Medical expert of the article
New publications
Subependymal cyst in a newborn baby
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
When performing a neurosonography of the brain, doctors sometimes discover a benign hollow neoplasm, after which they announce the diagnosis of "subependymal cyst in a newborn." What kind of pathology is this, how does it appear and is there a need for its treatment? How will such a cyst affect the growth and development of the child?
Let's say right away: this problem is not as scary as it usually seems to parents. Below you can read everything you need to know first of all about subependymal cyst in a newborn.
Epidemiology
They are detected in up to 5.2% of all newborns using transfontanellar ultrasound in the first days of life. [ 1 ]
A subependymal cyst is a tiny, often tear-shaped lesion that contains cerebrospinal fluid, the fluid that bathes the brain; it is located either in the caudate groove or along the anterior caudate nucleus. The size of the cystic lesion typically ranges from 2-11 millimeters. [ 2 ]
The most common cause of subependymal cyst formation is considered to be hypoxia or ischemia of the brain during labor. Although most specialists are inclined to believe that the true causes of the pathology have not yet been revealed.
Subependymal cysts are found in approximately five out of a hundred newborn children and, as a rule, have a favorable prognosis for the development and life of the child.
Causes subependymal cyst
With oxygen deficiency, which is observed in the fetus against the background of placental blood circulation disorder, the development of some serious pathologies and developmental failures of the baby is possible. One of such failures is sometimes a subependymal cyst: this pathology is often diagnosed in newborns as a result of prolonged blood circulation disorder, oxygen and/or nutrient deficiency.
A subependymal cyst can be detected both during pregnancy and after the baby is born. During pregnancy, such a cystic formation is not dangerous for the fetus, and under favorable circumstances, it can disappear on its own even before labor begins.
The exact reasons for the formation of a subependymal cyst in newborns are unknown to doctors, [ 3 ] however, it is believed that the following factors can influence its development:
- hypoxic disorders associated with umbilical cord entanglement or fetoplacental insufficiency;
- herpes virus infection in pregnant women;
- injuries to the baby during labor;
- severe or late toxicosis in the expectant mother;
- cocaine exposure during pregnancy; [ 4 ], [ 5 ]
- Rhesus incompatibility;
- iron deficiency anemia during pregnancy.
Risk factors
The risk group includes premature babies and newborns with insufficient body weight. In addition, subependymal cysts are sometimes diagnosed in multiple pregnancies, which is caused by a lack of oxygen in the brain tissue. As a result, some cells die, and in their place a new growth appears, which, as it were, replaces the necrosis zone.
Important: the longer the period of oxygen deficiency, the larger the subependymal cyst will be.
Let's consider the basic factors of cyst formation in more detail:
- Ischemic processes are the most common underlying cause of cystic formation. Ischemia in this case is explained by impaired blood flow in the brain tissue. A cavity is formed in the necrosis zone, which is subsequently filled with cerebrospinal fluid. If such a cyst is small, then there is no talk of any serious disorders: treatment is usually not prescribed, but only monitoring of the problem area is established. In case of unfavorable dynamics (for example, with further enlargement of the cyst, with the appearance of neurological symptoms), treatment is started immediately.
- Hemorrhage is the next most common underlying cause of subependymal cysts. Hemorrhage often occurs due to infectious processes, acute oxygen deficiency, or birth trauma. The most unfavorable prognosis in this case is for damage associated with intrauterine infections. [ 6 ]
- Hypoxic processes in tissues can be acute or moderate and are usually associated with placental circulation disorders. The trigger mechanism is often anemia, toxicosis in late pregnancy, multiple pregnancy, Rh incompatibility, polyhydramnios, fetoplacental insufficiency, infectious and inflammatory pathologies.
- Congenital rubella and cytomegalovirus (CMV) infection are the most common proven causes of nonhemorrhagic subependymal cysts in neonates.[ 7 ]
Pathogenesis
A subependymal cyst is located in an area of impaired blood supply to brain structures. Most often, this is a problem with ventricular localization. Unlike congenital cysts, subependymal cysts are usually located below the outer angles of the lateral ventricles and behind the foramen of Monro. Subependymal cysts can be divided into two types: acquired (secondary to hemorrhage, hypoxia-ischemia, or infection) and congenital (resulting from germinolysis). They are often present after grade 1 hemorrhage in the germinal matrix, which is associated with prematurity. [ 8 ]
One in ten children who encountered the herpes virus during intrauterine development or birth will have a "mark" on their nervous system. If the infection was generalized, a large percentage of children die, and those who survive often have psychoneurological disorders. The formation of subependymal voids caused by the virus is explained by subsequent damage to the germinal matrix - nerve fibers located near the lateral ventricles. The infection causes the death of nerve cells, the zones of which are replaced after some time by the formation of voids.
Hypoxic or ischemic damage, accompanied by softening and necrosis of tissue, also ends with substitution formation of cavities. Oxygen deficiency during intrauterine development or labor has a negative effect on the nervous structures. The activity of free radicals, the production of acidic metabolic products, the formation of thrombi at the local level generally cause necrosis and the appearance of cysts near the ventricles. Such subependymal cysts can be multiple, up to 3 mm in diameter. During the collapse of the cavities, irreversible atrophy processes occur with the appearance of neuroglial nodes.
In cases of birth trauma and cerebral hemorrhages, cyst formation is caused by the resorption of leaked blood with the appearance of a void, which is subsequently mistaken for a subependymal cyst.
Symptoms subependymal cyst
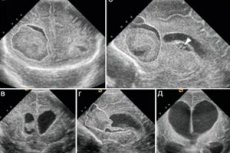
A subependymal cyst on an ultrasound image has clear boundaries and a spherical or slit-like configuration. In some cases, multiple lesions are observed, and the cysts are most often at different stages of development: some of them have just appeared, while others are already at the stage of “sticking together” and disappearing.
The size of a subependymal cyst in a newborn is usually 1-10 mm or more. They are formed symmetrically, on the left or right side, in the middle sections or horns of the lateral ventricles.
A subependymal cyst on the right side of a newborn is no more common than on the left. The more pronounced the oxygen deficiency, the larger the neoplasm will be. If there was a hemorrhage, the affected area will subsequently look like a single cavity with transparent liquid contents.
A left subependymal cyst in a newborn is usually not accompanied by a change in the size of the lateral ventricles, but in some cases they can still increase. Compression of adjacent tissues and further growth of the cavity are observed relatively rarely.
Over the course of several months from the moment the child is born, the neoplasm gradually decreases until it disappears completely.
The clinical picture of a subependymal cyst is not always the same, or is absent altogether. First of all, it depends on the size, number and localization of the lesion. With other combined pathologies, the symptoms are more severe and pronounced. Small cysts of a single location often do not reveal themselves in any way, do not affect the development of the child and do not cause complications.
The first signs of a bad subependymal cyst are as follows:
- sleep disturbances, excessive moodiness, crying for no reason;
- increased excitability, irritability, or apathy, lethargy and inhibited state;
- motor development disorders in children, increased muscle tone, and in severe cases – hypotonia, hyporeflexia; [ 9 ]
- insufficient weight gain, weakened sucking reflex;
- deterioration of hearing and vision;
- slight tremors of the limbs, chin;
- profuse and frequent regurgitation;
- increased intracranial pressure (prominent and pulsating fontanelle);
- convulsions.
The above symptoms are not always bright and clear. In the process of resorption of the subependymal cyst, the clinical picture usually weakens and even disappears. If the neoplasm continues to grow, then inhibition of psychomotor development, growth deficiency, and speech problems may be observed.
A subependymal cyst that is accompanied by any suspicious symptoms should be closely monitored by a physician.
Complications and consequences
Subependymal cysts in newborns in the vast majority of cases disappear on their own within a few months, without any treatment. However, it is necessary to monitor the cyst, since in rare cases, but still, unfavorable dynamics, growth and enlargement of the neoplasm are possible. If this happens, the following complications may occur:
- coordination disorders, movement disorders;
- problems with the hearing and visual apparatus;
- hydrocephalus, accompanied by excessive accumulation of cerebrospinal fluid in the cerebral ventricles;
- encephalitis.
Children with subependymal cysts (SECs) may experience temporary delays in physical growth after birth.[ 10 ]
Large subependymal cysts that put pressure on nearby brain structures are most often removed by surgery.
Diagnostics subependymal cyst
Diagnostics are performed using ultrasound in the first few days after the birth of the child. Since the area of the large fontanelle in a newborn is most often open, this makes it possible to examine all structural abnormalities without harming the baby. If the fontanelle is closed, magnetic resonance imaging becomes the optimal visualization method. Instrumental diagnostics are performed regularly, over several months, to observe the dynamics of the neoplasm.
If a woman is diagnosed with herpesvirus or cytomegalovirus, then additional tests are prescribed to clarify the diagnosis – this is called immunological diagnostics. This allows us to decide on subsequent therapeutic tactics. [ 11 ]
Immunological tests are complex and expensive, so they are often inaccessible to average families. In addition, even a confirmed herpesvirus infection does not provide any information about the degree of brain damage in a newborn. For this reason, most specialists believe that it is more logical to perform an echoencephalography procedure: its results will indicate the severity and nature of the brain structure disorder. The procedure is not dangerous and will not lead to unpleasant consequences for the baby.
Differential diagnosis
Differential diagnosis is made between connatal, subependymal cysts and periventricular leukomalacia. The latter pathology is localized above the angle of the lateral ventricles. Connatal cyst is located at the level or slightly below the upper outer angle of the anterior horn and body of the lateral ventricle, in front of the interventricular foramen. Subependymal cyst is predominantly located below the level of the angle of the lateral ventricles and behind the interventricular foramen.
Isolated SECs are usually a benign finding. Accurate diagnosis is important to differentiate subependymal cysts from other brain pathological conditions using a combination of brain ultrasound and MRI. [ 12 ] Magnetic resonance imaging helps to confirm the information [ 13 ] obtained from ultrasound, to determine the location of the subependymal cyst, and to differentiate the neoplasm from congenital cysts and other periventricular brain lesions. [ 14 ]
Treatment subependymal cyst
The treatment regimen for subependymal cysts in newborns is determined depending on the severity of the lesion. In the case of an asymptomatic cyst, no treatment is required: the problem is observed dynamically, the child is periodically examined by a neurologist, ultrasound monitoring is performed (when the fontanelle closes, an MRI is performed). Sometimes the doctor prescribes nootropic and vitamin drugs, although many specialists doubt the appropriateness of such a prescription.
In severe cases of damage, with combined brain pathologies, complex treatment is prescribed, using physiotherapy, massage and, of course, medications:
- Nootropic drugs improve metabolic processes in brain tissue. Such drugs include Piracetam, Nicergoline, Pantogam.
- Vitamin and mineral complexes improve tissue nutrition and stabilize tissue metabolism. B-group vitamins and magnesium-containing agents play a special role.
- Diuretics are appropriate when there is an increasing risk of cerebral edema or when intracranial pressure increases. The optimal diuretic drug is considered to be Diacarb.
- Anticonvulsants are used for convulsive syndrome. Depakine, Carbamazepine may be prescribed.
In infectious processes, children undergo immunotherapy with immunoglobulins (Pentaglobin, Cytotec), antiviral drugs (Virolex). The treatment regimen is determined individually.
Surgical treatment
Surgical removal of a subependymal cyst is extremely rare: only if the growth dynamics are unfavorable against the background of ineffective drug therapy. Surgical treatment can be performed using one of the following methods:
- The bypass method involves removing cerebrospinal fluid from the cystic cavity through a special tube, causing the walls to collapse and fuse. The procedure is quite effective, but dangerous due to the risk of infection getting into the tissue.
- The endoscopic method is considered the safest, but it is not suitable for all patients - for example, it cannot be used if the patient has visual impairment.
- Craniotomy is considered an effective operation and is used for large cystic formations.
A pediatric neurosurgeon performs such interventions only in the case of obvious progression and enlargement of the subependymal cyst, with a high risk of complications. During the operation, computer monitoring is performed: the image is displayed on the monitor, so the doctor has the opportunity to track all important operational moments, analyze and correct manipulations.
Prevention
Preventive measures to prevent the formation of subependymal cysts in children are based on the following criteria:
- mandatory pregnancy planning;
- early prenatal diagnostic measures;
- prevention of injuries during labor;
- neurological and pediatric monitoring of children belonging to risk groups.
In addition, it is important to exclude any teratogenic effects, especially in the early stages of the gestation period.
If necessary, the doctor may recommend that a pregnant woman undergo genetic counseling.
Forecast
If the subependymal cyst is isolated, i.e., not accompanied by neurological symptoms, not associated with other pathologies, has typical characteristics and is detected by ultrasound by chance, then we can talk about a good prognosis. Such neoplasms disappear on their own within a few months. The prognosis of isolated subependymal cysts remains uncertain. [ 15 ]
A poor prognosis is indicated if a subependymal cyst in a newborn is combined with other developmental anomalies.
Использованная литература

