Medical expert of the article
New publications
Osteoblastoclastoma
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Cases of oncological diseases are constantly increasing in the world. Among the lesions of the skeletal system, osteoblastoclastoma (giant cell tumor, osteoclastoma) is the most frequent – a benign tumor process prone to malignancy, capable of damaging a variety of skeletal bones. [ 1 ] The primary clinical picture of the disease proceeds unnoticed, but over time, swelling of a separate bone area attracts attention: the tumor increases gradually, painlessly. Treatment of the pathology is surgical, involving the removal of osteoblastoclastoma within healthy tissues. With timely treatment, the outcome of the disease is considered encouraging. [ 2 ]
Epidemiology
The first detailed description of this tumor was given by the French surgeon August Nelaton in the 19th century. The giant cell formation was included in the category of fibrous osteodystrophies. The pathology was called by different terms: brown tumor, gigantoma, osteoclastoma, local fibrous osteodystrophy, giant cell sarcoma. The name osteoblastoclastoma was introduced into medical terminology by Professor Rusakov.
Today, specialists have no doubts about the tumor origin of osteoblastoclastoma, which is considered one of the most common bone neoplasms. The disease occurs in men and women with approximately the same frequency. There are descriptions of family and hereditary pathology.
Osteoblastoclastoma can develop at almost any age. There are known cases of tumor detection in both one-year-old infants and 70-year-old elderly people. According to statistics, almost 60% of patients with such a neoplasm are people aged 20-30 years.
Osteoblastoclastoma belongs to the category of solitary tumors, usually single. Rarely do such foci develop in adjacent bone tissues. The lesion most often spreads to long tubular bones (almost 75% of cases), and small and flat bones are affected somewhat less often.
Long tubular bones are affected mainly in the epimetaphysis area (in childhood - in the metaphysis area). Tumor growth into the tissues of the articular and epiphyseal cartilage is not observed. Less often, the pathology affects the diaphysis area (less than 1% of cases).
Osteoblastoclastoma of the facial bones accounts for more than 20% of all tumors found in this location.
Medical specialists distinguish between malignant and benign osteoblastoclastoma. Malignant pathology is rare in childhood.
Causes osteoclastomas
Doctors cannot point to any one clear reason for the development of osteoblastoclastoma. It is believed that the appearance of the pathology can be influenced by:
- inflammatory processes affecting the bone and periosteum;
- traumatic injury or repeated injuries to the same area of bone;
- repeated irradiations;
- disruption of bone formation during the prenatal period.
In about seven out of ten cases, osteoblastoclastoma affects the long tubular bones, but it can spread into nearby tendons and soft tissues.
If the pathology develops in the maxillofacial area, then most often the cause is a bone injury or an infectious process - for example, after tooth extraction, extirpation. Less often, the appearance of a neoplasm is recorded in the area of the fibula and tibia, ribs and spinal column.
Women often suffer from the hands, toes, femurs, knee joints, with the formation of a tenosynovial giant cell tumor of diffuse form. Such a tumor has the appearance of a dense formation among soft tissues, localized near the tendons. Gradually, the process spreads to the articular bone, damaging and destroying it.
In general, the causes of osteoblastoclastoma are considered to be the following:
- changes in hormonal balance;
- endocrine pathologies;
- exposure to occupational hazards, bad habits;
- poor nutrition;
- long-term or incorrect use of certain medications;
- parasitic lesions;
- prolonged stay in radioactive zones.
Transformation of benign osteoblastoclastoma into a malignant tumor is possible under the influence of:
- frequent injuries to the pathologically altered bone segment;
- strong hormonal changes (for example, during pregnancy);
- repeated irradiation.
The factors listed above do not necessarily lead to the development of pathology, but they can have a negative impact on people predisposed to the development of osteoblastoclastoma.
Risk factors
Osteoblastoclastoma most often develops in patients over 10 years of age. In children under 5 years of age, the pathology is very rare.
The risk of developing a tumor increases under the influence of the following factors:
- Unfavorable environmental conditions, the presence of professional and domestic hazards, intoxications, chronic infectious diseases, parasitic infestations.
- History of oncological pathologies, previous radiation therapy (especially several courses), other exposure to radiation (including living or working in radioactively hazardous regions).
- Frequent injuries, fractures, bruises, bone cracks.
- Genetic factors, gene changes or mutations, cancer diagnoses in close relatives.
- Congenital bone defects, skeletal structure disorders.
Often, the environmental factor is not considered as the main reason, and completely in vain: environmental problems have a direct impact on the quality of air, food products, water regime of the area, which invariably affects health. The adverse effects of ultraviolet radiation are noted if a person visits beaches and open pools for a long time and regularly, gets sunburned.
The influence of carcinogens and radiation is also found in many hazardous industries involving chemicals such as nickel, asbestos, sulfuric acid, arsenic, as well as metal and plastic processing.
Pathogenesis
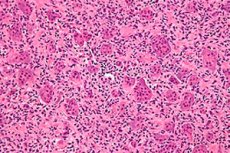
Giant cell tumor is a complex histologically benign bone lesion that rarely recurs, although it is certainly a source of "benign" metastases and frequently transforms into sarcoma after irradiation. In the absence of a clear histogenetic origin, giant cell tumor is named for its specific histologic appearance.
The typical morphologic description is a benign mononuclear stromal cell lesion with abundant benign osteoclast-like giant cells. Immunohistochemical and molecular studies of osteoclastoma tissues demonstrate two stromal cell populations, one composed of proliferating spindle cells that represent markers of osteoblastic origin,[ 3 ],[ 4 ] while the other population consists of polygonal cells that stain for CD14+/CD68+ monocyte/macrophage antigens.[ 5 ]
The main pathogenetic features of osteoblastoclastoma:
- The tumor includes two cell types: multinucleated giant cells and small mononuclear cells;
- most often affected are the distal segment of the femur, the proximal segment of the tibia, the distal segment of the radius, as well as the pelvic bones and scapula (less often - the spinal column);
- the lesion is predominantly isolated and solitary;
- the tumor is located in the epiphysis or metaphysis, which swells significantly, deforms in the form of a large tubercle or hemisphere;
- the pathological process reaches the articular cartilage and is interrupted;
- the neoplasm grows in all directions, but the main growth is observed along the long bone axis towards the diaphysis;
- the transverse dimension diametrically increases more than three times;
- in the cellular variant of osteoblastoclastoma, the neoplasm consists of chambers separated from each other by complete and partial barriers (like soap suds or irregular honeycombs);
- there is a divergence of the cortex, swelling from the inside, thinning, without periosteal layers;
- if the osteoblastoclastoma is of significant size, then the cortex is resorbed, the neoplasm is surrounded by a thin shell capsule consisting of the walls of the superficial chambers;
- in the osteolytic variant, there is no chamber pattern, the bone defect is homogeneous;
- saucer-shaped marginal defect;
- resorption of the cortical layer is observed, the crust becomes sharper at the line of damage, without undermining or periosteal layers;
- the defect has clear contours;
- pathological fractures are observed in 12% of patients.
Osteoblastoclastoma affects areas rich in myeloid bone marrow. Often, pronounced curvatures and shortening of the bone are detected - particularly in cases of delayed diagnosis and treatment. In most cases, the tumor is located eccentrically, with the destruction of the overwhelming majority of bone condyles. Radiologically, reaching the subchondral bone layer is noted. In almost half of the cases, the entire articular end of the bone is affected, which swells, the cortical layer is destroyed, the lesion extends beyond the bone limits.
Today, osteoblastoclastoma is rarely considered a benign tumor: it is classified as an aggressive neoplasm, primarily due to its unpredictability and high probability of malignancy.
Symptoms osteoclastomas
Clinical manifestations in childhood and old age are almost the same. The first signs are not immediately detected, since at first osteoblastoclastoma develops latently, and it can be identified only almost a year after the onset of development.
Experts divide the symptoms into general and local. General signs usually accompany malignant osteoblastoclastoma, and local ones are present in benign neoplasms.
General symptoms do not depend on the location of the affected bone:
- severe pain in the area of tumor growth;
- palpation crunching, indicating the growth of the neoplasm and destruction of the bone segment;
- the appearance of a network of vessels above the pathological focus;
- a steady increase in bloating;
- increasing pain as the tumor grows;
- impairment of muscle and joint function near the affected area;
- enlargement of nearby lymph nodes;
- general malaise, fatigue;
- increase in body temperature;
- loss of appetite, weight loss;
- apathy, helplessness.
Local manifestations are "tied" to the location of the affected bone. For example, if osteoblastoclastoma develops in one of the jaws, facial symmetry is gradually disrupted. The patient begins to experience difficulties with speech, chewing, and sometimes teeth become loose and fall out. In severe cases, necrotic areas and fistulas are formed.
90% of giant cell tumors exhibit a typical epiphyseal location. The tumor often extends into the articular subchondral bone or even abuts the cartilage. The joint and/or its capsule are rarely involved. In the rare case where an osteoclastoma occurs in a child, the lesion is most likely to be in the metaphysis. [ 6 ], [ 7 ] The most common sites in descending order are the distal femur, proximal tibia, distal radius, and sacrum. [ 8 ] 50% of osteoclastomas arise in the knee region. Other common sites include the fibular head, proximal femur, and proximal humerus. Pelvic localization is rare. [ 9 ], [ 10 ] Multicentricity, or the synchronous appearance of osteoclastoma in different skeletal sites, is known to occur but is extremely rare. [ 11 ], [ 12 ]
If osteoblastoclastoma develops in the legs, the patient's gait changes, over time the muscles of the damaged lower limb atrophy, walking becomes difficult. In some cases, dystrophic bone processes occur, the bone becomes thinner. Pathological fractures occur, accompanied by severe pain syndrome and tissue swelling. Complications in the form of hemorrhages, hematomas, and necrosis of soft tissues may occur.
If osteoblastoclastoma develops in the area of the humerus or femur, then the motor skills of the finger phalanges and the overall function of the affected limb are impaired.
When the tumor process becomes malignant, the patient's condition worsens. The following signs are noteworthy:
- pain in the affected area of the bone increases;
- the neoplasm is steadily growing;
- bone tissue is destroyed, the area of such destruction expands;
- the tumor focus loses its clear boundaries;
- the cortical layer is destroyed.
Only a specialist can see such changes when performing instrumental diagnostics.
Benign osteoblastoclastomas are characterized by a gradual latent or asymptomatic course. Pain syndrome occurs only during the progression of the pathology; after several months, the patient begins to experience radiating pain. In many patients, the first indication of the disease is a pathological fracture. At diagnosis, about 12% of patients with osteoclastoma currently have a pathological fracture. [ 13 ], [ 14 ] It is believed that the presence of a pathological fracture indicates a more aggressive disease with a higher risk of local recurrence and metastatic spread. [ 15 ]
When osteoblastoclastoma becomes malignant, the previously barely noticeable tumor becomes painful, and signs of irritation of the nerve endings are detected. If the neoplasm is primarily malignant, then there is severe, debilitating pain, with a rapidly increasing neurological picture.
Osteoblastoclastoma in children
The clinical signs of different forms of benign osteoblastoclastoma are often different. Cystic forms do not manifest symptoms for a long time, and in 50% of cases are detected only after the development of a pathological fracture. The tumor process is detected with severe intraosseous tissue proliferation, with the occurrence of pain syndrome. The protrusion of a bone section occurs only with pronounced proliferation: the patient has an expanded venous network, limited joint mobility. The lytic form of osteoblastoclastoma is characterized by faster growth, early onset of pain, but contractures occur less frequently.
Most often, in childhood, osteoblastoclastoma affects the upper metaphyses of the humerus and femur. Less often, lesions are found in the lower femoral metaphysis, tibia and fibula. In the lytic form, destruction of the epiphyseal cartilage is possible with further spread to the epiphysis, without penetrating the joint (the articular cartilage remains intact). In the active cystic form, tumor growth is noted in the central part of the diaphysis, with a sharp thinning of the cortical layer and bone swelling.
Osteoblastoclastomas in childhood are mostly benign, but they can also provoke significant bone destruction. When the epiphyseal cartilage grows, the growth of the limb area slows down, pathological fractures, pseudoarthrosis with a pronounced bone defect and pain syndrome can occur.
In a malignant process, a neoplasm of the osteogenic sarcoma type is formed: rapid growth and pronounced bone destruction are characteristic. For differential diagnosis, children undergo a histological examination.
Stages
Experts distinguish between the lytic and cellular-trabecular stages of osteoblastoclastoma development.
- The cellular-trabecular stage is characterized by the formation of foci of bone tissue destruction separated by partitions.
- The lytic stage is characterized by the formation of a continuous destructive focus, which is localized asymmetrically relative to the central bone axis. As the neoplasm grows, it can spread to the entire bone cross-section.
A typical sign of osteoblastoclastoma is the separation of the destructive focus from the healthy part of the bone. The bone marrow canal is separated from the neoplasm by a closing plate.
Forms
Depending on the clinical and radiological information and morphological features, the following basic types of osteoblastoclastoma are distinguished:
- The cellular type is found mainly in middle-aged and elderly patients. The neoplasm develops slowly, eventually revealing itself as a dense swelling with a nodular surface, without the possibility of limiting it from healthy bone. When localized in the jaw area, the latter acquires a spindle-shaped form. The position of the teeth does not change. The tissue covering the cellular osteoblastoclastoma has an anemic character. Radiographically, a shadow from a large number of cystic and cellular formations, separated from each other by barriers, is distinguished. There is no reaction from the periosteum.
- The cystic form of osteoblastoclastoma initially causes painful sensations. When palpating the tumor, some areas are pliable, and the symptom of "parchment crunch" is noted. The bone above the neoplasm becomes thinner, has a smooth, convex, dome-shaped form. On the radiograph, the lesion resembles an odontogenic cyst or ameloblastoma.
- The lytic type of pathology is relatively rare, mainly in children and adolescents. The neoplasm grows quite quickly. Against the background of thinning of the cortical layer, pain appears: at first they begin to bother at rest, then - when palpating the affected area. Expansion of the vascular network above the tumor site is noted. When the pathological focus is localized in the jaw area, the teeth become crooked and loose. Pathological fractures are possible. An unstructured zone of enlightenment is present on the radiograph.
According to the degree of malignancy, osteoblastoclastoma is divided into benign (without cellular atypism), primary malignant and malignant (transformed from a benign tumor).
Depending on the localization, the following types of pathology are distinguished:
- The peripheral form of osteoblastoclastoma on the upper jaw does not have any special morphological features and is located on the gums.
- The central form is located inside the bone structure and, unlike the peripheral form, has hemorrhagic zones, which cause the brown tint of the neoplasm. The tumor is represented by one conglomerate.
- Osteoblastoma of the lower jaw is located in the thickness of the bone tissue, in the area of the molars and premolars. The growth of the neoplasm occurs over several years (on average - 3-10 years), accompanied by a violation of the function of the temporomandibular joint.
- Osteoblastoclastoma of the upper jaw manifests itself by the appearance of a protrusion of the affected jaw area, loosening of teeth, and facial asymmetry. The tumor grows slowly and painlessly.
- Osteoblastoclastoma of the femur is the most common localization, with damage to the bone growth zone: the greater trochanter, neck and head of the femur. Less often, the lesser trochanter is affected (isolated). The pathology is accompanied by pain, bone deformation, pathological fractures.
- Osteoblastoclastoma of the ilium most often develops at its base. It is also possible to affect the Y-shaped cartilage with destruction of the horizontal branch of the pubic bone or the descending branch of the ischium. The pathology is initially asymptomatic, then pain appears during exertion, lameness.
Complications and consequences
The most unfavorable consequence of benign osteoblastoclastoma is its malignancy, or malignancy. Malignant giant cell tumor is rare; an analysis of studies revealed a frequency of 1.6% of primary malignancies and 2.4% of secondary malignancies. Infiltrative growth is detected, the nearest lymph nodes are affected, and metastasis may spread. [ 16 ]
Malignant giant cell osteoblastoma is capable of producing the following types of metastases:
- hot (rapidly developing, actively destroying surrounding tissues);
- cold (without specific development, existing for a long time in an inactive state, but having the ability to transform into “hot”);
- mute (existing in a state of anabiotic anabiotic and detected by chance).
Malignant osteoblastoclastoma can occur in three variants:
- A primary malignant tumor retains its basic type of structure, but there is atypicality of mononuclear elements and the presence of mitosis in them.
- Malignancy of a primarily benign tumor with the development of spindle cell or osteogenic sarcoma.
- Malignancy after previous treatment, particularly after non-radical interventions or irrational radiation therapy. In such a situation, polymorphic cell sarcoma with pulmonary metastasis most often develops.
Malignant osteoclastoma is generally considered to be a high-grade sarcoma; [ 17 ] however, data from studies suggest that malignant osteoclastoma behaves like a low- or intermediate-grade sarcoma. [ 18 ] Metastasis occurs in 1–9% of patients with osteoblastoclastoma, and some earlier studies have correlated the incidence of metastasis with aggressive growth and local recurrence. [ 19 ], [ 20 ]
After surgical interventions, patients with limited or lost ability to work are assigned the appropriate disability group.
Diagnostics osteoclastomas
To diagnose osteoblastoclastoma, it is necessary to use the following methods:
- questioning the patient, careful examination and palpation of the affected area of the bone, study of the anamnesis;
- laboratory and instrumental diagnostics, morphological studies.
When determining the anamnesis of the pathology, the doctor pays attention to the first manifestations of the tumor, the presence and nature of pain, previous illnesses and injuries, previous treatment, and the general condition. It is also important to clarify the condition of the urinary, reproductive, respiratory systems, liver and kidneys, lymph nodes, and to perform an ultrasound diagnosis of the internal organs.
Absolutely all patients are prescribed blood and urine tests, determining protein and fractions, sialic acids, phosphorus and calcium. It is necessary to determine the enzymatic activity of phosphatases, conduct a diphenyl test, evaluate C-reactive protein, etc. It should be noted that laboratory indicators for bone tumors are usually non-specific, but can help in differential diagnostics. For example, with malignant osteoblastoclastoma, such changes as leukocytosis, accelerated ESR, decreased blood protein and non-hemoglobin iron, increased sialic acids and alkaline phosphatase are possible. Oxyproline and hexokinase appear in the urine. Phosphorus and calcium levels increase in the blood serum.
Conventional studies for suspected osteoblastoclastoma include general and targeted X-rays, tomography. The X-ray allows for more precise localization, scale, and nature of the disease process, and for determining its spread to surrounding organs and tissues. Computer tomography allows for the examination of deep pathological destruction and the determination of the size of the lesion within the bone. However, magnetic resonance imaging is considered more informative: based on the information obtained during the study, doctors can assemble a spatial image, including a three-dimensional picture.
During the morphological examination, the material obtained during aspiration and trepanobiopsy, or the removed bone areas together with the osteoblastoclastoma, is studied. Puncture biopsy is performed using special needles, and the tumor is punctured under X-ray observation.
During the X-ray examination of long tubular bones, patients are found to have an osteolytic destructive focus, localized in an eccentric manner in the epiphysis region. In dynamics, the pathology diverges toward the articular cartilage, as well as to the bone metaphysis, and can occupy the entire cross-section (which is typical for osteoblastoclastoma of the head of the fibula and radius). The cortical layer is greatly thinned, swollen, and partial destruction is often detected. In a benign process, there is no periosteal reaction. The boundary between the neoplasm and the spongy substance is blurred, there is no clarity. In the overwhelming majority of cases, the sclerotic border is absent.
In cases of spinal cord damage, the tumor is located in the vertebral body in 80% of cases. The body with the arch and processes may be affected, sometimes several vertebrae, costal sections, and the sacroiliac joint are involved in the pathological process. Destructive foci may have a cellular or lytic structure.
When studying layered images on CT, destruction of the arc with transverse processes is determined, which cannot be seen on a regular X-ray. The use of MRI allows us to examine the effect of the tumor on the spinal cord. [ 21 ], [ 22 ]
Primary malignant osteoblastoclastoma is defined on the radiograph as a lytic destructive focus with blurred boundaries. In some cases, the structure is coarse-meshed. There is "swelling" of the affected bone area, severe thinning of the cortical layer with its subsequent destruction. The cortical plate is heterogeneous from the inside. Periosteal reaction is possible.
In malignant transformation of initially benign osteoblastoclastoma, a large-mesh, small-mesh or lytic structure of the destructive focus is revealed. The affected bone area is "swollen", the cortical layer is very thin, with uneven outlines on the inner side. Cortical destruction is possible. The periosteal reaction (weak Codman's peak) has the character of bulbous periostitis.
To detect possible metastasis, sonography is prescribed to help study the condition of internal organs.
The final stage of bone tumor diagnostics is histological identification and cytological examination of smears. The material is taken by biopsy (open or puncture).
Differential diagnosis
Benign osteoblastoclastomas require differentiation from all pathologies that show signs of a bone cyst or tissue lysis on radiographic imaging. Such pathologies include:
- fibrous dysplasia;
- lytic osteogenic sarcoma;
- parathyroid osteodystrophy;
- focus of bone tuberculosis;
- aneurysmal bone cyst.
If there are large and progressive bone lesions, osteoblastoclastoma should be suspected. This tumor is characterized by the absence of surrounding bone osteoporosis, a destructive process from the metaphysis, and late penetration of pathology into the epiphysis.
It is possible to differentiate parathyroid osteodystrophy from osteoblastoclastoma only using radiography and biochemical studies.
Difficulties may arise during the diagnosis of osteoblastoclastoma of long tubular bones, as well as when differentiating the disease from osteogenic sarcoma or cystic formations (bone or aneurysmal).
The localization of an aneurysmal cyst is mainly the diaphysis or metaphysis. With an eccentric localization of such a cyst, local bone swelling is noted, a thin cortical layer: the neoplasm is stretched along the bone, it may contain calcareous particles. With a central localization, the metaphysis or diaphysis swells symmetrically, which does not happen with osteoblastoclastoma.
In childhood, osteoblastoclastoma can be confused with the monostotic type of fibrous osteodysplasia. In this situation, the bone is deformed, shortened (sometimes lengthened), but does not swell, as in osteoblastoclastoma. Fibrous osteodysplasia mainly affects the metaphysis and diaphysis of tubular bones. The cortical layer can thicken, sclerotic areas are formed around the destruction zones. The development process is painless, slow.
If osteoblastoclastoma affects the lower jaw, the pathology should be differentiated from odontoma, bone fibroma, adamantinoma, and dentigerous cyst.
Who to contact?
Treatment osteoclastomas
The goal of treatment is to minimize morbidity and maximize the functionality of the affected bone; traditionally, this treatment was performed by intralesional curettage with packing of the cavity. Newer techniques such as cementation using bone cement are encouraging as they aid in reconstruction and reduce local recurrence.[ 23 ]
The only way to completely get rid of osteoblastoclastoma is through surgery: the tumor is removed, preventing further damage to the bone.
Small osteoblastoclastomas are carefully scraped out using a special curette. The resulting bone defect is replaced using autotransplantation. In case of large tumor sizes, bone resection is performed followed by plastic surgery. [ 24 ], [ 25 ], [ 26 ]
Due to the high rate (25-50%) of local recurrence after curettage and bone grafting, surgeons have been encouraged to improve their surgical procedures by using chemical or physical adjuvants such as liquid nitrogen, acrylic cement, phenol, hydrogen peroxide, local chemotherapy or radiotherapy.[ 27 ],[ 28 ] Local adjuvant therapy has been shown to help control the recurrence rate.[ 29 ]
If for some reason the patient is contraindicated for surgical intervention, then he is prescribed radiation therapy. With the help of radiation, it is possible to stop the growth of the neoplasm and destroy its structure. [ 30 ]
It is also possible to use the following techniques:
- Intralesional administration of steroid drugs. This method is relatively new and has not been used for very long. By means of injections, it is possible to achieve positive results with small osteoblastoclastomas: the tumor decreases in size. Sometimes, at the end of treatment, the lesion becomes more radiopaque compared to the surrounding bone area.
- Introduction of alpha-interferon. Based on the theory of the vascular origin of osteoblastoclastoma, specialists have introduced into practice the injection of alpha-interferon. This drug has an antiangiogenic ability - that is, it slows down the growth of blood vessels. This method has become effective in about 50% of patients, but it is used relatively rarely, which is due to the large number of side effects - such as headaches, general deterioration in health, severe fatigue and impaired ability to work.
For the treatment of malignant (primary or secondary) osteoblastoclastoma, only surgical intervention is used, which includes tumor resection together with the bone area. Before and after the operation, the patient is prescribed radiation and chemotherapy.
Inoperable osteoclastomas (eg, some sacral and pelvic tumors) can be treated with transcatheter embolization of their blood supply.
- Anti-RANKL therapy
Giant cells overexpress a key mediator in osteoclastogenesis: the RANK receptor, which in turn is stimulated by the cytokine RANKL, which is secreted by stromal cells. Studies of denosumab, a monoclonal antibody that specifically binds to RANKL, have yielded impressive treatment results, leading to its approval by the US Food and Drug Administration (FDA). [ 31 ], [ 32 ] Denosumab is primarily intended for patients at high risk of recurrence after initial surgery and local recurrence.
Surgical treatment
Various studies show that wide resection is associated with a reduced risk of local recurrence compared with intralesional curettage and may increase recurrence-free survival from 84% to 100%.[ 33 ],[ 34 ],[ 35 ] However, wide resection is associated with a higher rate of surgical complications and results in functional impairment, which usually requires reconstruction.[ 36 ],[ 37 ],[ 38 ]
If osteoblastoclastoma is localized in long tubular bones, the following surgical interventions may be used:
- Marginal removal with allo or autoplasty is performed for benign osteoblastoclastoma, slowly developing, with a cellular structure, located on the periphery of the epimetaphysis. Fixation with metal screws is possible.
- If the tumor process extends to the diametrical middle of the bone, 2/3 of the condyle and part of the diaphysis with the articular surface are removed. The defect is filled with a cartilaginous allograft. Strong tie bolts and screws are used. The connection of the allograft and the cortical layer of the host bone is performed obliquely, in order to avoid joint subsidence.
- If the epimetaphysis is destroyed or there is a pathological fracture, then segmental resection with joint disarticulation and replacement of the defect with an allograft is performed. Fixation with a rod on cement.
- In case of pathological fracture and malignancy of osteoblastoclastoma in the proximal part of the femur, total hip replacement surgery is performed.
- When removing the articular end segments of the knee joint, an allo-hemiarticular transplant is used with strong fixation. Individual total endoprosthetics with a titanium extended stem and subsequent radiation therapy are possible.
- If the aggressive tumor is localized in the area of the distal end of the tibia, resection with osteoplastic arthrodesis of the ankle is performed. In case of damage to the talus, bone extirpation with lengthening arthrodesis according to Zatsepin is used.
- If the pathological focus is localized in the cervical spine, anterior access to the vertebrae is practiced. Anterolateral access is possible with careful separation of the pharynx and the anterior side of the vertebrae to the cranial base.
- At the level of Th 1 -Th 2, anterior approach with oblique sternotomy to the third intercostal space is used. The vessels are carefully shifted downwards. If the lesion is located in the 3-5 thoracic vertebrae, an anterolateral approach and resection of the third rib are performed. The scapula is shifted backwards without cutting off the muscles. Difficulties may arise when accessing the anterior surfaces of the upper sacral vertebrae. An anterolateral retroperitoneal right approach is used, with careful separation of the vessels and ureter.
- If severe destruction of the vertebrae is detected, or the spread of the tumor to the arches in the thoracic and lumbosacral spine, transpedicular-translaminar fixation is performed with removal of the affected vertebrae and autoplasty.
- If osteoblastoclastoma is located in the pubic and ischial bones, the affected area is removed within the boundaries of healthy tissues without bone transplantation. If the bottom and roof of the acetabulum are affected, removal with subsequent bone-plastic replacement of the defect is indicated.
- If the sacrum and L5 are destroyed, the affected parts are removed posteriorly and stabilized using transpedicular fixation. The neoplasm is then removed retroperitoneally with subsequent bone grafting.
Prevention
There are no specific preventive measures to prevent the occurrence of osteoblastoclastoma. For prevention purposes, specialists recommend regularly undergoing X-ray examination every 1-2 years to promptly detect such tumors and treat them.
If a person discovers any bone compaction, he or she must immediately consult a doctor: a therapist, orthopedist, oncologist, traumatologist, or vertebrologist.
Additional medical recommendations include:
- avoid injuries, intoxications, eat properly and nutritiously, be physically active;
- consult a doctor in a timely manner, including regarding diseases of the musculoskeletal system;
- Be sure to visit a doctor and undergo a diagnostic examination if any new growth of unknown origin appears.
Forecast
In patients with osteoblastoclastoma, the outcome of the disease depends on many factors, such as the characteristics of the tumor development, its malignancy or benignity, localization, spread, timeliness of treatment, etc. In recent years, the results of treatment of malignant bone tumors have become much more progressive. Doctors use a combined approach, if necessary, using intensive polychemotherapy. At the same time, the percentage of completely recovered patients is more than 70%.
Experts say that the prognosis is positive if the osteoblastoclastoma is completely removed surgically and there are no relapses. Whenever possible, surgeons always try to perform organ-preserving operations with simultaneous bone grafting, and only in some cases is it a question of mutilating interventions, after which a person can no longer perform certain actions: they have to change their lifestyle. In such situations, doctors understand the term "recovery" as "the absence of tumor processes." Such patients require subsequent long-term rehabilitation, orthopedic, and sometimes psychological assistance.

