Medical expert of the article
New publications
Chromoblastomycosis pathogens
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Chromoblastomycosis (chromomycosis) is a chronic granulomatous inflammation with damage to the skin and subcutaneous tissue of the legs. Chromoblastomycosis is caused by many fungi, including Fonsecaea ctmpaeta, Fonsecaea pedroaoi, Phiahphora verrucosa, Ctadophiatophora carrionii, Exaphiala jeamelmei, Rilinosporidium seeheri. Many of them are dimorphic fungi. They belong (along with the causative agents of phaeohyphomycosis and mycetoma) to demacium fungi, characterized by a brown-black shade of the colony and cell walls of the fungal elements. The dark shade is due to the presence of melanins in them.
Morphology and physiology
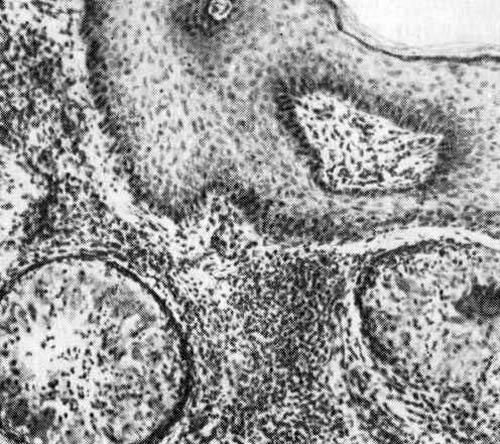
The pathogens are found in tissues and exudates in the form of clusters of round dividing cells (diameter 10 µm). Fungi grown on Sabouraud medium form fluffy colonies of dark brown tones, consisting of septate mycelium and different types of conidia.
Pathogenesis and symptoms of chromoblastomycosis
Infection occurs when the pathogen enters microtraumas of the skin, most often on the feet and shins. Over the course of several months or years, warty nodules form on the skin, abscesses and cicatricial changes appear. Convex satellite changes in the form of cauliflower form around the primary lesion. Cellular immunity predominates in patients, and DTH develops.
Microbiological diagnostics of chromoblastomycosis
In pathological material treated with 15% KOH solution, brown round cells of the pathogen measuring 10-12 µm are detected, the so-called sclerotia with partitions. The exception is Exophiala, which is distinguished by the formation of septate hyphae, as well as Rhinosporidium seeber, which forms sporangia and sporangiospores.
When cultivated on Sabouraud agar at 20-25 °C, the causative agents of chromoblastomycosis form slow-growing colonies (growth 11 days), consisting of black septate mycelium and different types of conidia.


 [
[