Medical expert of the article
New publications
Plasmacytoma
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A disease such as plasmacytoma is of great interest in the field of immunological research, as it is characterized by the production of a huge number of immunoglobulins with a homogeneous structure.
Plasmacytoma refers to malignant tumors composed of plasma cells growing in soft tissues or within the axial skeleton.
Causes plasmacytomas
Doctors still have not fully understood what causes B-lymphocytes to mutate into myeloma cells.
 [ 11 ]
[ 11 ]
Risk factors
The main risk factors for this disease have been identified:
- Older and middle-aged men – plasmacytoma begins to develop when the amount of the male hormone testosterone in the body decreases.
- People under 40 years of age account for only 1% of patients with this disease, so it can be argued that the disease most often affects people after 50 years of age.
- Heredity – about 15% of patients with plasmacytoma grew up in families where relatives had cases of B-lymphocyte mutations.
- People who are overweight – obesity causes a decrease in metabolism, which can lead to the development of this disease.
- Exposure to radioactive substances.
Pathogenesis
Plasmacytoma may occur in any part of the body. Solitary plasmacytoma of bone arises from plasma cells located in the bone marrow, while extramedullary plasmacytoma is thought to arise from plasma cells located on mucous membranes. Both variants of the disease are different groups of neoplasms in terms of location, tumor progression, and overall survival. Some authors consider solitary plasmacytoma of bone to be a marginal cell lymphoma with extensive plasmacytic differentiation.
Cytogenetic studies reveal recurrent losses in chromosome 13, chromosome arm 1p, and chromosome arm 14Q, as well as regions in chromosome arms 19p, 9q, and 1Q. Interleukin 6 (IL-6) remains a major risk factor for the progression of plasma cell disorders.
Some hematologists consider a solitary plasmacytoma of bone as an intermediate stage in the evolution from monoclonal gammopathy of unknown etiology to multiple myeloma.
Symptoms plasmacytomas
In plasmacytoma or myeloma disease, the kidneys, joints and immunity of the patient suffer the most. The main symptoms depend on the stage of the disease. It is noteworthy that in 10% of cases the patient does not notice any unusual symptoms, since the paraprotein is not produced by the cells.
With a small number of malignant cells, plasmacytoma does not manifest itself in any way. But when a critical level of these cells is reached, paraprotein synthesis occurs with the development of the following clinical symptoms:
- Joints ache – painful sensations appear in the bones.
- The tendons hurt – pathological protein is deposited in them, which disrupts the basic functions of the organs and irritates their receptors.
- Pain in the heart area
- Frequent bone fractures.
- Reduced immunity - the body's defenses are suppressed because the bone marrow produces too few leukocytes.
- A large amount of calcium from destroyed bone tissue enters the blood.
- Impaired kidney function.
- Anemia.
- DIC syndrome with development of hypocoagulation.
Forms
There are three distinct groups of the disease defined by the International Myeloma Working Group: solitary plasmacytoma of bone (SPB), extraosseous or extramedullary plasmacytoma (EP), and a multifocal form of multiple myeloma that is either primary or relapsed.
For simplicity, solitary plasmacytomas can be divided into 2 groups depending on location:
- Plasmacytoma of the skeletal system.
- Extramedullary plasmacytoma.
The most common of these is solitary plasmacytoma of bone. It accounts for about 3-5% of all malignant tumors caused by plasma cells. It occurs as lytic lesions within the axial skeleton. Extramedullary plasmacytomas are most often found in the upper respiratory tract (85%), but can be localized in any soft tissue. Paraproteinemia is observed in about half of cases.
Solitary plasmacytoma
Solitary plasmacytoma is a tumor that consists of plasma cells. This bone disease is local, which is its main difference from multiple plasmacytoma. Some patients initially develop solitary myeloma, which can then transform into multiple.
In solitary plasmacytoma, the bone is affected in one area. During laboratory tests, the patient is diagnosed with renal dysfunction and hypercalcemia.
In some cases, the disease progresses completely unnoticed, even without changes in the main clinical indicators. In this case, the prognosis for the patient is more favorable than with multiple myeloma.
 [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ]
[ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ]
Extramedullary plasmacytoma
Extramedullary plasmacytoma is a serious disease in which plasma cells transform into malignant tumors with rapid spread throughout the body. As a rule, such a tumor develops in the bones, although in some cases it can be localized in other tissues of the body. If the tumor affects only plasma cells, then isolated plasmacytoma is diagnosed. In case of numerous plasmacytomas, one can speak of multiple myeloma disease.
Spinal plasmacytoma
Spinal plasmacytoma is characterized by the following symptoms:
- Severe pain in the spine. The pain may increase gradually, simultaneously with the growth of the tumor. In some cases, the pain is localized in one place, in others it radiates to the arms or legs. Such pain does not go away after taking over-the-counter analgesics.
- The patient's sensitivity of the skin of the legs or arms changes. Often there is complete numbness, a tingling sensation, hyper- or hypoesthesia, an increase in body temperature, heat or, conversely, a feeling of cold.
- The patient has difficulty moving. The gait changes, and problems with walking may appear.
- Difficulty urinating and emptying the bowels.
- Anemia, frequent fatigue, weakness throughout the body.
Plasmacytoma of bone
When B-lymphocytes mature in patients with bone plasmacytoma, a failure occurs under the influence of certain factors - instead of plasma cells, a myeloma cell is formed. It has malignant properties. The mutated cell begins to clone itself, which increases the number of myeloma cells. When these cells begin to accumulate, bone plasmacytoma develops.
The myeloma cell is formed in the bone marrow and begins to grow from it. In the bone tissue, it actively divides. As soon as these cells get into the bone tissue, they begin to activate osteoclasts, which destroy it and create voids inside the bones.
The disease progresses slowly. In some cases, it can take up to twenty years from the time of B-lymphocyte mutation until the disease is diagnosed.
Pulmonary plasmacytoma
Plasmacytoma of the lungs is a relatively rare disease. Most often, it affects men aged 50 to 70 years. Typically, atypical plasma cells grow in large bronchi. When diagnosed, clearly defined, rounded, grayish-yellow, homogeneous nodules can be seen.
In pulmonary plasmacytoma, the bone marrow is not affected. Metastases spread hematogenously. Sometimes neighboring lymph nodes are involved in the process. Most often, the disease is asymptomatic, but in rare cases, the following signs are possible:
- Frequent cough with sputum production.
- Painful sensations in the chest area.
- An increase in body temperature to subfebrile levels.
Blood tests do not reveal any changes. Treatment involves surgery to remove the pathological foci.
Diagnostics plasmacytomas
Diagnosis of plasmacytoma is carried out using the following methods:
- An anamnesis is collected - the specialist asks the patient about the nature of the pain, when it appeared, what other symptoms he can identify.
- The doctor examines the patient - at this stage the main signs of plasmacytoma can be identified (the pulse quickens, the skin is pale, there are multiple hematomas, tumor seals on the muscles and bones).
- Conducting a general blood test - in case of myeloma disease the indicators will be as follows:
- ESR – not less than 60 mm per hour.
- Decreased number of erythrocytes, reticulocytes, leukocytes, platelets, monocytes and neutrophils in the blood serum.
- Decreased hemoglobin level (less than 100 g/l).
- A few plasma cells may be detected.
- Conducting a biochemical blood test - in case of plasmacytoma the following will be detected:
- Increased total protein levels (hyperproteinemia).
- Decreased albumin (hypoalbuminemia).
- Increased uric acid.
- Increased levels of calcium in the blood (hypercalcemia).
- Increased creatinine and urea.
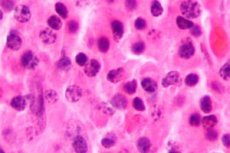
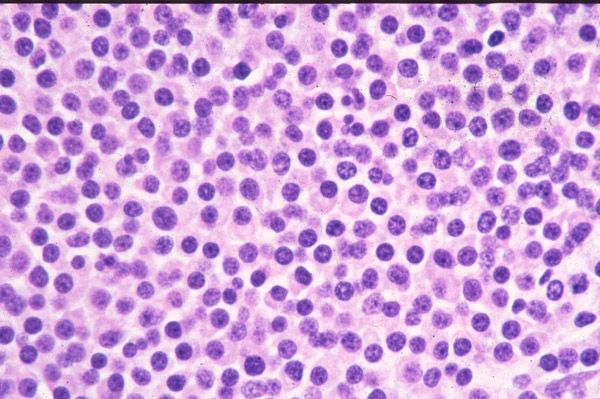
- Conducting a myelogram - the process examines the structure of the cells that are in the bone marrow. A puncture is made in the sternum using a special instrument, from which a small amount of bone marrow is extracted. In case of myeloma, the indicators will be as follows:
- High plasma cell count.
- A large amount of cytoplasm was found in the cells.
- Normal hematopoiesis is suppressed.
- There are immature atypical cells.
- Laboratory markers of plasmacytoma - blood from a vein is taken early in the morning. Sometimes urine can be used. In case of plasmacytoma, paraproteins will be found in the blood.
- Conducting a general urine analysis – determining the physical and chemical characteristics of the patient’s urine.
- Carrying out X-ray examination of bones – with the help of this method it is possible to detect the places of their damage, as well as to make a final diagnosis.
- Conducting a spiral computed tomography - a whole series of X-ray images is taken, thanks to which it is possible to see: where exactly the bones or spine are destroyed and where the deformation occurred, in which soft tissues tumors are present.
Diagnostic criteria for solitary plasmacytoma of bone
The criteria for defining a solitary plasmacytoma of bone vary. Some hematologists include patients with more than one lesion and elevated myeloma protein levels and exclude patients whose disease has progressed for 2 years or who have abnormal protein after radiation therapy. Based on magnetic resonance imaging (MRI), flow cytometry, and polymerase chain reaction (PCR), the following diagnostic criteria are currently used:
- Destruction of bone tissue in one place under the influence of plasma cell clones.
- Bone marrow infiltration with plasma cells is no more than 5% of the total number of nucleated cells.
- Absence of osteolytic lesions of bones or other tissues.
- No anemia, hypercalcemia or renal impairment.
- Low serum or urinary concentrations of monoclonal protein
 [ 30 ], [ 31 ], [ 32 ], [ 33 ]
[ 30 ], [ 31 ], [ 32 ], [ 33 ]
Diagnostic criteria for extramedullary plasmacytoma
- Detection of monoclonal plasma cells by tissue biopsy.
- Bone marrow infiltration with plasma cells is no more than 5% of the total number of nucleated cells.
- Absence of osteolytic lesions of bones or other tissues.
- No hypercalcemia or renal failure.
- Low serum protein M concentration, if present.
Differential diagnosis
Skeletal forms of the disease often progress to multiple myeloma within 2-4 years. Because of their cellular similarities, plasmacytomas must be differentiated from multiple myeloma. SPB and extramedullary plasmacytomas are characterized by the presence of only one lesion location (either bone or soft tissue), normal bone marrow structure (<5% plasma cells), and absent or low levels of paraproteins.
Who to contact?
Treatment plasmacytomas
Plasmacytoma or myeloma disease is treated using several methods:
- Stem cell or bone marrow transplant surgery.
- Conducting chemotherapy.
- Conducting radiation therapy.
- An operation to remove a bone that has been damaged.
Chemotherapy is used for multiple plasmacytoma. As a rule, treatment is carried out using only one drug (monochemotherapy). But in some cases, a complex of several drugs may be needed.
Chemotherapy is a fairly effective method of treating multiple myeloma. 40% of patients achieve complete remission, 50% - partial remission. Unfortunately, many patients experience a relapse of the disease over time.
To eliminate the main symptoms of plasmacytoma, various painkillers are prescribed, as well as procedures:
- Magnetoturbotron – treatment is carried out using a low-frequency magnetic field.
- Electrosleep – treatment is carried out using low-frequency pulsed currents.
In myeloma, it is also necessary to treat concomitant diseases: renal failure and calcium metabolism disorders.
Treatment of solitary plasmacytoma of bone
Most oncologists use approximately 40 Gy for spinal lesions and 45 Gy for other bone lesions. For lesions larger than 5 cm, 50 Gy should be considered.
As reported in the study by Liebross et al., there is no relationship between radiation dose and the disappearance of the monoclonal protein.
Surgery is contraindicated in the absence of structural instability or neurological deficits. Chemotherapy may be considered as the preferred treatment for patients who do not respond to radiation therapy.
Treatment of extramedullary plasmacytoma
Treatment of extramedullary plasmacytoma is based on the radiosensitivity of the tumor.
Combination therapy (surgery and radiation therapy) is the accepted treatment depending on the resectability of the lesion. Combination therapy may provide the best results.
The optimal dose of radiation for local lesions is 40-50 Gy (depending on the size of the tumor) and is administered over 4-6 weeks.
Due to the high rate of damage to the lymph nodes, these areas must also be included in the radiation field.
Chemotherapy may be considered for patients with refractory disease or recurrent plasmacytoma.
Forecast
Complete recovery from plasmacytoma is almost impossible. Only with isolated tumors and timely treatment can we talk about complete recovery. The following methods are used: removal of the bone that was damaged; bone tissue transplantation; stem cell transplantation.
If the patient follows certain conditions, a fairly long remission may occur:
- No severe concomitant diseases were diagnosed with myeloma.
- The patient exhibits high sensitivity to cytostatic drugs.
- No serious side effects were observed during treatment.
With the right treatment of chemotherapy and steroids, remission can last two to four years. In rare cases, patients can live ten years after diagnosis and treatment.
On average, with chemotherapy, 90% of patients survive for more than two years. If no treatment is given, life expectancy will not exceed two years.
 [ 40 ]
[ 40 ]

