Medical expert of the article
New publications
Adult pain rating scales
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Pain assessment scales are designed to determine the intensity of pain. The scales allow you to assess the subjective pain sensations that the patient experiences at the time of the study. The most widely used are verbal, visual and digital scales or scales that combine all three assessment options.
Verbal pain rating scales
Verbal Rating Scale
The verbal rating scale allows one to assess the intensity of pain by means of a qualitative verbal assessment. Pain intensity is described by specific terms ranging from 0 (no pain) to 4 (worst pain). From the proposed verbal characteristics, patients choose the one that best reflects the pain sensations they experience.
One of the features of verbal rating scales is that the verbal characteristics of the pain description can be presented to patients in a random order. This encourages the patient to select the pain gradation that is based on semantic content.
4-point verbal pain assessment scale (Ohnhaus EE, Adler R., 1975) |
5-point verbal pain rating scale |
||
No pain |
0 |
No pain |
0 |
Mild pain |
1 |
Mild pain |
1 |
Pain of moderate intensity |
2 |
Pain of moderate intensity |
2 |
Severe pain |
3 |
Severe pain |
3 |
Very severe pain |
4 |
||
Verbal descriptive pain scale
Verbal Descriptor Scale (Gaston-Johansson F., Albert M., Fagan E. et al., 1990)
When using a verbal descriptive scale, the patient must be asked whether he or she is experiencing any pain right now. If there is no pain, then his or her condition is assessed as 0 points. If there is pain, it is necessary to ask: "Would you say that the pain has increased, or is the pain unimaginable, or is this the most severe pain you have ever experienced?" If so, then the highest score of 10 points is recorded. If there is neither the first nor the second option, then it is necessary to clarify: "Would you say that your pain is mild, average (moderate, tolerable, not severe), severe (sharp), or very (especially, excessively) severe (acute)."
Thus, there are six possible options for pain assessment:
- 0 - no pain;
- 2 - mild pain;
- 4 - moderate pain;
- 6 - severe pain;
- 8 - very severe pain;
- 10 - unbearable pain.
If the patient experiences pain that cannot be characterized by the proposed characteristics, for example between moderate (4 points) and severe pain (6 points), then the pain is assessed with an odd number that is between these values (5 points).
The Verbal Descriptive Pain Rating Scale can also be used in children over the age of seven who are able to understand and use it. This scale can be useful for assessing both chronic and acute pain.
The scale is equally reliable for both primary school children and older age groups. In addition, this scale is effective for various ethnic and cultural groups, as well as for adults with minor cognitive impairments.
Facial pain scale
Faces Pain Scale (Bien, D. et al., 1990)
The facial pain scale was created in 1990 by Bieri D. et al. (1990).
The authors developed a scale to optimize the child's assessment of pain intensity using facial expressions that change with the degree of pain experienced. The scale is presented with pictures of seven faces, with the first face having a neutral expression. The next six faces depict increasing pain. The child must choose the face that, in his or her opinion, best demonstrates the level of pain he or she is experiencing.

The Facial Pain Scale has several features compared to other rating facial pain scales. First, it is more of a proportional scale than an ordinal one. In addition, the scale has the advantage that children can more easily relate their own pain to a drawing of a face presented on the scale than to a photograph of a face. The simplicity and ease of use of the scale make it possible for its wide clinical application. The scale has not been validated for work with preschool-aged children.
 [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
[ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
The Faces Pain Scale-Revised (FPS-R)
(Von Baeyer C. L. et al., 2001)
Carl von Baeyer and his students from the University of Saskatchewan (Canada) in collaboration with the Pain Research Unit modified the facial pain scale, which was called the modified facial pain scale. The authors left six faces in their version of the scale instead of seven, while maintaining a neutral facial expression. Each of the images presented in the scale received a numerical rating in the range from 0 to 10 points.
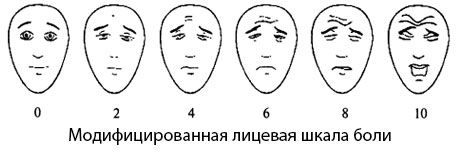
Instructions for using the scale:
"Look carefully at this picture, where there are faces that show how much pain you can have. This face (show the leftmost one) shows a person who is not in pain at all. These faces (show each face from left to right) show people whose pain is increasing, growing. The face on the right shows a person who is in unbearable pain. Now show me the face that shows how much pain you are in right now."
Visual Analogue Scale (VAS)
Visual Analogue Scale (VAS) (Huskisson E. S., 1974)
This method of subjective pain assessment involves asking the patient to mark a point on a 10 cm long ungraded line that corresponds to the degree of pain. The left border of the line corresponds to the definition of "no pain", the right - "the worst pain imaginable". As a rule, a paper, cardboard or plastic ruler of 10 cm in length is used.
On the back of the ruler there are centimeter divisions, according to which the doctor (and in foreign clinics this is the responsibility of the nursing staff) notes the obtained value and enters it into the observation sheet. The unconditional advantages of this scale include its simplicity and convenience.
Also, to assess the intensity of pain, a modified visual analogue scale can be used, in which the intensity of pain is also determined by different shades of color.
The disadvantage of VAS is its one-dimensionality, i.e. the patient only notes the intensity of pain on this scale. The emotional component of the pain syndrome introduces significant errors into the VAS indicator.
During dynamic assessment, a change in pain intensity is considered objective and significant if the current VAS value differs from the previous one by more than 13 mm.
Numerical Pain Scale (NPS)
Numeric Pain Scale (NPS) (McCaffery M., Beebe A., 1993)
Another scale is constructed according to the principle described above - a numerical pain scale. A ten-centimeter segment is divided by marks corresponding to centimeters. It is easier for the patient, unlike the VAS, to evaluate pain in digital terms; he determines its intensity on the scale much faster. However, it turned out that during repeated tests, the patient, remembering the numerical value of the previous measurement, subconsciously reproduces an intensity that does not really exist
Pain, but tends to remain in the area of the previously named values. Even with a feeling of relief, the patient tries to recognize a higher intensity, so as not to provoke the doctor to reduce the dose of opioids, etc. - the so-called symptom of fear of repeated pain. Hence the desire of clinicians to move away from digital values and replace them with verbal characteristics of pain intensity.
Bloechle et al. pain scale
Pain scale of Bloechle et al. (Bloechle C., Izbicki JR et al., 1995)
The scale was developed to assess pain intensity in patients with chronic pancreatitis. It includes four criteria:
- Frequency of pain attacks.
- Pain intensity (pain assessment on a VAS scale from 0 to 100).
- The need for analgesics to relieve pain (the maximum degree of severity is the need for morphine).
- Lack of performance.
NB!: The scale does not include such a characteristic as the duration of the pain attack.
Sign |
Characteristic |
Grade |
Frequency of pain attacks |
No |
0 |
Several times during the year (2-12 times/year) |
25 |
|
Several times a month (24-50 times/year) |
50 |
|
Several times a week (100-200 times/year) |
75 |
|
Daily (more than 300 times/year) |
100 |
|
Intensity of pain |
No |
0 |
Unbearable |
100 |
Sign |
Characteristic |
Grade |
The need for analgesics to relieve pain |
No |
0 |
Aspirin |
1 |
|
Tramadol |
15 |
|
Buprenorphine |
80 |
|
Morphine |
100 |
|
Duration of disability during the past year due to pain |
No |
0 |
1-7 days |
25 |
|
Up to 1 month |
50 |
|
Up to 365 days a year |
75 |
|
Constantly |
100 |
When using more than one analgesic, the need for analgesics to relieve pain is equal to 100 (maximum score).
If there is continuous pain, it is also rated at 100 points.
The scale is assessed by summing up the scores for all four features. The pain index is calculated using the formula:
Overall rating on scale/4.
The minimum score on the scale is 0, and the maximum is 100 points.
The higher the score, the more intense the pain and its impact on the patient.
Observational-based pain assessment scale for intensive care units
Critical Care Pain Observation Tool (CPOT) (Gelinas S., Fortier M. et al., 2004)
The CPOT scale can be used to assess pain in adult patients in the ICU. It includes four features, which are presented below:
- Facial expression.
- Motor reactions.
- Tension in the muscles of the upper limbs.
- Speech responses (in non-intubated patients) or ventilator resistance (in intubated patients).

