Medical expert of the article
New publications
Paraurethral cyst: signs, treatment with surgery
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Women of reproductive age experience various conditions, some of them are very common and some are rare but can potentially hinder their lifestyle. One of them is the formation of cysts in the reproductive organs. Cysts are common in women, but some cysts are rarely found in men in the urethra. This condition is also known as a paraurethral cyst. Let's take a closer look.
Epidemiology
Prevalence statistics suggest that paraurethral cysts typically occur between the ages of 20 and 60 years in approximately 1-6% of women. Urethral diverticula account for approximately 80% of paraurethral cystic lesions. Because of their usually asymptomatic nature, paraurethral cysts are rarely diagnosed and treated, and reports available in databases are relatively scarce. Patients most often present to the physician during the third and fourth decades of life due to recurrent infections and urinary disorders of unknown cause.
Causes a paraurethral cyst
A paraurethral cyst in women is classified primarily as acquired or congenital, although a clear distinction is often difficult. The main causes of the development of pathology are derived from this.
The female reproductive system develops from the Müllerian ducts. Inadequate absorption of the Müllerian contents can lead to stasis cysts. Most congenital vaginal cysts originate from the Müllerian ducts (they are the second most common vaginal cysts after acquired squamous cell cysts.) They are most often located around the vagina in the anterior or anterior trunk of the vagina. Congenital paraurethral cysts arise from various embryological components and vestigial remnants of the vagina and female urethra. To understand the mechanism of cyst formation, one must know some of the embryology and where the cyst may originate from. The vagina originates from the paramesonephric (Müllerian) duct, the mesonephric (Wolffian) duct, and the urogenital sinus. Most vaginal cysts are of Müllerian duct origin. They usually produce mucus and may be symptomatic, especially in older patients.
The paraurethral glands and ducts that descend into the female urethra are rudimentary analogues of the prostate gland in men. There are 6-30 paraurethral ducts. The two largest canals are commonly called Skene's canals. Paraurethral cysts arise from the Skene's canal. These glands secrete a small amount of mucoid material that serves to lubricate the urethral meatus during intercourse.
It performs many important functions in women and men:
- Secretes fluid to lubricate the opening of the urethra.
- The secreted fluids contain antimicrobial properties to protect the urinary tract from infection.
- It also secretes an ejaculate known as prostate-specific antigen, which is found in men. Prostate-specific antigen is a type of protein produced by the epithelial cells of the prostate gland.
And a cyst is formed when the outflow of fluid from the gland is blocked and its swelling occurs. Such a cyst is lined with transitional epithelium. However, some of the paraurethral ducts opening distally near the external meatus are lined with stratified squamous epithelium. Cysts derived from persistent mesonephric (Gartner's) ducts are lined with cuboidal or low columnar epithelium and do not secrete mucus. They are usually located in the anterolateral wall of the vagina and are usually asymptomatic.
Microscopically, cysts are usually lined by stratified squamous epithelium and may contain caseous or purulent material.
Acquired cysts are the most common cystic lesion of the vagina, often considered secondary to trauma due to childbirth or caused by iatrogenic surgical trauma, such as episiotomy. When the duct in these glands becomes clogged, fluid begins to accumulate, leading to the formation of cysts. Causes of obstruction of fluid outflow from the cyst can be not only trauma, but also pregnancy, long-term persistent infection.
Risk factors
Risk factors are not limited to age alone. Currently, no specific risk factors have been identified for the formation of a Skene's canal cyst.
It is important to note that having a risk factor does not mean that a person will get the disease. A risk factor increases the likelihood of getting the condition compared to a person without risk factors.
A paraurethral cyst in men is a rare phenomenon, since these glands are poorly developed in men, and their function is replaced by the prostate. The reason for the formation of a cyst in men is unclear, but it most often occurs after the first sexual experience in those whose gland has not been completely reduced. Infection is important in the development of inflammation.
 [ 11 ]
[ 11 ]
Pathogenesis
The pathogenesis of further complications is that this condition causes enlargement and swelling of these glands and in the worst case, the cyst can turn into a painless abscess, which can be formed due to bacteria or pathogens. The main bacteria responsible for this are often Chlamydia and N. gonorrhea. Opportunistic infections in patients suffering from HIV can also cause this type of infection.
Paraurethral gland cysts are rare in the young age group. As a rule, paraurethral cysts are formed in adult women (middle-aged and elderly women). In rare cases, this condition is also observed in infants.
Symptoms a paraurethral cyst
The first symptoms of the disease with a small cyst may be frequent urinary tract infections. This is because the cyst may be a source of infection that is difficult to identify.
Most of the time, the glands will be less than 1 centimeter in diameter and will be asymptomatic. When patients begin to notice symptoms, the cyst is usually larger than 1 centimeter. Symptoms that accompany the appearance of paraurethral cysts include: the presence of a palpable, sometimes visible thickening or nodule in the vaginal area or external urethra. There may also often be pain in the female genital area, dysuria, dyspareunia, and impaired urine flow. Other symptoms of the cyst may include painful sex, discomfort when sitting and walking. Larger cysts may block the urethra, causing painful urination.
If this cyst progresses without treatment, it will develop further into an abscess, which can become much more difficult for patients. Some women may develop fever as a result of the abscess forming in the gland.
Is it possible to get pregnant if you have a paraurethral cyst? This question interests many, since the pathology is quite common. The gland itself does not have any obstacles to normal fertilization. But it can be a hidden source of infection, which can be dangerous for the child. During childbirth, a large cyst can interfere with the normal passage of the fetus through the birth canal. Therefore, it is not recommended to get pregnant with such a pathology, since there may be complications.
Stages
The stages of cyst development are its increase in size, and the final stage can be considered the formation of an abscess. The types of cysts are determined histologically, and this is indicated by the cellular layer that lines the cyst from the inside. This is not very important for treatment, but can have prognostic significance in terms of the development of dysplasia in the future.
Complications and consequences
The consequences and complications of a cyst may be the following:
- continuous and recurring occurrence of cysts;
- recurrence of abscesses that will need to be treated on an ongoing basis;
- damage to muscles, vital nerves and blood vessels during surgery;
- Post-surgical wound site infection is a potential complication.
When a paraurethral cyst bursts, everything depends on its contents. If there is a simple transudate, there should be no consequences and simple preventive antibacterial treatment can be used. If the cyst contained pus, then it is imperative to sanitize the cyst cavity, as this can become a source of infection and be complicated by the development of inflammation of the genitals.
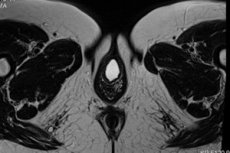
Diagnostics a paraurethral cyst
Diagnosis of pathology should begin with collecting complaints. Physical examination allows to determine changes in 63% of cases. There is a change in the vaginal wall, which can cause purulent or bleeding secretion from the urethra. During a pelvic examination, doctors can usually feel cysts or abscesses if they are large enough to cause symptoms. The doctor can also visually determine a round cyst of the canal during examination.
Instrumental diagnostics are performed to clarify the diagnosis. Ultrasonography is often used for more detailed information. Cystoscopy can also be performed using a flexible viewing tube to examine the bladder.
Another option may include a fine-needle biopsy, which involves inserting a thin needle into the cyst and removing its contents. This sample is then sent for lab testing. For women aged 40 and over, a biopsy will also help determine the presence of any cancer cells. These tests can help determine the type of cyst, as well as the treatment plan.
Many medical conditions can have similar signs and symptoms. Your doctor may perform additional tests to rule out other medical conditions to arrive at a definitive diagnosis.
Differential diagnosis
Differential diagnostics of paraurethral cyst should be carried out with the following pathology: ureterocele; Gartner canal cyst; Müllerian remnant cyst; vaginal wall inclusion cysts; urethral or vaginal neoplasm; urethral prolapse; urethral diverticulum.
A ureterocele is a congenital anomaly that involves cystic dilation of the terminal ureter, often associated with a stenotic orifice. About 90% of ectopic ureteroceles involve the upper portion of a duplex collecting system and 10% involve a single system. In women, ureteroceles may occur after genitourinary infections. A prolapsed ureterocele is a smooth, round, interstitial mass of variable size and color. The main differential diagnosis of a ureterocele, as opposed to a cyst, is aspiration of the material. If the fluid aspirated from the mass is urine, the diagnosis will be definitive.
Gartner canal cysts are lined with cuboidal or low columnar epithelium and do not secrete mucus. They are located on the anterolateral portions of the vagina, lateral to the upper and anterior to the lower portion. Usually, the cysts are solitary, may be small, or they may become so large that they protrude from the vagina. Biopsy analysis is also the main differential feature of such a cyst.
Urethral or vaginal neoplasm: Paraurethral masses may be solid or cystic. Solid masses are usually evident on physical examination and include fibroma, leiomyoma, neurofibroma, lipoma, myoblastoma, hemangioblastoma, lymphangioma, and their malignant counterparts. Most patients are over 50 years of age. Tumors may have a variety of manifestations: papillary growth in the urethra, as a soft, friable, fungal mass, ulcerative lesions, or as a submucosal mass creating a thickening of the anterior vaginal wall. Pelvic examination (under general anesthesia) is required, combined with cystourethroscopy and biopsy of the lesion. In the initial stages of differential diagnosis of a paraurethral cyst and neoplasm, the most important thing is the biopsy result - if the cells have abnormal or atypical features, then this indicates a neoplasm.
Who to contact?
Treatment a paraurethral cyst
Treatment will depend on various factors such as symptoms, the size of the cyst, or whether the cyst is infected. In most cases, when the cysts are small and do not cause any symptoms, you will not need any treatment. In other cases, the following treatment options are available.
Drug treatment is the use of certain medications.
- Iodinol is used as an antiseptic for paraurethral cysts. The drug contains iodine ion and alcohol. These are strong antibacterial drugs with a pronounced antiseptic effect. The drugs are used externally. Method of application - you can use the solution for lubrication three to four times a day, which is not very convenient to do yourself. Therefore, you can do baths or douches, diluting the drug with water. Side effects can be in the form of a strong allergic reaction to iodine. With a high concentration of alcohol, there may be a burning sensation or itching.
- When the cyst infection is caused by bacteria, antibiotic therapy may be used. Your doctor may prescribe antibiotics such as penicillin. Amoxiclav is an antibiotic that is protected from destruction by bacteria. The drug may be a first-line antibiotic. The dosage is 500 milligrams three times a day for at least five days. Side effects of this group of antibiotics may include severe allergic reactions or stool disorders.
- Folk treatment is the use of home methods in which you have to sit in a warm bath filled with water for about 15-20 minutes per session. This should be repeated several times a day. Chlorhexidine can be added to the solution. If carried out for 3-4 days, the cyst may rupture and cause leakage of fluid. This method can be suggested to a patient with minor cysts.
- Use apple cider vinegar to try to shrink vaginal cysts. Either make a bath and add 1 tablespoon of vinegar, or you can make a cotton ball and use that. Apply the soaked cotton ball or ball directly to the cyst and hold it there for 30 minutes twice a day until you notice the swelling has gone down. While vinegar is a popular home remedy, scientists do not recommend using vinegar as a medicine.
- Use a warm compress. Fill a bottle with hot water and wrap it in a clean towel. Place it against the cyst to provide some pain relief. You can also try applying a heat pack. You can also dip a flannel or cotton cloth in hot water, squeeze out the water, and apply it directly to the cyst.
- Apply aloe vera mixture. Mix 1 to 2 tablespoons of aloe vera gel with 1/4 to 1/2 teaspoon of turmeric powder. Stir until the mixture forms a paste. Use a cotton swab to apply the mixture to the cyst. Leave it on for 20 to 30 minutes once a day. Do not rinse or scrub the paste. Studies have shown that turmeric is an anti-inflammatory agent that can reduce irritation caused by vaginal cysts.
Vitamins can be used, but physiotherapy treatment is only indicated in the postoperative period. Iontophoresis with antibiotics can be used for better scar healing.
Surgical treatment is an option for women with large cysts or abscesses. Removal of a paraurethral cyst or excision of a paraurethral cyst is performed when there is a risk of malignancy or its size interferes with daily life. The doctor will make a small incision in the cyst and extract the contents there. The postoperative period involves the prescription of antibiotics if there is an infection in the cyst or an abscess caused by bacteria, as well as to prevent complications. Temperature after removal of a paraurethral cyst may be due to the development of infection and secondary infection, so this condition must be carefully monitored.
Marsupialization. This method is usually performed under local anesthesia. It is used in cases where cysts frequently recur or where surgical removal is not desired. The doctor will first give you a local anesthetic. Then an incision will be made into the cyst or abscess and a drain will be placed on each side. A catheter will be placed in the hole to allow drainage of the fluid. This will be a small, permanent opening so that the fluid can drain freely. Post-operative care is important: a minimum level of activity should be provided until the surgical wound has healed. Follow-up care with regular screening and check-ups is important. Most women experience relief after drainage. At follow-up checks one year after the procedure, almost all patients have no further symptoms of discomfort when urinating and there is no visual evidence of a cyst.
Prevention
Prevention of the formation of paraurethral glands is a little complicated, since there are no direct causes for the development of this pathology.
There are no specific ways to prevent a cyst from developing. However, by taking certain measures, the risk of further complications can be reduced:
- Safe sex practices (such as using condoms).
- Always maintain good personal hygiene.
- Drink plenty of water and other fluids (such as fruit juices).
- Medical check-ups at regular intervals with scans and physical examinations (as recommended by your doctor) are recommended.
Forecast
The prognosis for a paraurethral cyst is usually good with proper treatment. Most women experience relief after drainage of the abscess. In very rare cases, women may experience recurrent cysts and abscesses, which may require treatment through a surgical procedure called marsupialization.
Today, a paraurethral cyst is an unpleasant pathology that brings a lot of inconvenience to both women and men. Early diagnosis makes it possible to carry out effective treatment and improves the prognosis. Treatment methods are limited by the individual characteristics of the cyst, but the main thing is preventive measures.

