal fatty tissue is poorly developed. Therefore, blood vessels and lymph nodes are visible through the peritoneum.
The lesser omentum is relatively well formed, the omental opening in a newborn is large. The greater omentum at this age is short and thin. It only partially covers the loops of the small intestine. With age, the greater omentum lengthens, thickens, and a large amount of fatty tissue and lymphoid nodules appear in its thickness. The depressions of the parietal peritoneum, folds, and pits formed by the peritoneum are poorly expressed. Their depth increases with age. Often, with increasing age, especially in older people, adhesions (adhesions) form between the visceral and parietal layers of the peritoneum, which affects the functional state of the internal organs.
What do need to examine?
How to examine?


 [
[