Medical expert of the article
New publications
Rheumatic polymyalgia
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Polymyalgia rheumatica (PMR) is a rheumatic disorder characterized by pain and stiffness in the neck, shoulders, and hips. The disorder is more common in adults over 50 years of age. It is an inflammatory condition associated with elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Giant cell arteritis (GCA) may coexist with and/or develop in patients with polymyalgia rheumatica. Some authors consider giant cell arteritis to be an extreme manifestation of the same disease spectrum as polymyalgia rheumatica. The challenges in managing PMR include proper diagnosis of the condition and appropriate treatment, which requires a long-term follow-up period. This article reviews the causes, pathophysiology, and manifestations of polymyalgia rheumatica. [ 1 ]
Epidemiology
The annual incidence of polymyalgia rheumatica per 100,000 population aged 50 years or older has been found to be between 58 and 96 in predominantly white populations. Incidence rates increase with age up to 80 years.[ 2 ],[ 3 ] PMR is considered the second most common inflammatory autoimmune rheumatic disease after rheumatoid arthritis in some predominantly white populations. Polymyalgia rheumatica is much less common in black, Asian, and Hispanic populations.
Causes rheumatic polymyalgia
The etiology of polymyalgia rheumatica is not well understood.
Familial aggregation of PMR suggests a genetic predisposition.[ 4 ] HLA class II alleles are associated with PMR, and among them the most frequently correlated allele is HLA-DRB1*04, observed in up to 67% of cases.[ 5 ] Genetic polymorphisms of ICAM-1, RANTES and IL-1 receptors also appear to play a role in the pathogenesis of PMR in some populations.[ 6 ]
There have been reports of increased incidence of PMR along with GCA during mycoplasma pneumonia and parvovirus B19 epidemics in Denmark, suggesting a possible role of infection in the etiopathogenesis.[ 7 ] Epstein-Barr virus (EBV) has also been suggested as a possible trigger for polymyalgia rheumatica.[ 8 ] However, several other studies have not supported the infectious etiology hypothesis.[ 9 ],[ 10 ]
There are also reports of an association between PMR and diverticulitis, which may suggest a role for altered microbiota and chronic intestinal inflammation in the immunopathogenesis of the disease.[ 11 ]
There is also a case series of previously healthy patients who developed GCA/PMR after influenza vaccination.[ 12 ] Vaccine adjuvants can induce autoimmune reactions causing adjuvant-induced autoimmune/inflammatory syndrome (ASIA), which can have clinical features similar to polymyalgia rheumatica.
Pathogenesis
Polymyalgia rheumatica is an immune-mediated disease and elevated inflammatory markers are one of the most common features. IL-6 appears to play a central role in mediating inflammation.[ 13 ] Interferon (IFN) may be present in temporal artery biopsy in patients with GCA but not in patients with PMR, suggesting its role in the development of arteritis.[ 14 ] Elevated IgG4 levels were found in patients with PMR but less frequently in patients with GCA.[ 15 ] The same study found an increased number of patients with features of polymyalgia rheumatica and without elevated IgG4 levels who also had GCA.
Patients with polymyalgia rheumatica have lower numbers of circulating B cells compared to healthy adults. The number of circulating B cells is inversely correlated with ESR and CRP. This altered B cell distribution may contribute to the IL-6 response in PMR.[ 16 ] Autoantibodies, which play an important role in the pathogenesis, are not a feature of polymyalgia rheumatica. Patients with PMR have decreased numbers of Treg and Th1 cells and increased numbers of TH 17 cells.[ 17 ] Increased expression of toll-like receptors 7 and 9 in peripheral blood monocytes also suggests a role for innate immunity in the pathogenesis.[ 18 ]
Symptoms rheumatic polymyalgia
Polymyalgia rheumatica is characterized by symmetrical pain and stiffness in and around the shoulders, neck, and hip girdle. The pain and stiffness are worse in the morning and also worse after rest or prolonged inactivity. Limited range of motion of the shoulder is common. Patients often complain of pain and stiffness in the forearms, hips, thighs, upper and lower back. Symptoms come on quickly, usually within a day to 2 weeks. This affects quality of life, as the pain can interfere with nighttime sleep and daily routine activities such as getting out of bed or a chair, showering, combing hair, driving, etc.
The pain and stiffness associated with polymyalgia rheumatica are most likely due to inflammation of the shoulder and hip joints and, in the upper extremity, the subacromial, subdeltoid, and trochanteric bursae.[ 19 ] Almost half of patients experience systemic symptoms such as fatigue, malaise, anorexia, weight loss, or low-grade fever.[ 20 ] Persistent high fever is uncommon in polymyalgia rheumatica and should raise suspicion of giant cell arteritis.[ 21 ]
Peripheral involvement is also common in arthritis, occurring in up to a quarter of patients. Other peripheral features such as carpal tunnel syndrome, distal limb swelling with pitting edema, and distal tenosynovitis may be present. Arthritis does not lead to erosions, deformities, or the development of rheumatoid arthritis.[ 22 ] Distal limb swelling with pitting edema responds rapidly to glucocorticoids.[ 23 ]
On physical examination, diffuse tenderness is usually present across the shoulder without localization to specific structures. Pain usually limits the active range of motion of the shoulder, and passive range of motion may be normal with careful examination. Limitation of neck and hip motion due to pain is also common. Muscle tenderness of the neck, arms, and thighs may be present. Even though the patient may complain of nonspecific weakness, muscle strength is usually normal with closer examination.
Giant cell arteritis and polymyalgia rheumatica
PMR and GCA are often comorbid, and 20% of patients with PMR will have a later diagnosis of GCA. In biopsy-proven giant cell arteritis, features of polymyalgia rheumatica are present in up to 50% of cases.
In a study of patients with polymyalgia rheumatica with persistence of classic symptoms but without cranial GCA-like symptoms, PET/CT scans were positive for large vessel vasculitis in 60.7%. Inflammatory pain in the lumbar region, pelvic girdle, and diffuse lower extremity pain were also predictors of a positive PET/CT scan in these patients.[ 24 ] In another study, among patients who required higher doses of steroids or those with atypical features such as low-grade fever and weight loss among others, 48% had large vessel vasculitis on PET/CT. Elevated CRP values were found to correlate with large vessel vasculitis.[ 25 ]
In a study in which a random sample of 68 patients with "pure" polymyalgia rheumatica was selected, histological examination of temporal artery biopsies revealed inflammatory changes in only three patients (4.4%).[ 26 ]
Patients with polymyalgia rheumatica should be evaluated for signs suggestive of giant cell arteritis at each visit. Routine temporal artery biopsy is not recommended. Signs such as new headache, visual and jaw symptoms, temporal artery tenderness and pulselessness, peripheral pulselessness, persistent inflammatory markers, high fever, and refractoriness of classic symptoms are red flags that should prompt urgent evaluation for giant cell arteritis.
Forms
2012 Preliminary classification criteria for polymyalgia rheumatica: a joint initiative of the European League Against Rheumatism/American College of Rheumatology [30]
Patients aged 50 years or older with bilateral shoulder pain and abnormal C-reactive protein or ESR concentrations plus at least four points (without ultrasound) or five points or more (with ultrasound):
- Morning stiffness lasting more than 45 minutes (two points).
- Hip pain or limited range of motion (one point).
- Absence of rheumatoid factor or antibodies to citrullinated protein (two points).
- No other concomitant disease (one point).
- If ultrasound is available, at least one shoulder with subdeltoid bursitis, biceps tenosynovitis, or brachial synovitis (posterior or axillary); and at least one hip with synovitis or trochanteric bursitis (one point).
- If ultrasound is available, both shoulders with subdeltoid bursitis, biceps tenosynovitis, or brachial synovitis (one point).
"A score of 4 had 68% sensitivity and 78% specificity for distinguishing all comparable subjects from polymyalgia rheumatica. Specificity was higher (88%) for distinguishing shoulder conditions from PMR and lower (65%) for differentiating rheumatoid arthritis from polymyalgia rheumatica. The addition of ultrasound, a score of 5, increased sensitivity to 66% and specificity to 81%. These criteria are not intended for diagnostic purposes." [ 27 ]
Complications and consequences
Patients with polymyalgia rheumatica have an increased risk of cardiovascular disease ranging from 1.15 to 2.70 according to various studies. Premature atherosclerosis as a result of chronic inflammation is the most likely cause of premature CAD. [ 28 ]
The association of cancer with polymyalgia rheumatica is not entirely clear.[ 29 ] In a study of increased risk of lymphoplasmacytic lymphoma, Waldenstrom's macroglobulinemia was associated with polymyalgia rheumatica with an OR of 2.9.[ 30 ]
Patients with polymyalgia rheumatica have a higher chance of developing inflammatory arthritis. Features of small joint synovitis, younger age, and positive anti-CCP positivity in patients with PMR have been found to be associated with the risk of developing inflammatory arthritis.[ 31 ]
Diagnostics rheumatic polymyalgia
The diagnosis of rheumatic polymyalgia is possible only after excluding other diseases that occur with similar clinical and laboratory signs (oncopathology, rheumatoid arthritis, etc.).
Laboratory research
Elevated ESR is a common feature of polymyalgia rheumatica. ESR above 40 mm is considered significant by most authors. [ 32 ], [ 33 ] ESR below 40 mm/h is present in 7-20% of patients. Patients with low ESR are usually less likely to have systemic symptoms such as fever, weight loss, and anemia. The response to therapy, relapse rate, and risk of developing giant cell arteritis in these patients are comparable to those with high ESR. [ 34 ], [ 35 ] C-reactive protein is also usually elevated. One study found that CRP is a more sensitive indicator of disease activity and ESR is a better predictor of relapse. [ 36 ]
Normocytic anemia and thrombocytosis may be present. Liver enzymes, especially alkaline phosphatase, are sometimes elevated. Serologic tests such as antinuclear antibodies (ANA), rheumatoid factor (RF), and anti-citrullinated protein antibodies (Anti-CCP AB) are negative. Creatine phosphokinase (CPK) is within normal limits.
Visual studies
- Ultrasound
Ultrasound is useful in diagnosis and treatment monitoring by assessing the extent of subacromial/subdeltoid bursitis, long head of biceps tendosynovitis, and brachial synovitis. In one study, a Power Doppler (PD) signal in the subacromial/subdeltoid bursa was observed in one third of patients with polymyalgia rheumatica. A positive PD signal at diagnosis correlated with an increased recurrence rate, but persistence of PD findings did not correlate with relapses/relapses.[ 37 ] The 2012 ACR/EULAR PMR classification criteria include ultrasound.
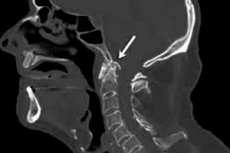
- Magnetic resonance imaging (MRI)
MRI is as helpful in diagnosing bursitis, synovitis, and tenosynovitis as ultrasound, but is more sensitive to findings in the hip and pelvic girdle.[ 38 ] MRI of the pelvis often reveals bilateral peristernal enhancement of the pelvic girdle tendons and occasionally low-grade synovitis of the hip. Enlargement of the proximal origin of the rectus femoris appears to be a highly specific and sensitive finding.[ 39 ]
- Positron emission tomography (PET)
PET scanning shows FDG uptake in the shoulders, ischial tuberosities, greater trochanters, glenohumeral, and sternoclavicular joints in patients with polymyalgia rheumatica.[ 40 ] The role of PET in the diagnosis of large vessel vasculitis is described below in the discussion of giant cell arteritis.
Differential diagnosis
Polymyalgia rheumatica has non-specific features that can mimic many other diseases. Other entities should be excluded from the investigation, if necessary by clinical suspicion, before making a diagnosis of PMR. Some important distinctions are listed below: [ 41 ]
- Rheumatoid arthritis.
- Giant cell arteritis.
- Antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis.
- Inflammatory myositis and statin-induced myopathy.
- Gout and calcium pyrophosphate dihydrate crystal deposition disease (CPPD).
- Fibromyalgia.
- Overuse or degenerative shoulder pathology such as osteoarthritis, rotator cuff tendinitis and tendon rupture, adhesive capsulitis.
- Diseases of the cervical spine, such as osteoarthritis, radiculopathy.
- Hypothyroidism.
- Obstructive sleep apnea.
- Depression.
- Viral infections such as EBV, hepatitis, human immunodeficiency virus, parvovirus B19.
- Systemic bacterial infections, septic arthritis.
- Cancer.
- Diabetes.
Who to contact?
Treatment rheumatic polymyalgia
Oral glucocorticoids (GCs) are a well-established treatment option. The main points of the 2015 EULAR-ACR guidelines for treatment are summarized below: [ 42 ]
- 12.5 to 25 mg/day prednisone equivalent as initial therapy.
- Glucocorticoid levels should be reduced gradually.
- Reduce the dose to 10 mg prednisone equivalent per day over 4-8 weeks.
- Once remission is achieved, reduce daily oral prednisone by 1 mg every 4 weeks until discontinued.
- Minimum 12 months of treatment
- If relapse occurs, increase oral prednisone to the pre-relapse dose and gradually decrease it (over 4-8 weeks) to the dose at which relapse occurred.
- Individualize dose reduction schedules based on regular monitoring of the patient's disease activity, laboratory markers, and adverse events.
- Consider early introduction of methotrexate (MTX) in addition to glucocorticoids, particularly in patients at high risk of relapse and/or on long-term therapy, and in cases with risk factors, comorbidities, and/or concomitant medications where GC-related adverse effects are more likely to occur
Clinical trials have used oral methotrexate at doses of 7.5 to 10 mg weekly. The study shows that leflunomide is an effective steroid-sparing agent that can also be used in polymyalgia rheumatica.[ 43 ] It may be an alternative if the patient cannot take methotrexate for various reasons. There are limited data on azathioprine for the treatment of polymyalgia rheumatica, and its use may be an option in cases with contraindications to methotrexate.[ 44 ] The 2015 EULAR-ACR guidelines do not recommend the use of anti-TNF agents.
Observational series and open-label studies have shown that tocilizumab (TCZ) is useful in polymyalgia rheumatica with relapse or inadequate response to GCs.[ 45 ] An open-label study showed that when used in newly diagnosed patients with polymyalgia rheumatica, relapse-free remission without GC treatment was achievable at 6 months.[ 46 ] Randomized controlled trials are needed to assess whether TCZ routinely provides benefit to some patients with PMR.
Vitamin D and calcium supplements are commonly recommended for patients taking long-term steroids. Bisphosphonate prophylaxis is a recommended option for patients at moderate to high fracture risk, which includes patients over 40 years of age with a FRAX score > 1% and a 10% risk of hip fracture and major osteoporotic fracture, respectively.[ 47 ]
Close follow-up is recommended. Guidelines published by the BSR and BHPR recommend follow-up at weeks 0.1–3 and 6, then at months 3, 6, 9 and 12 in the first year of life (with additional visits for relapses or adverse events). [ 48 ] It seems reasonable to follow patients every 3 months until remission and then every 6 months annually thereafter to monitor for relapse. Relapses often involve rising ESR and CRP and return of symptoms. Increased risk of relapse has been found to correlate with higher initial dose of steroids used, rapid steroid tapering, HLA-DRB1*0401 and persistently high inflammatory markers. [ 49 ], [ 50 ]
Forecast
When diagnosed early and treated appropriately, polymyalgia rheumatica has a favorable prognosis. Mortality among people with polymyalgia rheumatica does not increase significantly compared to the general population.

