Medical expert of the article
New publications
Peripheral neuropathy
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

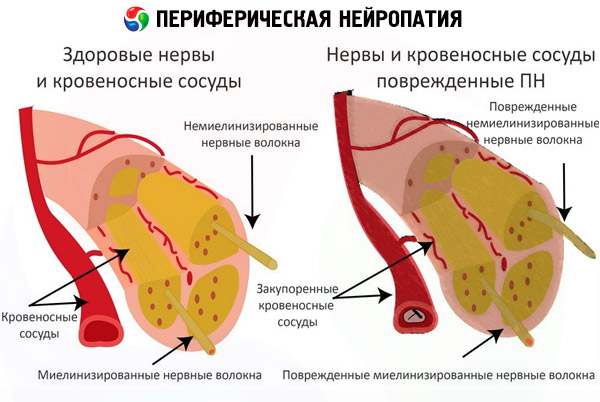
When peripheral nerves are affected, the diagnosis of "peripheral neuropathy" is almost always made; such a disease is often secondary and associated with other painful conditions. With peripheral neuropathy, nerve fibers responsible for the transport of impulses from the central nervous system to the muscles, skin and various organs are damaged.
At the initial stage of neuropathy, the patient may not suspect that he has the disease: for example, peripheral neuropathy of the extremities often begins to manifest itself as tickling or tingling sensations in the fingers or toes. Then the symptoms become more alarming, and only then does the person think about visiting a doctor.
What do you need to know about peripheral neuropathy to identify the problem in time and prevent its further development? All the necessary points can be found in this article.
Epidemiology
Peripheral neuropathy is diagnosed in approximately 2.5% of people. If the disease is detected in childhood and adolescence, then the most common cause is hereditary predisposition. In older patients, peripheral neuropathy is detected in 8% of cases.
The overwhelming majority of patients suffering from peripheral neuropathy are between 35 and 50 years of age.
Causes peripheral neuropathy
Various forms of neuropathy, in essence, begin their development with practically the same causes:
- contusion, nerve laceration;
- damage to nerve fibers by a tumor process;
- critical decrease in immune defense;
- critical vitamin deficiency;
- chronic intoxication, including alcohol;
- vascular diseases, inflammatory changes in the vascular walls;
- diseases of the circulatory system, thrombophlebitis;
- metabolic, endocrine disorders;
- microbial and viral infectious pathologies;
- long-term use of certain medications, such as chemotherapy;
- acute polyradiculoneuritis;
- hereditary peripheral nerve disorder.
Peripheral neuropathy after chemotherapy
The development of neuropathy after chemotherapy is often a side effect of a specific chemotherapy drug. However, this is not always the case: in many patients, the development of peripheral neuropathy after chemotherapy is associated with toxic decay of the tumor process. It is believed that some end products can significantly accelerate the course of the systemic inflammatory process. In such a case, the patient complains of general weakness, sleep disturbance, loss of appetite. In the laboratory, toxic decay of the tumor is reflected in all blood parameters.
Neurotoxic reaction is considered a specific systemic consequence of all chemotherapeutic regimens. Therefore, it is almost impossible to avoid such a consequence: if the dosage of the chemotherapy drug is reduced or canceled altogether, the treatment prognosis worsens significantly. To continue chemotherapy and alleviate the patient's condition, doctors additionally prescribe strong analgesics and anti-inflammatory drugs. Vitamin preparations and immunosuppressants are used as an auxiliary treatment.
Risk factors
Peripheral neuropathy occurs as a result of other factors and diseases, although in some cases the cause cannot be determined.
To date, doctors have voiced almost two hundred factors that can lead to the development of peripheral neuropathy. Among them, the following stand out in particular:
- endocrine disorders, obesity, diabetes;
- long-term exposure to toxic substances (paints, solvents, chemicals, alcohol);
- malignant diseases requiring chemotherapy;
- HIV, viral joint disease, herpes, chickenpox, autoimmune diseases;
- specific vaccination (for example, against rabies, influenza);
- possible traumatic damage to nerves (for example, in road accidents, stab and gunshot wounds, open fractures, prolonged compression);
- chronic hypothermia, vibration;
- long-term treatment with anticonvulsants, antibiotics, cytostatics;
- malnutrition, insufficient intake of B vitamins;
- hereditary predisposition.
Pathogenesis
Peripheral neuropathy is based on a dystrophic degenerative process. That is, nerve fibers are destroyed simultaneously with deterioration of trophism and intoxication.
The membranes of neurons and axons (nerve rods) are subject to destruction.
Peripheral neuropathy affects nerve fibers located outside the brain and spinal cord. Neuropathy of the lower extremities is most often diagnosed, which is associated with a greater length of nerve fibers. These fibers are responsible for general sensitivity, tissue trophism and muscle function.
In many patients, peripheral neuropathy occurs "masked" as other diseases. If the disease is not detected in time, the nerve can be destroyed all the way to the central parts of the nervous system. If this happens, the disorders will become irreversible.
 [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
[ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
Symptoms peripheral neuropathy
The clinical picture of peripheral neuropathy depends on the type of affected nerve fibers. Symptoms may not immediately become apparent: the disease manifests itself on an increasing schedule, worsening over many days, months, and even years.
The main symptom that patients pay attention to is muscle weakness – a person quickly gets tired, for example, when walking or doing physical work. Other symptoms include pain and cramps in the muscles (at the initial stages, cramps often manifest themselves as small twitches of the superficial muscle fibers).
Further, the clinical symptoms expand. Muscular atrophic changes and degenerative processes in bone tissues are observed. The structure of the skin, hair, and nail plates is disrupted. Such disorders are usually caused by damage to sensory or vegetative fibers.
Damage to sensory nerves is characterized by a number of typical signs, because such nerves perform strictly specific functions. For example, the ability to vibrate sensitivity may deteriorate: a person stops feeling touch, limbs and especially fingers begin to "go numb". Often the patient cannot feel whether he is wearing gloves or socks. It is also difficult for them to determine the size and shape of objects by touch. Over time, such problems lead to the loss of reflexes, to a distortion of the sense of the spatial position of the body.
Severe neuropathic pain gradually "shakes" the patient's psycho-emotional state, everyday activity and quality of life deteriorate. If the pain manifests itself mainly at night, then insomnia, irritability may occur, and work capacity deteriorates.
If the nerve structures responsible for pain and temperature sensitivity are affected, the patient becomes insensitive to pain and temperature stimuli. Less often, the opposite happens - when the patient perceives even a slight touch as severe and unbearable pain.
If clusters of autonomic nerve fibers are damaged, the consequences can become more dangerous - for example, if such nerves innervate the respiratory organs or the heart, breathing problems, arrhythmia, etc. may occur. The function of sweat glands is often impaired, urinary function is impaired, blood pressure gets out of control, depending on which nerves are affected.
The first signs most often manifest as pain in the limbs and muscles, but it happens that peripheral neuropathy reveals itself with other symptoms:
- loss of sensitivity in the fingers or limbs (this may include pain, temperature or tactile sensitivity);
- increased sensitivity of the fingers or limbs;
- a feeling of "goosebumps" or burning on the skin;
- spastic pain;
- unsteadiness of gait, impaired motor coordination and balance;
- increasing muscle weakness;
- problems with breathing, heart function, urination, erection.
There may also be other, non-specific manifestations of peripheral neuropathy, which must be reported to the doctor.
Peripheral neuropathy in children
The occurrence of peripheral neuropathy in childhood is most often hereditary. In many children, such neuropathies are manifested by the development of symmetrical, increasing muscle atrophy - mainly of the distal type.
For example, Charcot-Marie-Tooth disease is transmitted in an autosomal dominant manner and is the most common. The pathology is characterized by demyelination of damaged nerve fibers, with subsequent remyelination and hypertrophy, which leads to deformation of the nerves. In this case, the lower limbs are most often affected.
Acute childhood polyradiculoneuropathy is somewhat less common. This type of childhood neuropathy occurs 15-20 days after an infectious disease. The complication is manifested by impaired sensitivity in the lower extremities, symmetrical weakness, and loss of reflexes. If the bulbar muscles are involved in the process, then difficulties with chewing and swallowing are observed. The prognosis for such a disease is relatively favorable: as a rule, 95% of patients recover, but the rehabilitation period can last up to 2 years.
Forms
Peripheral neuropathy includes a number of painful conditions that, although they have common characteristics, can be quite diverse. This allows us to distinguish different types of peripheral neuropathies, which depends on both the localization of the lesion and the mechanism of pathology development.
- Peripheral neuropathy of the lower extremities is the most common of all types of this disease. The lower extremities suffer due to predominant damage to the long nerves, so the first signs usually affect the furthest parts of the legs - the ankles. Over time, the disease moves higher, the calves and knees are involved in the process: muscle function and sensitivity deteriorate, blood flow is difficult.
- Diabetic peripheral neuropathy is a common complication that occurs in patients with diabetes. As a rule, such a diagnosis is made to patients with obvious symptoms of damage to the peripheral nerves. Diabetic neuropathy is characterized by deterioration of sensitivity, disorders of the autonomic nervous system, urinary disorders, etc. In practice, this is manifested by numbness of the legs and/or arms, problems with the heart, blood vessels, and digestive organs.
- Peripheral neuropathy of the facial nerve manifests itself as unilateral paralysis of the facial muscles caused by damage to the facial nerve. The facial nerve branches in two, but only one of the branches is affected. This is why signs of neuropathy with damage to the facial nerve appear on one half of the face. The affected area of the face takes on a "mask-like" appearance: wrinkles are smoothed out, facial expressions disappear completely, pain and a feeling of numbness may bother, including in the ear area on the affected side. Tearing, salivation, and changes in taste sensations are often observed.
- Peripheral neuropathy of the upper extremities may manifest itself as damage to one of the three main nerve cords: the radial nerve, the median nerve, or the ulnar nerve. Accordingly, the clinical picture will depend on which nerve is damaged. The most common symptoms that are present with any type of damage to the upper extremities are severe pain, numbness of the fingers or the entire hand. Additional signs are general manifestations of neuropathies: spastic muscle twitching, a feeling of "pins and needles", deterioration of sensitivity and motor coordination.
The classification also applies to predominant nerve damage. As is known, there are three types of nerves, and they are responsible for sensitivity, motor activity and vegetative function. Accordingly, peripheral neuropathy can be of several types:
- Peripheral sensory neuropathy is diagnosed when sensory nerve fibers are damaged. The pathology is characterized by acute pain, tingling, and increased sensitivity (decreased sensitivity also occurs, but much less frequently).
- Peripheral motor neuropathy occurs with damage to the motor nerve fibers. This pathology is manifested by muscle weakness, which diverges from the lower to the upper sections, which can cause a complete loss of motor ability. Impaired motor function is accompanied by frequent convulsions.
- Peripheral sensorimotor neuropathy has a mixed nature of damage and is manifested by all of the listed clinical signs.
- Peripheral autonomic neuropathy is a lesion of the nerves of the autonomic nervous system. The clinical picture is characterized by increased sweating, impaired potency, and difficulty urinating.
There is also a clinical classification of peripheral neuropathy, according to which the following stages of pathology are distinguished:
- Subclinical stage of initial manifestations.
- The clinical stage of neuropathy is the stage of a vivid clinical picture, which is divided into the following categories:
- chronic pain stage;
- acute pain stage;
- a stage without pain against the background of decreased or complete loss of sensitivity.
- Stage of late consequences and complications.
Complications and consequences
Peripheral neuropathy can significantly undermine a person's health. Thus, the possibility of developing negative consequences and complications is not excluded. First of all, with peripheral neuropathy, sensory function suffers, which threatens complications such as:
- severe “shooting” pain in the area of nerve innervation;
- sensation of a foreign object under the skin;
- loss of thermal sensitivity, which, in turn, can cause burns, cryotrauma, etc.
However, more serious complications may also occur when the autonomic nervous system is damaged:
- deterioration of the skin condition;
- hair loss at the site of innervation;
- hyperpigmentation of the skin;
- sweating disorder;
- disruption of skin trophism, formation of erosions, ulcers, and even gangrene of the limb.
If the nerves responsible for motor activity are affected, smoothing of the knee and other reflexes may be observed. Often, spasmodic convulsions, muscle weakness, and muscle atrophy occur. In such cases, the disease often ends in disability.
Diagnostics peripheral neuropathy
Diagnosis is sometimes difficult due to the variety of symptoms of peripheral neuropathy. Most patients have to undergo a full course of neurological diagnostics to get the correct diagnosis.
The tests are performed to detect diabetes, vitamin deficiency, and disorders of the vascular and urinary systems. This is especially important if the innervation of individual organs is affected, or if peripheral neuropathy is caused by endocrine or other disorders.
Diagnostic testing of muscle strength helps detect seizure activity and motor nerve cell damage.
Instrumental diagnostics are prescribed selectively and may include the following procedures:
- Computer tomography, magnetic resonance imaging – allow you to find the cause of nerve compression (for example, a spinal hernia, a tumor process).
- Electromyography – helps to trace the transmission of nerve impulses to the muscles.
- Nerve conduction testing is a diagnostic test of the transmission of nerve impulses by placing electrodes on the skin.
Who to contact?
Treatment peripheral neuropathy
Treatment is based on eliminating the underlying pathology that caused the development of peripheral neuropathy. For example, if diabetes mellitus was a factor in the development of the disease, then it is necessary to establish control over the blood sugar level first. If peripheral neuropathy was provoked by vitamin B deficiency, then it is important to establish additional intake of multivitamins, as well as adjust the patient's diet.
Often, timely medical intervention not only alleviates the patient's condition, but also helps stop further progression of peripheral neuropathy. However, it is better to use a combination of different treatment methods.
Patients with peripheral neuropathy may be prescribed the following medications:
- Analgesics – for example, Paracetamol, non-steroidal anti-inflammatory drugs (Ibuprofen, Ortofen).
- Medicines aimed at improving blood circulation (Actovegin, Pentoxifylline).
- B-group vitamins (Undevit, Neurorubin).
- Anticholinesterase drugs (Axamon, Proserin).
If peripheral neuropathy is severe, the doctor may additionally prescribe anticonvulsants (for example, Sibazon), antidepressants (St. John's wort).
For severe pain, prescription analgesics (Tramadol) are used.
In case of peripheral neuropathy of autoimmune origin, plasmapheresis and intravenous administration of immunoglobulin are used - this allows suppressing the activity of the body's own immune system and stopping the attack on nerve fibers.
Method of administration and dosage |
Side effects |
Special instructions |
|
Ortofen |
The daily dose is 100-150 mg, taken in 2-3 doses. |
Depression, headache, stomach pain, trembling fingers, irritability. |
If the drug is to be taken for a long time, it is necessary to provide additional protection for the digestive system in advance. |
Actovegin |
Administer intravenously, 20-30 ml with 200 ml of the main solution, daily for a month. |
There is a risk of allergy, including the development of anaphylaxis. |
Before starting treatment, a test injection is required to rule out allergies - 2 ml is administered intramuscularly. |
Neurorubin |
Administer intramuscularly one ampoule per day until acute clinical signs are eliminated. |
Feeling of anxiety, tachycardia, digestive disorders. |
Long-term use of the drug (more than six months) can cause the development of reverse peripheral sensory neuropathy, so the issue of long-term treatment is discussed with the doctor individually. |
Aksamon |
Administer intramuscularly 5-15 mg up to 2 times a day for 10-15 days, sometimes up to a month. |
Tachycardia, nausea, increased salivation and sweating. |
Axamon enhances the sedative effect of many drugs, so you must be careful when driving a car and working with various mechanisms. |
Tramadol |
Prescribed only by a doctor for severe pain, 50 mg per dose. The daily limit of the drug is 400 mg. |
Tachycardia, nausea, dizziness, increased sweating, deterioration of vision and taste. |
During the treatment period, the consumption of alcohol in any form is prohibited. |
Physiotherapy treatment
Physiotherapy is used quite often for peripheral neuropathy. Regular and properly selected procedures help restore the lost functionality of the muscles and restore the blood supply to the tissues. However, physiotherapy methods are allowed to be used only after the acute period of the disease has ended, as well as during rehabilitation measures.
Electrophoresis with drugs that improve metabolism and vascular circulation is successfully used. Myoelectric stimulation procedures help neurons restore their sensory and motor abilities. However, it is better if the listed methods are used in combination.
Massage, including water massage, has a mechanical effect that accelerates blood circulation and metabolic processes in sore arms or legs.
Physical therapy sessions are mandatory to maintain muscle tone.
Folk remedies
There are many folk remedies known to alleviate the condition of a patient with peripheral neuropathy. However, we strongly advise: when using such folk remedies, you must first consult with your doctor.
The following recipes are considered by people to be the most effective.
- Cocktail with egg yolks and honey.
The ingredients required are one fresh egg yolk, 4 tsp. unrefined vegetable oil, 100 ml freshly squeezed carrot juice and 2 tsp. honey. All ingredients should be mixed well in a blender. The resulting amount of medicine should be drunk daily twice (morning and evening) before meals.
- Salt bath.
Pour hot water (approximately 55°C) into a basin to half the capacity. Add 200 g of salt and 150 ml of table vinegar. Dip the affected limbs into the solution for 20 minutes. The procedure is carried out daily for 4 weeks.
- Clay mask.
Dilute 120 g of cosmetic clay with water until it reaches the consistency of sour cream. Apply the mixture to the affected area and leave until dry. Perform the procedure daily until the condition improves steadily.
- Massage with camphor oil.
Camphor oil is rubbed into the affected area with light massaging movements, then left to soak in for a quarter of an hour. Then the affected area is intensively rubbed with alcohol and wrapped warmly. The procedure is repeated every day, preferably at night, for 4 weeks.
 [ 43 ], [ 44 ], [ 45 ], [ 46 ]
[ 43 ], [ 44 ], [ 45 ], [ 46 ]
Herbal treatment
You can add medicinal plant treatment to folk treatment. The simplest and most effective method is considered to be this: spring nettle leaves are laid out on the floor and you walk on them with bare feet.
The following methods can also improve the effect of basic drug treatment:
- An infusion is prepared from laurel powder and fenugreek seeds. To prepare the infusion, brew 2 teaspoons of laurel powder and 2 full tablespoons of fenugreek seeds in a 1 liter thermos. Infuse for 2 hours, filter and drink little by little throughout the day.
- Brew 2 tbsp. of calendula in 200 ml of boiling water, leave for half an hour. Take 100 ml per day for a month.
- Prepare a bath with pine branches and red hot pepper. Boil half a kilogram of pine branches in 3 liters of water, add 2 tbsp. of ground pepper, pour into a basin. Dilute with water so that the solution is not too hot. Steam your feet for about half an hour, overnight.
Homeopathy
As a supplement to the main therapy, you can also consider the use of homeopathic remedies:
- Aconite - used for dry skin, tingling, tremors, cramps.
- Alumen – used for unbearable itching, ulceration, paresthesia.
- Argentum nitricum – suitable for the treatment of diabetic neuropathy.
- Carcinosinum is indicated for delayed wound healing and purulent processes in the extremities affected by neuropathy.
- Colchicum is used for neuropathy, which is accompanied by joint damage.
- Graphitis - especially suitable for the treatment of diabetic foot syndrome.
- Mercurius solubilis is indicated for skin itching and trophic disorders.
- Phosphorus - used for complications of neuropathy.
- Secale cornutum is recommended for dry gangrene and paresthesia.
The dosages of the listed drugs are individual: they are prescribed by a homeopathic doctor after a personal consultation.
Surgical treatment
Surgery may be needed if peripheral neuropathy is associated with tumor processes that compress the nerves. Surgical treatment is also appropriate for vertebral hernias and mononeuropathies. Thus, nerve compression can be eliminated by cutting tendon or muscle fibers. This is how carpal tunnel syndrome is treated.
Prevention
The best option for preventing peripheral neuropathy is proper nutrition with healthy food while quitting smoking and drinking alcohol. Statistics provided by the WHO indicate that approximately 80% of neuropathies occur as a result of metabolic disorders and chronic intoxications.
Patients suffering from diabetes should constantly monitor their blood glucose levels. When sugar levels are elevated, glucose has a toxic effect on neurons.
People who spend a lot of time "on their feet" need to pay special attention to the quality of the shoes they wear. Shoes should be comfortable and of high quality.
Regular walking is recommended as a preventive measure, as it activates the immune system and improves the cardiovascular system. A good night's rest in a comfortable bed and a well-ventilated room also helps restore nerves.
Forecast
In case of timely seeking of medical help, with correct treatment of the disease, the prognosis of peripheral neuropathy can be considered favorable.
In case of hereditary etiology of peripheral neuropathy, it is impossible to talk about a complete cure, but there is a possibility of slowing down the further development of the disease. As a rule, competent therapy and lifestyle changes can alleviate painful symptoms and prolong the ability of patients to work.
If you seek medical help late and complications develop, the prognosis cannot be considered favorable: many patients diagnosed with peripheral neuropathy subsequently become disabled.

