Medical expert of the article
New publications
Rhinoviruses
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Rhinoviruses are viruses that contain ribonucleic acid. They are the most common causative agents of acute respiratory viral infections. Rhinoviruses are the culprits of rhinitis, pharyngitis and bronchitis. Very rarely, rhinoviruses cause more serious respiratory tract damage. However, there are cases when they cause bronchial asthma in a child or chronic bronchitis in an adult, can lead to otitis media and sinusitis; they can also aggravate asthma, cystic fibrosis.
Causes rhinovirus infection
Rhinoviruses (RV) are members of the Picornaviridae family. There are over 100 different subtypes in 3 main groups, classified according to receptor specificity: intercellular adhesion molecule-1 (ICAM-1), low-density lipoprotein receptor, and cellular sialoprotein receptors.
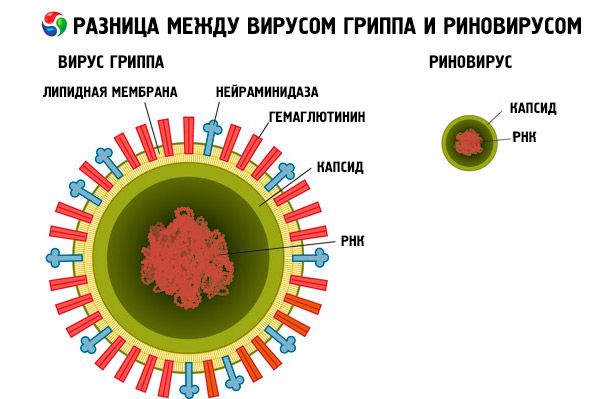
Science knows more than a thousand serotypes of rhinoviruses. Despite such diversity, the structure of the virus is very simple - it contains only ten genes, while humans have more than 20,000 genes. The icosahedral capsid is 12 pentamers, contains 4 viral proteins.
However, such a primitive structure of the rhinovirus does not prevent it from confusing the immune system and infecting a person. This type of virus is very common. In areas with a moderate climate, epidemiological outbreaks of diseases caused by rhinoviruses are often recorded in early autumn and spring. Isolated cases are observed constantly, regardless of the time of year. In the tropics, the maximum number of cases is recorded during the rainy season.
Risk factors
- Smoking increases the risk of respiratory infections by about 50%.
- Newborns and older people are at risk, possibly due to decreased immunity.
- Failure to comply with personal hygiene rules.
- Anatomical, metabolic, genetic, and immunologic disorders (eg, tracheoesophageal fistula, congenital heart defects, cystic fibrosis, or immunodeficiency) increase the risk and severity of infection.
Pathogenesis
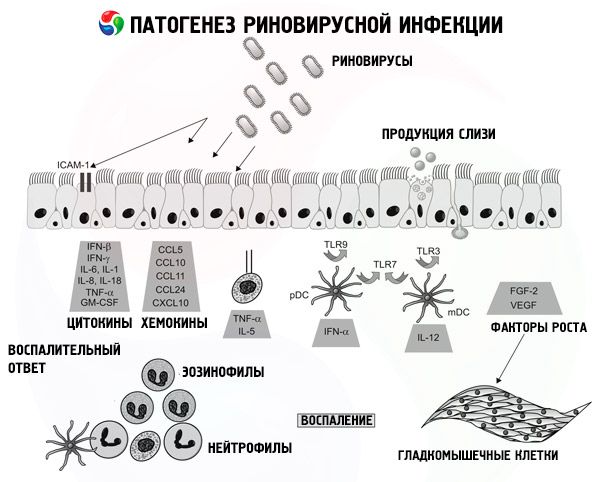
Rhinoviruses have different transmission mechanisms. Most often - direct contact or aerosol route. The entry gates are the nasal mucosa and conjunctiva. The main receptor for interaction in the human body with rhinoviruses is ICAM-1, which is found in large quantities in the posterior nasopharynx. Contrary to popular belief, kissing, normal conversation, coughing do not contribute to the spread of the disease.
Rhinoviruses are resistant to cold, but die from heat, lack of moisture and antiseptics. You can become infected with the virus through contact with a patient who has rhinovirus in their nasal discharge. Rhinovirus spreads by airborne droplets. The diversity of rhinoviruses ensures their invulnerability. A drug or vaccine that successfully affects the protein shell of a given strain is powerless in the fight against strains that have the same protein but a different structure. And when a virus strain has at least some resistance to the drug, natural selection and mutation will bring about the emergence of strains that will be absolutely resistant to the drug.
Rhinoviruses do not attack many cells and do not cause much harm. So where do such complications come from? The point here is in the peculiarities of the immune defense mechanisms. The affected cells produce special molecules, cytokines, which serve as a signal to launch a cascade of cellular immunity reactions. It is because of them that we feel so unwell. Cytokines are the culprits of inflammation in the throat and abundant mucus secretion. You can feel healthy not at all when the immune system defeats the rhinovirus, but only after the immune system begins to work in normal mode.
Today, doctors do not have any means to effectively combat rhinoviruses. Vaccinations are practically useless. No drug can destroy the virus. The mistake of many is taking antibiotics, which are effective in combating bacteria and are absolutely powerless against viruses. Often, doctors prescribe antibiotics even if they are not sure of the nature of the disease: whether it is a viral or bacterial infection. Careless treatment with antibiotics encourages the development of drug-resistant bacteria.
We greatly underestimate rhinoviruses. They have many types and science is only beginning to comprehend their diversity. At the end of the last century, scientists discovered several dozen strains, which they classified into two large genera. In 2006, scientists in the United States discovered a strain of rhinovirus that did not belong to either of these genera. And then it turned out that this was a representative of another, third genus, which is also very common. In different areas, the genes of rhinovirus strains are almost identical. This fact serves as evidence of the very rapid spread of this third genus, which was called HRV-C.
Rhinoviruses have a genetic core that changes very little. However, some viral genes change very rapidly. Scientists have found that they are necessary for the survival of rhinoviruses that have entered into battle with the human immune system. After the body has begun to produce antibodies to cope with one strain of the virus, it is still vulnerable to other strains, since these antibodies are powerless against their protein shell. The hypothesis is supported by the fact that every year a person is infected with several different strains of rhinovirus.
Despite these facts, some representatives of the scientific world are optimistic about the future and believe that it is possible to develop a cure for rhinoviruses. Since rhinoviruses have the same genetic core, it can be assumed that it cannot mutate. That is, rhinoviruses whose mutation has affected the core die. When people find a way to influence the core, the disease can be defeated.
But is there any point in doing this? Rhinovirus is dangerous because it opens the way for more dangerous pathogens. However, it is relatively safe. A week later, the infected person already forgets about the symptoms, and 40% of those tested, in whom the tests found rhinovirus, did not even know about it - it did not manifest itself in any way.
Scientists even acknowledge the beneficial effect of rhinovirus on the body. The collected data confirm that children who have had relatively safe viral, including rhinovirus, and bacterial infections are less susceptible to immune disorders in adulthood. Rhinovirus, one might say, trains the immune system so that it does not react too actively to minor threats, but is able to concentrate on truly serious dangers. Therefore, it is worth thinking about and, perhaps, changing the view of rhinoviruses: to look at them not as enemies, but as wise trainers.
Symptoms rhinovirus infection
The incubation period ranges from 12-72 hours to 7-11 days.
Symptoms of rhinovirus infection are similar to those of a common cold. The infection develops asymptomatically for 2-4 days, and then severe rhinitis with severe nasal discharge and pharyngitis with no symptoms of toxic damage appears. In some cases, the vessels of the conjunctiva and eye membranes are affected.
Headaches, body aches and other disorders typical of the flu are less pronounced with ARVI. Body temperature does not rise as often and is not as high as with the flu or adenovirus infection. After two or three days, the symptoms become less pronounced, but persist for up to a week.
Other symptoms of rhinoviruses:
- Dryness or irritation in the nasal cavity.
- Nasal congestion, sneezing.
- Annoying dry cough.
- Hoarseness of voice.
- Profuse nasal discharge, watery or mucopurulent (yellow or green).
- Painless enlargement of the lymph nodes.
Complete recovery from rhinovirus in young children may occur even later – after 14 days.
Colds and rhinovirus infections may increase stroke risk in children. The findings of a study by Hills and colleagues from Northern California conducted between 1993 and 2007, which included about 2.5 million children, showed a significant impact of colds and upper respiratory infections in the first 3 days of illness on the risk of stroke in children.
Diagnostics rhinovirus infection
An accurate diagnosis can be established using laboratory diagnostic methods, when rhinovirus is cultivated on human cell cultures. Immunofluorescence is also used, which detects antigen in particles of the nasal mucosa epithelium. The most accurate diagnosis is provided by a neutralization reaction with paired blood serums.
Treatment rhinovirus infection
Rhinovirus infections are relatively harmless and resolve quickly, so treatment focuses on relieving symptoms and taking steps to prevent the virus from spreading.
The basis of treatment is rest, drinking plenty of fluids, and taking medications that will ease the painful condition. It is necessary to maintain a comfortable temperature and humidity in the room. This will help soothe the irritated nasopharynx and make breathing easier. Alcohol and smoking should be excluded during the illness.
It is impossible to defeat the virus with the help of one drug, but if you use complex treatment, you can help the body cope with rhinovirus infection faster.
Since the clinical picture of rhinovirus infection is very similar to the manifestations of other types of ARVI, broad-spectrum antiviral drugs are most often used. Targeted drugs make sense to use only after the diagnosis has been confirmed. All respiratory tract infections caused by viruses (rhinoviruses, influenza, parainfluenza, adenoviruses, enteroviruses or coronaviruses) are treated according to the same algorithm.
1. Taking antiviral drugs:
- Arbidol (stops the penetration of viruses into epithelial cells). It can be taken from the age of two. Children under 6 are prescribed 2 tablets per day, from 6 to 12 years old take 4 tablets, adults - 8 tablets. The course of therapy is 5 days;
- Isoprinosine - the recommended daily dose is 50 mg/kg. It should be divided into 2-3 doses. The course of taking the drug should last at least 5 days;
- Lokferon, Bonafton, Oxolinic ointment - these drugs are intended for local use. They inhibit the activity of viruses and are administered intranasally;
- Ribavirin - the course of treatment is 5-7 days. It is prescribed from 12 years old in a dosage of 10 mg/kg.
2. Taking immunomodulators that inhibit the reproduction of viruses and stimulate the body’s immune response.
- Interferon-α is started with 5 drops every half hour for 4 hours. Then the number of doses is reduced to 5 times a day. The course of treatment is 5-7 days;
- Viferon in suppositories - administered 2 times a day.
3. Taking immunostimulants.
- Cycloferon. From 4 years old, one tablet is prescribed per day, from 7 to 11 years old - 2 tablets, adults take 3 tablets;
- Anaferon can be taken even by the smallest. It is prescribed to children who have reached 6 months of age: 4 tablets on the first day, then 1 tablet 3 times a day for 5 days.
4. Elimination of disease symptoms:
- taking antipyretic drugs (Nurofen, Paracetamol);
- taking cough medicine. When prescribing a medicine, the doctor takes into account the nature of the cough and the place where it is localized;
- to make breathing easier, rinse the nose with Aqua Maris, Humer or a hypertonic solution;
- To eliminate swelling, Pinosol or Xylen are dripped intranasally.


 [
[