Medical expert of the article
New publications
Investigation of the autonomic nervous system
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

In many cases, a thorough analysis of the patient's complaints and anamnestic information about the function of the genitourinary sphere and rectum, the presence of increased sweating, imperative urges to urinate, urinary incontinence and erectile dysfunction (in men) is sufficient to assess the vegetative functions. A more detailed study of the vegetative nervous system is advisable in patients presenting the corresponding complaints, as well as in a number of polyneuropathies.
Blood pressure, heart rate
- The orthostatic test is designed to assess the participation of the sympathetic nervous system in the vegetative support of activity. Blood pressure and heart rate (HR) are measured with the patient lying down and then standing. Blood pressure and HR are measured again 3 minutes after assuming a vertical position. With normal vegetative support of activity, HR (by 30 per minute) and systolic blood pressure (by 20 mm Hg) increase immediately upon transition to a vertical position, while diastolic blood pressure changes little. While standing, HR may increase by 40 per minute, and systolic blood pressure may decrease by 15 mm Hg below the initial level or remain unchanged; diastolic blood pressure does not change or slightly increases compared to the initial level. Insufficient autonomic support is diagnosed if an orthostatic test shows a drop in systolic blood pressure of 10 mm Hg or more immediately after moving to a vertical position or by 15 mm Hg or more while standing. In this case, one should assume insufficiency of the sympathetic nervous system and the probability of orthostatic arterial hypotension. Excessive autonomic support is diagnosed if systolic blood pressure rises immediately after moving to a vertical position by more than 20 mm Hg; or if the heart rate increases by more than 30 per minute; or if only an isolated rise in diastolic blood pressure is observed.

- The fist squeeze test is also used to assess the vegetative support of activity. The patient squeezes the fist for 3 minutes with a force equal to 30% of the maximum possible (determined by a dynamometer). Normally, diastolic arterial pressure increases by 15 mm Hg or more. In case of vegetative insufficiency, such an increase does not occur.
- The deep breathing test evaluates the parasympathetic nervous system. The patient is asked to breathe deeply and infrequently (6 breaths per minute). Deep, infrequent breathing in a healthy person slows the pulse by at least 15 per minute. A slowdown of less than 10 per minute indicates a decrease in the activity of the vagus nerve system.
- The eyeball pressure test (Dagnini-Ashner) allows one to evaluate the reactivity of the parasympathetic nervous system. Using the pads of your fingers, press on the eyeballs of the patient lying on his back until he feels a slight pain. Continue the effect for 6-10 seconds. Normally, by the end of the test, the patient's pulse slows down by 6-12 per minute. A more pronounced slowing (vagal reaction) indicates increased vegetative reactivity, a less pronounced one - decreased vegetative reactivity. The absence of a reaction or a paradoxical increase in pulse rate (perverted vegetative reactivity) indicates the predominance of the tone of the sympathetic nervous system.

Sweating
To assess sweating, palpate the skin. In doubtful cases, you can resort to the iodine-starch test. The patient's skin is lubricated with a solution of iodine in a mixture of ethyl alcohol and castor oil (iodine - 1.5; castor oil - 10; ethyl alcohol - 90). A few minutes after drying, the skin is evenly sprinkled with starch powder. Then, artificially induce sweating in the patient (1 acetylsalicylic acid orally and a glass of hot tea). In places where sweat is secreted, a reaction of starch with iodine occurs and an intense dark purple coloration occurs. Zones where sweating is absent remain uncolored.

Urination
If the patient complains of urination, first of all, his abdomen is palpated. In some cases, this will allow to detect a distended, overfilled bladder. The nature of urination disorders is usually clarified based on the results of instrumental urodynamic examination (cystomanometry, uroflowmetry ).
Frontal lobe damage, especially bilateral, leads to a decrease in descending inhibitory influences on the spinal urination center, which is manifested by imperative urges to urinate and urinary incontinence (central uninhibited bladder). Bladder sensitivity and the sensation of its filling are preserved, the function of the bladder sphincters is not impaired, since its spinal innervation is intact. Central uninhibited bladder is typical for elderly people and also occurs with diffuse brain damage. Cognitive disorders contribute to urination disorders.
Acute spinal cord injury above the sacral segments (spinal cord injury) causes spinal shock, in which detrusor function is inhibited and the bladder becomes overfilled. "Overflow incontinence" may occur. Then, as spasticity develops in the legs, the detrusor also becomes "spastic" (hyperactive) due to the loss of suprasegmental inhibitory control and the release of the intact sacral segments and their local reflex arcs. A suprasacral bladder, or automatic reflex bladder, is formed, which is not subject to voluntary control, functions automatically (the detrusor contracts reflexively in response to filling), and is manifested by imperative urinary incontinence. The feeling of bladder fullness and its sensitivity during urination are reduced or lost, since the ascending sensory pathways in the spinal cord are interrupted.
Damage to the parasympathetic neurons of the sacral segments (S2 - S3 ) or their axons (trauma, radiculomyeloischemia, meningomyelocele) leads to the development of atony of the bladder, while bladder sensitivity may be preserved (infrasacral bladder, motor paralytic bladder). Urinary retention occurs, the bladder overflows with urine. In this case, "incontinence from overflow", or paradoxical urinary incontinence (ischuria paradoxa) is possible: there are signs of both urinary retention (the bladder is constantly overflowing and does not empty on its own) and incontinence (urine constantly flows out drop by drop due to mechanical overstretching of the external sphincter). The constant presence of a significant amount of residual urine in the bladder is accompanied by a high risk of developing a urinary tract infection.
Damage to the peripheral nerves that innervate the bladder or to the posterior spinal roots leads to its deafferentation. It loses sensitivity and becomes atonic (peripheral extramedullary bladder, sensory paralytic bladder). This form of the bladder is typical for diabetic autonomic polyneuropathy, tabes dorsalis. The feeling of bladder filling is lost and the bladder emptying reflex disappears, as a result of which it overflows. Overflow incontinence occurs. The constant presence of residual urine in the bladder is associated with a high risk of urinary tract infection.
The "autonomous" bladder is completely deprived of any innervation (secondary damage to the intramural bladder ganglia during prolonged stretching of the bladder walls). In this case, the intramural reflex is switched off, which closes at the level of the bladder wall and is the basis for the excitation of more complex reflexes. Sensory information about the bladder in such cases is absent, and efferent impulses are not perceived by the bladder wall, which is manifested by bladder atony and urinary retention.
Meningeal syndrome
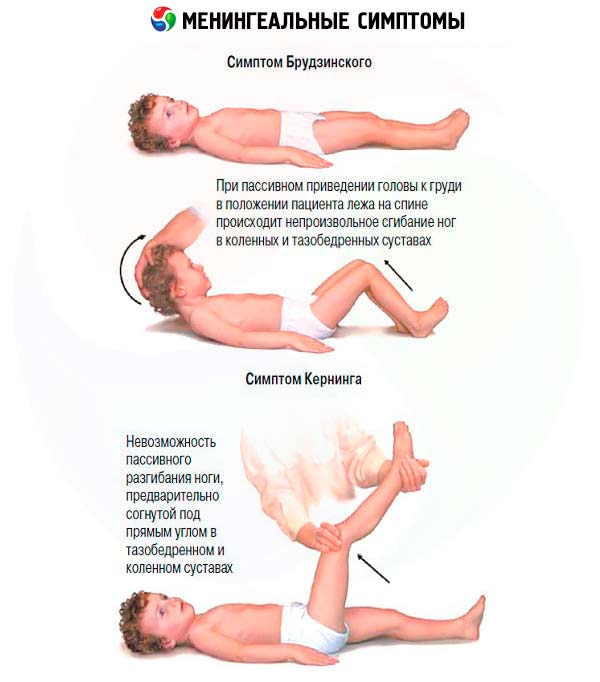
Meningeal symptoms appear with inflammation of the meninges ( meningitis ), with their irritation by spilled blood ( subarachnoid hemorrhage ), less often - with exogenous or endogenous intoxication and increased intracranial pressure (with brain tumors). The most informative meningeal signs include stiffness of the occipital muscles, Kernig's symptom, Brudzinsky's symptoms. All meningeal symptoms are examined with the patient lying on his back.
- To detect stiffness of the occipital muscles, the doctor places the back of the patient's head on his hand and waits until the neck muscles relax. Then he carefully bends the patient's neck, bringing the chin closer to the chest. Normally, with passive flexion of the neck, the chin touches the chest; with irritation of the meninges, there is tension in the neck muscles and the chin does not reach the chest. It should be remembered that the limitation of the range of motion in the cervical spine can be caused by arthrosis of the facet joints of the cervical vertebrae (spondyloarthrosis). However, with spondyloarthrosis, neck flexion is not so significantly impaired and at the same time, lateral rotation of the neck is significantly limited, which is not typical for meningeal irritation syndrome. Severe stiffness of the neck muscles is also possible with Parkinson's disease, but if you continue to gently apply pressure to the back of the head, the neck can be bent to its full extent, although the patient may experience slight discomfort.
- Kernig's Symptom: the patient's leg is bent at a right angle at the hip and knee joints, then straightened at the knee joint. When the meninges are irritated, tension in the flexor muscles of the lower leg is felt, which makes it impossible to straighten the leg.
- Brudzinski's symptoms: when attempting to passively tilt the patient's head toward the chest, flexion occurs in the hip and knee joints (upper Brudzinski's symptom); a similar movement of the lower limbs is also caused by pressure on the pubic symphysis (middle Brudzinski's symptom); a similar flexion movement in the contralateral lower limb occurs when performing the Kernig test (lower Brudzinski's symptom).


 [
[