Medical expert of the article
New publications
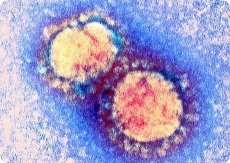
Respiratory syncytial virus (RS virus)
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The RS virus is one of the most common pathogens of ARI in children in the first 2-3 years of life. It was first isolated in 1956 from a chimpanzee suffering from ARI, and in 1957 R. Chenok (et al.) isolated similar strains from children suffering from ARI.
The virion is spherical, its diameter varies in individual particles from 120 to 200 nm. The genome is represented by single-stranded non-fragmented negative RNA with m. w. about 5.6 MD; it apparently carries 10 genes encoding 10 virus-specific proteins, 7 of which are part of the virion, and the rest are non-structural. RS virus differs from other paramyxoviruses in that it does not have hemagglutinin and neuraminidase, and it does not have hemolytic activity. The genome structure is as follows: 3'-lC-lB-NPM-lA-GF-22K-L-5'. Proteins G and F are glycoproteins that are part of the supercapsid and form surface spikes. Protein G ensures fixation of the virus on sensitive cells, and protein F ensures fusion of two types: a) fusion of the viral membrane with the cell membrane and its lysosomes; b) fusion of the infected cell with adjacent uninfected cells, resulting in the formation of a syncytium - a symplast of cells connected to each other by cytoplasmic processes ("reticular tissue"). This phenomenon served as the basis for calling the virus "respiratory syncytial". Proteins N, P and L (polymerase complex containing transcriptase) are part of the nucleocapsid. Proteins M and K are associated with the inner surface of the virion supercapsid. The functions of the remaining proteins are still unknown. According to antigenic properties, two serovariants of the virus are distinguished. The virus reproduces well in cultures of many strains of transplantable cells (HeLa, HEp-2, etc.) with the manifestation of a characteristic cytopathic effect, as well as with the formation of plaques; it is not cultivated on chicken embryos. The RS virus is very labile and is easily destroyed by freezing and thawing, when treated with fat solvents, detergents, and various disinfectants; when heated to 55 °C it dies in 5-10 minutes.
Symptoms of respiratory syncytial infection
The source of infection is a sick person. Infection occurs through airborne droplets. The incubation period is 3-5 days. The virus multiplies in the epithelial cells of the respiratory tract, the process quickly spreads to their lower sections. Respiratory syncytial infection is especially severe in children of the first six months of life in the form of bronchitis, bronchiolitis, pneumonia. Antibodies to the virus are found in 75% of three-year-old children.
Post-infection immunity is stable and long-lasting; it is caused by the appearance of virus-neutralizing antibodies, immune memory cells, and secretory antibodies of the IgAs class.
Diagnosis of respiratory syncytial infection
Laboratory diagnostics of respiratory syncytial infection is based on rapid detection of viral antigens in nasopharyngeal discharge (in deceased individuals, tissues of the lungs, trachea, and bronchi are examined) using the immunofluorescence method, isolation and identification of the virus, and determination of specific antibodies. To isolate the virus, cell cultures are infected with the test material, and its reproduction is judged by the characteristic cytopathic effect; the virus is identified using the immunofluorescence method, CSF, and the neutralization reaction in cell culture. The serological method (CSF, RN) is not reliable enough in children of the first six months of life who have maternal antibodies in a titer of up to 1:320. To diagnose the disease in them, it is better to use methods for detecting specific antigens using RIF or IFM.


 [
[