Medical expert of the article
New publications
Sleepwalking or sleepwalking
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
In the International Classification of Diseases (ICD-10) there is no pathology of sleepwalking, but there is sleepwalking (medical name somnambulism) – class V (mental and behavioral disorders), code – F51.3.
Since time immemorial, this unusual state in sleep, accompanied by unconscious movement, some actions and even speech, has been attributed to the negative influence of moonlight (especially during the full moon). In fact, the moon has nothing to do with it: sleepwalking is a type of sleep disorder - parasomnia.
Epidemiology
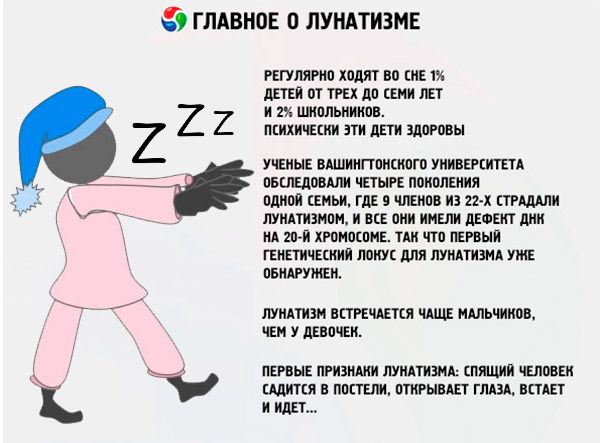
Sleepwalking is more common in boys than in girls. The peak of this parasomnia is between 8 and 12 years of age, although manifestation is noted at an earlier age. According to the latest data (2015), the overall prevalence of sleepwalking in childhood – from 2.5 to 13 years – is 29.1%.
Adult sleepwalking is thought to affect up to 2.5-3% of the population. According to a 2010-2012 study by a team of scientists from the American Academy of Neurology (AAN) under the auspices of the National Institutes of Health, sleepwalking is much more common in adults than previously thought.
As Neurology Journal (2012, May) writes, sleepwalking is provoked by depression, anxiety, and obsessive-compulsive disorders. Of the 15,929 Americans over 18 (involved in the study), almost a third had a history of sleepwalking. In 3.6%, such an incident was noted only once a year; in 2.6%, sleepwalking attacks occurred monthly. Moreover, 17% of the participants had sleepwalkers among their blood relatives.
People suffering from depression "travel" in their sleep 3.5 times more often than those who do not have prolonged depressive states. And with obsessive-compulsive disorders, somnambulism is observed in 7.3% of patients.
Causes sleepwalking
Most experts see the key causes of sleepwalking in neurosis, which arises from life circumstances that traumatize the psyche and internal contradictions of the personality and can lead to certain disorders of the nervous system functions, in particular, the processes of excitation and inhibition in the cerebral cortex. That is, sleepwalking occurs as a psychogenic neurotic reaction.
Risk factors
Risk factors for such a CNS reaction include:
- severe fatigue, lack of sleep (prolonged disruption of its schedule), anxiety, stress, depression;
- obsessive-compulsive disorders (in adults, sleepwalking and obsessive thoughts are possible, i.e. obsessive-compulsive neurosis );
- strokes;
- traumatic brain injury;
- fever;
- migraine with aura;
- encephalitis and other brain infections;
- hyperthyroidism;
- sleep apnea syndrome;
- essential narcolepsy (Gelineau disease);
- neurodegenerative changes in the brain (in Alzheimer's or Parkinson's diseases);
- taking tricyclic antidepressants, neuroleptics, sleeping pills;
- drug addiction;
- alcohol abuse (causes alcoholic sleepwalking).
Sleepwalking in children, as well as sleepwalking in teenagers, is not that uncommon: according to a survey conducted by the National Sleep Foundation (USA), 1% of children aged three to seven and 2% of schoolchildren regularly sleepwalk. These children are mentally healthy, and in most cases, parasomnia goes away as they grow older.
According to neuropsychiatrists, more attention should be paid to sleepwalking in adults - when all the structures of the brain have long been formed, and this sleep disorder may indicate the onset of irreversible neurodegenerative processes.
Is sleepwalking related to epilepsy? Since a phase similar to paradoxical sleep has been identified during an epileptic seizure, and epileptics are unable to remember events that occurred before the seizure, sleepwalking is considered part of the complex of epileptic symptoms in patients with this disease.
And one more question: is sleepwalking hereditary? A family tendency to this type of parasomnia was traced by specialists back in the 1980s. And in 2011, it was reported that scientists from the University of Washington examined four generations of one family, where 9 members out of 22 suffered from sleepwalking, and all of them had a DNA defect on the 20th chromosome. So the first genetic locus for sleepwalking has already been discovered. According to the journal of the American Medical Association JAMA Pediatrics, 48-61% of children with sleepwalking have one or both parents who are sleepwalkers.
Pathogenesis
The pathogenesis of sleepwalking is associated with changes in the normal neurophysiological mechanism of sleep or with individual characteristics of the bioelectrical activity of the cerebral cortex and subcortex during night sleep.
By the way, those who sleep for a long time during daylight hours, despite the fact that the weakening of alpha waves of the brain occurs at night, may experience sleepwalking during the day.
From the moment of falling asleep until awakening, there are five repeating sleep cycles, during which there are alternating periods of orthodox slow-wave sleep (NREM - without eye movement under closed eyelids) and rapid-paradoxical sleep (REM - with closed eye movement). Their average ratio in the structure of night sleep is 80% and 20%, respectively.
Immediately after a person falls asleep, alpha waves in the brain weaken and are replaced by theta waves, which leads to a decrease in muscle activity, body temperature, heart rate and breathing, and a slowdown in metabolism. This is slow-wave sleep (NREM), and as it deepens, the bioelectric signals generated by the brain become predominantly delta waves. At the same time, some subcortical and cortical neurons are truly inactive during sleep, while other groups of neurons can be variably active. Thus, the reticular formation of the brain and the structures of the hippocampus will react to any external stimuli even during sleep, initiating movement to maintain the integrity of the body. Subcortical thinking (the subconscious) is very active during sleep.
During periods of rapid eye movement (REM) sleep, which briefly replace slow-wave sleep, the opposite is true: the pulse and breathing quicken, cerebral blood flow increases, the adrenal glands synthesize hormones faster, and the activity of neurons in the brain is very similar to their state during wakefulness.
Sleepwalking attacks occur in the first two hours after falling asleep – during the third stage of the deepest sleep NREM, when the parasympathetic nervous system, which maintains homeostasis, dominates. Sleepwalking occurs in people with sleep stage disorders, when the brain gets “stuck” in the slow-wave sleep stage, desynchronization of bioelectric signals in the brain occurs, and part of the cortex and certain areas of the subcortex are brought into a state of partial physiological activity.
The pathogenesis of sleepwalking in children and adolescents also depends on the maturity of the brain structures that ensure the functional activity of the central nervous system. In childhood and adolescence, the hypothalamic-pituitary system works intensively (producing the growth hormone somatotropin), and the bioelectrical activity of the cerebral cortex has its own characteristics. Thus, the synchronization of its biopotentials increases at 6-10 years, decreases at 11-14 years, and increases again after 15-16 years. With a decrease in the level of synchronization, the processes of excitation of the central nervous system prevail, multiple disorders of vegetative functions are observed.
But sleepwalking, according to Freud, is a sign of unresolved emotional conflict and is an attempt to satisfy unconscious instinctive needs.
Symptoms sleepwalking
The first signs of sleepwalking: the sleeping person sits up in bed, opens his eyes, gets up and walks...
The obligatory symptoms of sleepwalking are: empty, glassy eyes and a blank expression on the face; clumsiness of movements; lack of reaction to the surroundings and confusion.
A sleepwalker may wander around the apartment, start getting dressed, pick up objects, rearrange things in the room, climb into a closet, climb onto a windowsill; may leave the house and walk in an unknown direction (including along the roadway). Sleepwalking children may calmly walk to their parents' bedroom or simply towards the light; a common symptom is enuresis and grinding of teeth in their sleep (bruxism).
A sleepwalking attack can last less than a minute or can last for half an hour. It is very difficult to wake a person in this state, since the brain is resistant to stimulation during deep sleep.
The patient can lie down and calm down anywhere. And when he wakes up, he remembers nothing and becomes confused. However, adults sometimes remember individual moments of what happened.
In the list of symptoms, sleepwalking and somniloquy are called sleepwalking and sleeptalking, that is, talking out loud during sleep. Somniloquy also refers to parasomnia and manifests itself in different ways: mumbling, quite loud sounds, screams and even long, often indistinct, speech. Most often, a sleeping person begins to talk during a less deep delta wave of the orthodox stage of sleep. Sleepwalking and somniloquy in the form of screams are more common in children and adolescents, especially when combined with nightmares.
Sleepwalking in adults may include elements of aggression, as well as inappropriate actions. Indecent exposure and even sexual activity in a state of somnambulism are possible. Until 2003, doctors defined this as sexual behavior in sleep; but there was a tendency to single out sexual sleepwalking, which – following the efforts of a group of Canadian neurologists (Shapiro C., Trajanovic N., Fedoroff J.) – is now called sexsomnia.
Complications and consequences
According to doctors, sleepwalking in itself does not harm children and adolescents emotionally, since memory does not record these "night walks", and sleepwalking is not considered a sign of mental illness. But then what is dangerous about sleepwalking?
Sleepwalkers can easily injure themselves, for example, when going down stairs, falling, or attempting to jump from a height. Long-term sleep disturbance can lead to excessive daytime sleepiness and possibly problems with academic performance and behavior at school.
Undesirable consequences for others cannot be ruled out – when actions in a parasomnic state are of an aggressive and violent nature (especially in men).
It is a common misconception that sleepwalkers should not be woken up; in fact, they should be woken up, otherwise the "walk" may end in an accident. However, it is recommended that children not be disturbed, but carefully returned to bed.
Diagnostics sleepwalking
Diagnosis of sleepwalking should be carried out by a neurologist, psychiatrist or somnologist.
To determine the degree of brain activity and study sleep characteristics, specialists use instrumental diagnostics:
- electroencephalogram (EEG);
- electromyogram (EMG);
- electrooculogram (EOG);
- polysomnography.
Differential diagnosis
The task performed by differential diagnostics is to identify neurodegenerative changes in the brain (MRI is used), obsessive-compulsive disorders and other conditions in which parasomnias may be observed. And to differentiate them from delirium and hallucinations.
Who to contact?
Treatment sleepwalking
In the vast majority of cases, sleepwalking is not treated: comprehensive therapeutic care should be provided for the disease that led to the development of parasomnia.
Most often, the problem can be eliminated or at least the symptoms of sleepwalking in a child can be alleviated by improving sleep hygiene. For example, experts recommend regular relaxing procedures before bedtime. If sleepwalking in children occurs frequently, doctors may recommend using scheduled awakening – 45-50 minutes after the child falls asleep. This disrupts the sleep cycle and prevents an attack.
Hypnosis can be used to treat sleepwalking in adults. In addition, some may be prescribed pharmacological agents, such as sleeping pills, sedatives, or antidepressants. Thus, as a first-line treatment for sexsomnia (sexual sleepwalking), Clonazepam tablets (other names: Klonopin, Ictoril, Rivotril) are used - 0.5 mg an hour before bedtime. This psychotropic drug is contraindicated in kidney disease, liver problems, muscle weakness, and pregnancy. Side effects include nausea, ataxia, depression, and increased irritability. Long-term use causes addiction.
The most important thing in sleepwalking is to prevent injuries during attacks. The child should not sleep on top of a bunk bed; windows and the door to the balcony should be tightly closed at night, unnecessary furniture should be removed (so that the sleepwalker does not trip), the lock on the entrance doors should be blocked (to prevent going outside).
Sleepwalking and the army
Many people are interested in whether people with sleepwalking are accepted into the army?
Fitness for military service in terms of health of servicemen of the National Guard of Ukraine undergoing medical examination in accordance with the Regulation on military medical examination in the Armed Forces of Ukraine, approved by the order of the Minister of Defense of Ukraine dated August 14, 2008 No. 402.
Appendix to Order No. 402, Article 18: behavioral syndromes, personality and emotional disorders F50-F69; F80-F99 (associated with eating disorders, with non-addictive substance abuse); behavioral and emotional disorders in adolescence (hyperkinetic, social, emotional, unspecified mental), etc. The ICD code for sleepwalking is F51.3.
If the listed behavioral syndromes and personality disorders: 1) are pronounced, with a tendency to repeated long-term decompensations or pathological reactions - the person is unfit for military service and is removed from military registration; 2) are moderately expressed with unstable compensation or compensated - the person is unfit for military service in peacetime, limitedly fit in wartime.


 [
[