Medical expert of the article
New publications
Shingles
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Herpes zoster (shingles, zona) is the result of reactivation of the varicella-zoster virus from a latent state in the dorsal root ganglia of the spinal cord.
An acute lesion of the central nervous system; characterized by vesicular eruptions and neuralgic pain in areas of the skin innervated by peripheral sensory nerves ascending to the affected ganglia. Treatment of herpes zoster includes antiviral drugs and possibly glucocorticoids for up to 72 hours after the onset of the rash.
Epidemiology
People who have previously had chickenpox are affected. Shingles is a secondary endogenous infection in relation to chickenpox.
Shingles is observed in people of all age groups - from children in the first months of life to elderly and old people who have previously had chickenpox. 75% of cases occur in people over 45 years old, while children and adolescents account for less than 10%. The incidence rate is 12-15 per 100,000 people. Patients with shingles are considered a source of infection for those who have not had chickenpox. The contagiousness index is no higher than 10%, since, unlike chickenpox, the virus is not constantly detected on the surface of the mucous membrane of the respiratory tract.
Cases of shingles are registered throughout the year; the disease does not have a pronounced seasonality.
Causes shingles
Shingles is caused by the same virus that causes chickenpox (human herpes virus type 3). Chickenpox is an acute invasive phase of the virus, herpes zoster (shingles) is a reactivation of the latent phase. Inflammatory changes appear in the spinal ganglia and associated dermatomes. In some cases, the inflammatory process affects the posterior and anterior horns of the gray matter, pia mater, posterior and anterior roots. Activation of the pathogen is caused by local damage affecting the ganglia of the posterior roots of the spinal cord; systemic diseases, especially Hodgkin's disease; taking immunosuppressants. Shingles occurs at any age, most often in the elderly, HIV-infected patients; it is most severe in immunocompromised individuals. Sometimes the causes of shingles are unknown.
Pathogens
Pathogenesis
Shingles develops as a secondary endogenous infection in individuals who have had chickenpox, in a clinically expressed, latent or latent form due to the reactivation of the varicella zoster virus (Varicella zoster virus), integrated into the genome of cells in the cranial and spinal sensory ganglia. The interval between primary infection and clinical manifestations of shingles is calculated in tens of years, but can be short and last for several months. The mechanism of reactivation of the varicella virus has not been sufficiently studied. Risk factors include old age and senile age, concomitant diseases, primarily oncological, hematological, HIV infection, drug addiction, use of glucocorticoids, cytostatics, radiation therapy. The risk group includes recipients of organ transplants. Reactivation of the virus can be provoked by stressful conditions, physical trauma, hypothermia, infectious diseases, alcoholism. Reactivation of the virus is associated with conditions accompanied by immunosuppression, primarily with partial loss of specific immunity.
As a result of activation of the chickenpox virus (Varicella zoster virus), ganglionitis develops with damage to the intervertebral ganglia, ganglia of the cranial nerves and damage to the posterior roots. The process may involve the vegetative ganglia, the substance and membranes of the brain and spinal cord. Internal organs may be affected. Spreading centrifugally along the nerve trunks, the virus enters the epidermal cells and causes inflammatory-degenerative changes in them, which is manifested by corresponding rashes within the innervation zone of the corresponding nerve, i.e. dermatome. Hematogenous spread of the virus is also possible, as evidenced by the generalized form of the disease, polyorgan lesions.
The pathological picture of herpes zoster is caused by inflammatory changes in the spinal ganglia and related areas of the skin, as well as in the posterior and anterior horns of the gray matter, posterior and anterior roots of the spinal cord and the pia mater. The morphology of the vesicles is identical to those in chickenpox.
Symptoms shingles
Three to four days before the symptoms of herpes zoster appear, prodromal signs include chills, fever, malaise, and gastrointestinal upset. Pain may be felt in the area of the future rash. Around the third to fifth day, characteristic clusters of vesicles on an erythematous base appear in the innervation zone of one or more spinal ganglia. Hyperesthesia is usually noted in the affected area, and the pain may be severe. The rash appears most often in the chest area and spreads to one side of the body. Approximately five days after its appearance, the vesicles begin to dry out and form a scab. The lesion may become generalized, with damage to other areas of the skin and visceral organs, especially in immunocompromised patients.
The first episode of shingles usually creates immunity (recurrence is noted in no more than 4% of cases). However, postherpetic neuralgia can persist for months or years, especially in old age. Infection of the trigeminal nerve leads to severe, constant pain. The pain of postherpetic neuralgia can be acute, constant, or episodic and debilitating.
In adults, the earliest symptoms of shingles are the appearance of radicular pain. The pain can be intense, paroxysmal, and is often accompanied by local hyperesthesia of the skin. In children, the pain syndrome is less pronounced and occurs 2-3 times less frequently. In the prodromal period, the appearance of rashes is preceded by such symptoms of shingles as weakness, malaise, fever, chills, muscle and joint pain, headache. In the area of the affected dermatome, a feeling of numbness, tingling, or burning is possible. The duration of the prodromal period varies from 1 to 7 days.
Symptoms of herpes zoster during the period of clinical signs are characterized by lesions of the skin and/or mucous membranes, manifestations of intoxication and neurological symptoms.
Vesicles are considered the main element of local and generalized skin rashes in herpes zoster; they develop in the germ layer of the epidermis.
At first, the exanthema looks like a pink-red spot, which quickly turns into tightly grouped vesicles ("clusters of grapes") with transparent serous contents, located on a hyperemic and edematous base. Their size does not exceed several millimeters. The contents of the vesicles quickly become cloudy, then the patient's condition improves, the temperature returns to normal, the vesicles dry up and become covered with a crust, after which there is no scar. Complete healing occurs within 2-4 weeks. With shingles, the rash has a segmental, unilateral character, usually capturing 2-3 dermatomes. The predominant localization of skin lesions in shingles is noted in the innervation zone of the branches of the trigeminal nerve, then, in descending order, in the area of the thoracic, cervical, lumbosacral, cervicothoracic segments. In 10% of patients, the spread of exanthema beyond the affected dermatomes is observed. Dissemination may be accompanied by the appearance of multiple or single elements of the rash, with a shorter period of regression. Generalization of the exanthema is noted 2-7 days after the appearance of the rash in the dermatome area, it may be accompanied by a deterioration in the general condition. In addition to typical vesicular rashes, in weakened patients the exanthema can transform into a bullous form, acquire a hemorrhagic character and be accompanied by necrosis. Necrotic rashes are observed in individuals with immunodeficiency (HIV infection, cancer). In these cases, scars remain at the site of the rash. In the area of the rash, widespread hyperemia of the skin and pronounced edema of the underlying tissues are determined. When the rash is localized in the area of the first branch of the trigeminal nerve, pronounced edema is often observed. The exanthema is accompanied by enlargement and moderate soreness of the regional lymph nodes. Children may have signs of acute respiratory infections. The elevated body temperature lasts for several days, accompanied by moderate symptoms of intoxication. During this period of the disease, general cerebral and meningeal symptoms of shingles are possible in the form of adynamia, drowsiness, diffuse headache, dizziness, vomiting. Symptoms of shingles appear on average 2-3 weeks.
Postherpetic neuralgia develops immediately after 2-3 weeks of illness. The pain is usually paroxysmal and intensifies at night, becoming unbearable. The severity of the pain decreases after some time, or it completely disappears within a few months. Chronicization of postherpetic neuralgia is observed rarely and only in immunocompromised individuals.
Shingles may occur with symptoms of radicular pain only, with single vesicles or without any rash at all. The diagnosis in such cases is established based on the increase in titers of antibodies to the chickenpox virus (Varicella zoster virus).
Repeated cases of shingles are typical for patients with HIV infection or oncological diseases (leukemia, lung cancer). In this case, the localization of the rash may correspond to the localization of the tumor, so repeated shingles is considered a signal for an in-depth examination of the patient. In the pathology of shingles, a significant place is occupied by eye damage (keratitis), which determines the severity of the disease and serves as the reason for transferring patients to the ophthalmology department.
Stages
Shingles is divided into four periods:
- prodromal (preherpetic neuralgia);
- stage of herpetic eruptions;
- convalescence (after the disappearance of the exanthema);
- residual effects.
 [ 22 ]
[ 22 ]
Forms
Shingles can occur in mild, moderate and severe forms. Abortive or protracted course is possible. The severity criteria are considered to be the severity of intoxication, signs of damage to the central nervous system, the nature of local manifestations (type of exanthema, intensity of pain syndrome).
Herpes of the geniculate ganglion of the facial nerve (Ramsay-Hunt syndrome) develops when the geniculate ganglion of the facial nerve is affected and is characterized by ear pain, facial nerve paralysis, and sometimes vestibular disorders. Vesicular eruptions appear in the external auditory canal; taste may be lost in the anterior third of the tongue.
Ophthalmic herpes is an ocular form of herpes zoster, which develops with damage to the trigeminal ganglion - the Gasserian ganglion, and is characterized by pain and vesicular rashes along the ocular branches of the V nerve, around the eyes. Blisters on the tip of the nose (Hutchinson's symptom) reflect damage to the nasociliary branch of the V nerve. It should be remembered that eye damage can develop in the absence of damage to the tip of the nose.
Oral herpes is uncommon but may cause acute unilateral lesions; prodromal symptoms of herpes zoster are usually absent.
In the structure of clinical manifestations of herpes zoster, a significant place is occupied by various syndromes of damage to the central and peripheral parts of the nervous system.
Sensory disturbances in the area of the rash: radicular pain, paresthesia, segmental disorders of superficial sensitivity are observed constantly. The main symptom is local pain, the intensity of which fluctuates widely. The pain has a pronounced vegetative coloring (burning, paroxysmal, increasing at night). It is often accompanied by emotional and affective reactions.
Radicular paresis is topically confined only to certain areas of rash: lesions of the oculomotor nerves, facial nerve (variants of Hunt syndrome), paresis of the upper limbs, abdominal wall muscles, lower limbs, and the sphincter of the bladder. These symptoms of shingles usually develop on the 6th to 15th day of the disease.
Polyradiculoneuropathy is a very rare syndrome in patients with herpes zoster; only a few dozen cases have been described.
Serous meningitis is one of the main syndromes in the picture of herpes zoster. When examining the cerebrospinal fluid in the early stages, two- or three-digit lymphocytic or mixed pleocytosis is detected, including in the absence of general cerebral and meningeal phenomena (clinically "asymptomatic" meningitis).
Encephalitis and meningoencephalitis are observed in the acute period. Signs of CNS damage appear on the 2nd-8th day of rashes in the dermatome. CT allows to detect foci of destruction of brain tissue already from the 5th day of encephalitis.
Diagnostics shingles
It is difficult to recognize herpes zoster in the prodromal period, but after the appearance of characteristic rashes, diagnosis is not difficult. Herpes zoster diagnosis is based on the recognition of a typical rash. If the diagnosis is doubtful, a Tzanck test can be performed to detect multinucleated giant cells. Sometimes the herpes simplex virus can cause almost the same lesions as herpes zoster. However, herpes simplex usually relapses, while herpes zoster rarely relapses, the rashes are located along the dermatomes. Viruses can be identified by culturing and analyzing biopsy material.
Laboratory confirmation of diagnosis involves detection of the virus antigen by microscopy or by the immunofluorescence method, serological diagnostics of herpes zoster. PCR is promising.
What do need to examine?
What tests are needed?
Differential diagnosis
Diagnosis of herpes zoster in the vast majority of cases does not cause difficulties. The leading position is retained by clinical criteria, the main of which is considered to be the presence of a characteristic exanthema with a peculiar segmental topography, almost always one-sided.
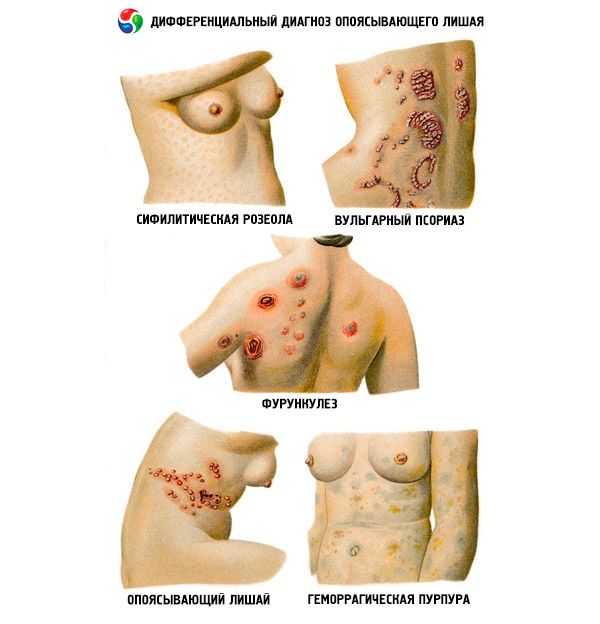
In some cases, differential diagnostics of herpes zoster is carried out with zosteriform herpes simplex. The bullous form of herpes zoster is differentiated from erysipelas, skin lesions in oncological, hematological diseases, diabetes mellitus and HIV infection.
Who to contact?
Treatment shingles
Patients with severe herpes zoster are hospitalized. Patients with a generalized form of the infectious process, damage to the first branch of the trigeminal nerve and the central nervous system require mandatory hospitalization.
Herpes zoster is treated with local sedatives, such as wet compresses, and sometimes systemic analgesics. Antiviral drugs can reduce the severity and frequency of acute rashes and the incidence of serious complications in immunocompromised individuals and pregnant women. Treatment of herpes zoster should begin as early as possible, ideally in the prodromal period; it is ineffective if started later than 72 hours after the first rash appears. Famciclovir 500 mg orally 3 times daily for 7 days and valacyclovir 1 g orally 3 times daily for 7 days are used: these drugs have better bioavailability than orally administered acyclovir (at a dose of 800 mg 5 times daily for 7-10 days) and are therefore preferable. Glucocorticoids help speed up recovery and relieve acute pain, but do not reduce the incidence of postherpetic neuralgia.
In immunocompromised patients, it is recommended to administer acyclovir at a dose of 10 mg/kg intravenously every 8 hours for 7 days for adults and 500 mg/m2 intravenously every 8 hours for 7-10 days for children over 1 year old.
Prevention of primary infection is carried out by vaccinating children and susceptible individuals. A pronounced booster effect of the vaccine has been shown in elderly individuals who have previously suffered from chickenpox (a decrease in the number of cases of the disease).
Treatment of postherpetic neuralgia can be difficult. Gabapentin, cyclic antidepressants, and topical lidocaine or capsaicin ointments are used. Occasionally, opioid analgesics may be needed. Intrathecal methylprednisolone is sometimes effective.
Pathogenetic treatment of herpes zoster involves the administration of dipyridamole as a disaggregant, 50 mg 3 times a day, for 5-7 days. Dehydration treatment of herpes zoster is indicated (acetazolamide, furosemide). It is advisable to prescribe immunomodulators (prodigiosan, imunofan, azoximer bromide, etc.).
In case of postherpetic neuralgia, NSAIDs (indomethacin, diclofenac, etc.) are used in combination with analgesics, sedatives and physiotherapy. Vitamin therapy is possible (B1, B6, B12), it is preferable to carry out it with a lipophilic modification of vitamins - milgamma "N", which has a higher bioavailability.
In severe cases with severe intoxication, detoxification treatment of shingles is carried out with intravenous administration of rheopolyglucin, infucol, dehydration is increased, anticoagulants and corticosteroid hormones are used in small doses. Locally - 1% solution of brilliant green, 5-10% solution of potassium permanganate, in the crust phase - 5% bismuth subgallate ointment; in sluggish processes - methyluracil ointment, solcoseryl. Antibiotics are prescribed only to patients with shingles with signs of activation of bacterial flora.
In general, the therapeutic strategy is determined by the stage and severity of the process, the characteristics of the clinical course of herpes zoster, the general condition and age of the patient.
When treating ophthalmic herpes, a consultation with an ophthalmologist is necessary; for ear herpes, an otolaryngologist is necessary.
Approximate periods of incapacity for work
7-10 days.
Clinical examination
Outpatient observation in case of severe course of the disease and presence of complications for 3-6 months.
 [ 30 ], [ 31 ], [ 32 ], [ 33 ]
[ 30 ], [ 31 ], [ 32 ], [ 33 ]
Patient information sheet
You should avoid hypothermia and other stressful conditions, limit physical activity, eat a balanced diet. It is also necessary to check the state of the immune system.

