Medical expert of the article
New publications
Osteoarthritis
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The combined term "arthroso-arthritis" literally means that a person against the background of articular arthrosis develops an additional pathology - an inflammatory process in the form of arthritis of the same joint. The disease is complex, since it includes simultaneously destructive and inflammatory pathogenetic mechanism. Treatment of such pathology should be as comprehensive as possible, using, among other things, physiotherapy.
Often the diagnosis of osteoarthritis is made in patients with an acute stage (exacerbation) of osteoarthritis.
Epidemiology
Osteoarthritis is a fairly common disease, which is diagnosed in about 5-10 people out of a hundred, and this is not an insignificant figure. In addition, over the last decade, there has been an annual increase in the incidence of the disease. Although many experts believe that these figures do not reflect the real statistical picture, as not all patients with arthritis seek medical help.
At the age of 20 to 40 years, pathology is more often detected in men, and at the age of 40-60 years - in women. After 60 years of age, the incidence rate is approximately the same, regardless of gender.
Large joints are most often affected: knee, hip, shoulder joints. Small joints are affected mainly in people who, due to their profession, are forced to perform monotonous movements of the upper limb, hand and fingers. In this situation, metacarpophalangeal joints are mainly affected.
Causes of the arthritis
The basis for the development of osteoarthritis is the impact of pathological load on the joint and its inability (for one reason or another) to resist it. To put it differently, the joint can suffer under the influence of age-related changes, intense load, lack of nutrition, which leads to damage, thinning of cartilage, displacement and destruction of bone elements. Further to the already formed osteoarthritis is joined by an inflammatory reaction - arthritis.
For the appearance of inflammation is often enough trivial hypothermia, a sharp change in weather conditions, traumatic injury, infectious lesions, stress, etc.
Infectious-caused disease more often occurs due to acute respiratory infections or acute respiratory viral infections, inflammation of the lungs, infection of the urinary system. If a person has weak immunity, the pathogen easily settles in degeneratively altered tissues.
Sometimes it is a specific type of pathogen - for example, tubercle bacillus, pale treponema, brucella, and so on.
Traumatic arthritis-arthritis is provoked by acute trauma (fracture, open joint injury, etc.) or chronic trauma (sports overload, professional "habitual" exposure), as well as reconstructive interventions (in particular, surgical, dental).
Risk factors
The underlying factors for the development of combined osteoarthritis-arthritis may be as follows:
- Older age. It is believed that with age, the risks of joint problems increase significantly. In women, the disease is more likely to develop after 50-55 years of age.
- Harmful habits. Smoking, alcohol abuse, drug use contribute to the problem.
- Toxic effects (occupational, alcohol intoxication).
- Errors in nutrition (incomplete, monotonous diet, consumption of unhealthy food).
- Obesity.
- Hypodynamia, lack of physical activity.
- The presence of pathologies caused by allergies and autoimmune processes (scleroderma, bronchial asthma, systemic lupus erythematosus, pollinosis, glomerulonephritis, etc.).
- Traumatic joint injuries.
- Excessive stress on the joint, sports and occupational overload.
- Chronic infections.
- Neuropathology, metabolic disorders, endocrine disorders (diabetes mellitus, thyroid disease).
- Congenital joint abnormalities.
- Diseases of the musculoskeletal and cardiovascular system (including varicosis, thrombophlebitis).
- Undergone surgical interventions on joints.
Pathogenesis
Under the influence of the above etiologic factors, there is relatively early or accelerated wear and tear of joint elements such as cartilage, bone-tendon-complementary segments, capsule, tendons, and ligaments.
Metabolic processes are disturbed, the properties and quantity of collagen and elastic fibers, chondrocytes and synovial fluid deteriorate. Cartilage loses its elasticity: at first there is roughness in the center, areas of disintegration, micro-damage, then the underlying bone tissue is exposed. The cartilage layer then gradually disappears altogether.
Significant deterioration of the shock-absorbing abilities of the joint is closely associated with the formation of subchondral osteosclerosis. Zones of ischemia and sclerotic changes are formed. At the same time, there is compensatory cartilage overgrowth at the borders of the articular surfaces of the epiphyses, osteophytes are formed - ossified areas along the edges. The joint capsule undergoes fibrous changes.
If autoimmune processes occur in the patient's body, they activate catabolic disorders, as a result of which the cartilage tissue of the joint is damaged.
These pathological changes lead to increased vulnerability of the affected joints. Any infectious or traumatic process can cause the development of arthritis, an inflammatory complication of already developed osteoarthritis.
Symptoms of the arthritis
The first signs of arthroso-arthritis are usually as follows: periodically increasing, then subsiding pain, a feeling of short-term stiffness in the morning, impaired functionality of the affected joint. Pain increases gradually, there is crepitation and stiffness. As the pathological process worsens, there is atrophy of the surrounding muscles, and the joint itself slightly enlarges and changes shape, which is especially noticeable on the supporting joints.
The pain is mechanical in nature - that is, it tends to increase with physical activity and subside in a calm state. The development of an inflammatory reaction is indicated by an unexpected increase in pain syndrome, the appearance of "night" pain, swelling, swelling, redness, local and general increase in temperature.
The increase in joint volume is due to both proliferative changes and the development of inflammation and edema of periarticular structures.
Patients often complain of intra-articular crepitation (crunching, crackling, squeaking) during movements.
The course of arthrozo-arthritis is more often slowly progressive, with periodic relapses and increasing clinical and radiologic picture, aggravation of functional disorders.
- Osteoarthritis of the knee joint is often manifested by the so-called "starting" pain, which begins to bother you while walking (and is especially evident when walking down stairs). The pain is in the antero-internal part of the knee, sometimes radiating to the thigh or ankle joint, and worsens when trying to bend the knee. Many patients show weakening and atrophy of the quadriceps muscle, pain when probing the area of the articular gap or periarticular areas. Virtually every second patient has knee articulation curvature with "turning" it outward against the background of joint instability.
- Arthrosis-arthritis of the ankle joint has signs similar to the pathology of the knee. The ankle increases in volume, mobility is partially limited, the patient begins to limp when walking. Prolonged standing position is also uncomfortable.
- Arthrosis-arthritis of the shoulder joint is characterized by an initial inflammatory lesion of soft tissues: ligaments, tendons, muscles, vascular bed. Due to increasing trophic disorders, the wear of the cartilage layer accelerates, the pathological process spreads to the bone tissue, joint deformation occurs.
- Osteoarthritis of the hip joint at the initial stage of development can be manifested by pain not in the affected joint, but in the knee, outer part of the thigh, buttocks, lumbar region. This greatly complicates the diagnosis. At the same time, motor restriction is detected, pain when trying to rotate inward, when probing the groin area lateral to the pulsation site of the femoral artery. With long-standing arthroso-arthritis, atrophy of the femoral and gluteal muscles, forced position of the affected limb can be observed. At the same time there may be compensatory curvature of the lumbar spine, pelvic lateral tilt and scoliosis, which together provoke the appearance of spinal pain. The patient's gait changes and lameness is formed.
- Osteoarthritis of the toes more often affects women, especially those who have reached menopause. In many cases, this disease is not due to any obvious cause - that is, it is considered idiopathic. The main symptoms are pain and burning when walking, "uncomfortable" shoes that used to be comfortable.
- Arthritis of the metatarsophalangeal joints of the foot usually affects several joints at the same time, most often in the area of the first and third toes. Nodular seals are formed, painful when palpated. While standing or walking, patients note unpleasant tingling, numbness, burning. During periods of remission, the discomfort almost completely disappears, but eventually resumes.
- TMJ arthroso-arthritis is a lesion of the lower jaw, which is characterized by severe pain when trying to move it. Pathology more often develops as a result of infection or trauma to the dentoalveolar mechanism. In addition to pain, patients indicate difficulties with chewing and opening the mouth, increased body temperature during periods of exacerbation of the disease, irradiation of pain to the ear area.
- Osteoarthritis of the wrist joint is usually caused by thinning of the cartilage layer in the area of the joint. The main complaints of patients are regularly worsening pain and limitation of mobility associated with the pain syndrome. Swelling of tissues is possible.
- Osteoarthritis of the elbow joint at the stage of exacerbation is accompanied by pain, motor stiffness and fever. Among other symptoms: swelling of the affected joint, general deterioration of health, weakness, localized redness of the skin.
- Arthritis arthritis of the hand joints during a relapse manifests itself with acute pain, swelling and redness, fever. In the period of symptom subsidence, residual phenomena in the form of pain against the background of hypothermia of the hands, morning stiffness of the fingers, crunching of small articulations. It is possible formation of nodular elements in the area of the lesion. As the disease progresses, articular cartilage is destroyed, bones are fused and deformed.
- Arthritis of the acromial-clavicular joint is initially manifested by a slight discomfort and occasional aching pain in the affected shoulder. At further stages of the disease, a person almost completely loses mobility in this area. In addition, during relapses, all signs of the inflammatory process - arthritis - are detected.
Osteoarthritis of the spinal column reveals itself with a feeling of heaviness in the affected area of the back during active loading, or against the background of prolonged immobility. Over time, begins to bother the aching pain syndrome, prone to intensification with movements. There is crunching, motor stiffness.
Stages
In the radiological aspect, it is customary to distinguish such stages of pathology development:
- There are questionable radiologic manifestations - in particular, the articular gap is not narrowed, or the narrowing is insignificant, but small small osteophytic elements on the edges of the articular surfaces are detected.
- Manifestations are present, but to a minimal extent: the articular gap is slightly narrowed, single osteophytic elements on the edges of the articular surfaces are detected.
- The signs are moderate: the gap is narrowed, the osteophytes are more pronounced, manifestations of subchondral osteosclerosis are present, and the articular surfaces are slightly curved.
- The manifestations are clearly expressed, the gap is narrowed, osteophytes are multiple and large, bone epiphyses are deformed.
Degrees
- Osteoarthritis of the 1st degree is characterized by increasing pain during physical activity, and their disappearance during rest. When the joints of the lower extremities are affected, pain appears even when standing or walking for a long time. When the shoulder joint is affected, crunching may occur, and pain appears against the background of withdrawal of the arm to the extreme position. Motor restriction is not observed.
- Osteoarthritis of the 2nd degree is characterized by moderate pain, possible lameness (if the joints of the lower extremities are affected), muscle hypotrophy. When the shoulder is affected, pain appears if you raise the arm above the shoulder girdle, or after prolonged motor activity. Motor ability is moderately limited.
- Osteoarthritis of the 3rd degree is accompanied by an increased risk of fractures due to structural disorders of the bone. Pain is sharp, more often constant (even at rest), there is lameness and joint instability, muscle atrophy, limited passive movements.
Forms
Arthrozo-arthritis is classified according to a number of signs. Separately distinguish the degrees of pathology. In addition, the disease is age-related (caused by age-related changes), as well as traumatic and pathological (due to injuries or joint diseases).
Osteoarthritis can have a chronic slow course, or progressive, in which the affected joint is destroyed in as little as 2-3 years.
Also the pathology is subdivided, depending on the localization:
- Gonarthrosis arthritis is a lesion of the knee joint;
- Coxarthrosis arthritis is a lesion of the hip joint;
- Uncovertebral arthroso-arthritis is a lesion of the cervical spinal column;
- Vertebral arthroso-arthritis is a lesion of the vertebral column;
- Patellofemoral arthritis-affects the patella and part of the femur.
Complications and consequences
Osteoarthritis is characterized by slow progression. Treatment allows you to slow down the process and permanently preserve the patient's motor capabilities. If the doctor's prescriptions are ignored, complications and unfavorable consequences may develop:
- Severe curvature of the affected joint;
- Deterioration of motor function to the point of complete loss of movement;
- Shortening of the affected limb (in particular, this often happens in arthritis of the hip or knee);
- Bone curvatures, deformities of the spine, fingers and limbs.
Ultimately, the patient loses the ability to work, and in complex cases - becomes unable to move independently and even to self-care. Severe neglected forms of pathology can become an indication for the appointment of the first or second group of disability.
Diagnostics of the arthritis
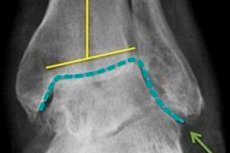
The diagnosis of osteoarthritis is made by an orthopedist based on the clinical picture and the available radiologic findings. Dystrophic changes in cartilage and adjacent bone structures are visible on the radiograph.
There is narrowing of the articular gap, curvature of the bone pad (often flattening), presence of cystic elements, signs of subchondral osteosclerosis and bony outgrowths (osteophytes). Joint instability is possible. If X-ray examination does not reveal pathological changes, or does not allow their identification, additional instrumental diagnostics in the form of computed tomography and magnetic resonance imaging is prescribed. Consultation of specialized specialists, such as endocrinologist, surgeon, rheumatologist, infectious disease specialist, is indicated to find out the root causes of arthritis-arthritis development.
The tests consist of an examination of venous blood:
- General blood analysis with evaluation of leukocyte formula and COE;
- Determination of fibrinogen, antistreptolysin O, uric acid in serum;
- C-reactive protein determination;
- Rheumatoid factor, antinuclear factor on HEp-2 cells;
- Antibodies to extractable nuclear antigen (ENA-screen).
The research methods used are flow cytofluorimetry, capillary photometry, clotting method, immunoturbidimetry, enzymatic colorimetric method, indirect immunofluorescence reaction, and enzyme immunoassay.
Differential diagnosis
In most cases, the diagnosis of osteoarthritis does not cause difficulties. Difficulties arise if the exacerbation of pathology is atypical, or there are no characteristic radiological manifestations (in the early stages of the disease).
The differential diagnosis is primarily performed with such diseases and lesions:
- Gout;
- Rheumatoid, reactive arthritis;
- Streptococcal (rheumatic) polyarthritis;
- Osteoarthritis;
- Metabolic arthropathy;
- Chondrocalcinosis, acute calcifying periarthritis;
- Psoriatic arthropathy.
The first-time onset of arthroso-arthritis should be differentiated with gout and pseudopodagra, arthropathy, septic arthritis, and swelling.
Acute rheumatism of the joints is more often detected in childhood and adolescence. Pathology starts about 14 days after a sore throat, and the manifestations of arthritis are accompanied by cardiac disorders. Blood tests demonstrate an increased titer of antistreptococcal antibodies. Therapy with salicylates has a positive therapeutic effect.
Patients with gout do not have carditis, but uric acid crystals are found everywhere.
In rheumatoid arthritis, slow progression of the disease is noted, the proximal interphalangeal and metacarpophalangeal joints of the hands are affected. There is symmetry of joint involvement, increasing muscle atrophy. Rheumatoid factor is detected.
In psoriatic arthritis, symmetry of the lesions is also noted, psoriatic skin rashes are also characteristic.
Reactive arthritis develops against the background of an infectious disease, or immediately after it. Blood tests reveal an increased titer of antibodies to the infectious agent.
Among other things, differentiation is made with gonorrheic and post-traumatic arthritis, intermittent hydroarthrosis.
Who to contact?
Treatment of the arthritis
The choice of the therapeutic scheme is always left to the attending physician, and is determined by the causes, stage and clinical picture of the disease. Medications (external, oral, injectable), physiotherapy, and if necessary, surgery is involved. In addition, the patient is recommended to adjust nutrition and physical activity to minimize pathological changes in joint structures.
Drug therapy is prescribed to relieve pain syndrome, as well as to restore the affected tissues and inhibit further pathological intra-articular processes.
It is possible to use medications such as:
- Non-steroidal anti-inflammatory drugs (Diclofenac, Indomethacin, Ketorol, both internally and injected and externally);
- Hormonal agents (corticosteroids) - more often in the form of intra-articular injections;
- Antispasmodics and analgesics (particularly Midocalm).
Special drugs with chondroprotective activity have a restorative effect on the joint. They saturate the cartilage tissue with nutrients, inhibit the process of destruction, activate regeneration at the cellular level. The most common representatives of chondroprotectors are chondroitin and glucosamine: treatment with such drugs is long, and the effect depends on both the duration of intake and the timeliness of their appointment.
Selection of this or that medication, dose and duration of the treatment course is carried out by the attending doctor.
Among other conservative treatment methods:
- Intra-articular injections of corticosteroid agents (mainly during periods of exacerbation of arthrozo-arthritis);
- Intra-articular injections of hyaluronic acid (to improve gliding and freedom of movement in the affected joint);
- PRP and cytokine therapy (use of the patient's blood products, with platelet enrichment, to stimulate intra-articular blood circulation and synovial fluid production, to improve trophic processes).
In case of severe damage to the articulation, when drug treatment can no longer be effective, surgical intervention is prescribed.
Drug treatment
|
Diclofenac |
In osteoarthritis, 75 mg (1 ampoule) of the drug is usually administered intramuscularly per day. In severe symptoms, the dose can be increased to 2 ampoules per day (with an interval of several hours), or combined with other dosage forms of Diclofenac (ointments, tablets). Long-term treatment with the drug is not recommended. |
|
Indomethacin |
Take 25-50 mg up to four times a day (in complicated cases - up to six tablets per day). In case of a prolonged treatment course, the daily dose should not exceed 75 mg. |
|
Ketorol (Ketorolac) |
For pain, take up to 90 mg per day, not more than 3-5 consecutive days (preferably during or immediately after meals). |
|
Midocalm |
The drug tolperisone hydrochloride and lidocaine has myorelaxing and analgesic activity, which is relevant for the elimination of muscle spasms in arthroso-arthritis. In the acute period of the disease it is injected intramuscularly 100 mg twice a day. |
|
Chondroitin with glucosamine |
The recommended dose is 1 tablet up to 3 times a day (about 1000 mg of chondroitin sulfate and 1500 mg of glucosamine daily). The average duration of intake is 6 months. |
Nonsteroidal anti-inflammatory drugs can cause adverse renal side effects - in particular, we are talking about the development of acute renal failure, nephrotic syndrome, hyponatremia. However, most often adverse symptoms are associated with erosive and ulcerative lesions of the digestive tract, which are mainly found in the prepyloric part of the stomach and antrum. Many patients have functional digestive disorders, esophagitis, esophageal strictures, gastritis, ulcers and perforations, gastrointestinal bleeding, as well as NSAID-induced enteropathies.
Physiotherapy treatment
Physical therapy is part of additional non-medication treatment and may include the following techniques:
- Shockwave therapy - helps to eliminate bone overgrowths and stimulate blood circulation, through the influence of ultrasonic waves.
- Electromyostimulation - involves electron-pulse action that stimulates muscle contractions.
- Ultraphonophoresis - consists in the action of ultrasound in combination with the application of medication.
- Ozone therapy - involves the use of ozone gas, which has anti-inflammatory, antiseptic, analgesic, immunomodulatory effects.
If indicated, the doctor may prescribe such procedures as laser therapy, phonophoresis, electrophoresis, UHT, magnetotherapy. A set of exercises aimed at improving local metabolism and stimulating blood circulation, strengthening the periarticular muscle corset is developed.
In addition, therapeutic exercise, mechanotherapy (physical therapy with the use of exercise machines), as well as massage and, if indicated, joint traction to minimize the load.
Herbal treatment
The use of medicinal plants has also proven itself in the therapy of arthritis-arthritis. Thanks to herbs, it is often possible to relieve pain, eliminate stiffness and prevent distortion of the diseased joint. Especially popular are such plants as calendula and chamomile flower, St. John's wort, burdock rhizome and comfrey, nettle and hop cones. They are used in the form of decoctions for external and internal use.
Strong anti-inflammatory effect is characterized by the herb cinquefoil, as well as a herbal mixture based on horsetail, fir, yarrow, dandelion, mother and stepmother, plantain and ergot. These plants are used in the form of decoctions and alcohol tincture.
Some herbal remedies can be used without prior preparation. For example, a fresh burdock or horseradish leaf can be applied to a sore joint. Other remedies, however, require special preparation:
- A good therapeutic effect in arthrozo-arthritis has a medicinal infusion of nettle and birch leaves, as well as tricolor violet. To prepare the infusion pour 8 tbsp. Liters of plant matter 500 ml of boiling water, insist under a lid for half an hour. The resulting remedy is drunk during the day instead of tea.
- Prepare a tincture of burdock rhizome, St. John's wort leaves and hop cones: the plants are crushed, pour alcohol (100 ml per 10 g of mixture), kept in a sealed container in a dark place for 14 days. Then the remedy is filtered (passed through several layers of gauze) and used for rubbing sick places, as well as inside (three times a day 1 tbsp. L.).
- Prepare an equivalent mixture of plants such as nettle, birch leaves, willow bark, calendula. One tablespoon of plant mass is poured 500 ml of boiling water, insist for 12 hours, filtered. Drink 100 ml up to three times a day, and also used to prepare baths.
It should be borne in mind that folk remedies, unlike drugs, are not able to produce a rapid therapeutic effect. Therefore, it is necessary to set up for long-term therapy, with medication support prescribed by a doctor.
Surgical treatment
The assistance of a surgeon may be required if conservative methods of therapy for arthritis arthritis are ineffective. Indications include:
- Severe, unrelenting pain that does not respond to analgesics;
- The formation of pustules;
- Increasing joint stiffness to the point of immobility;
- Severe cartilage deformity;
- Severe intra-articular damage.
- The following types of operations are used as standard:
- Endoprosthesis with replacement of the disturbed joint with an artificial analog;
- Arthrodesis with complete immobilization of the joint;
- Osteotomy with partial removal of bone tissue at a certain angle to reduce joint load;
- Debridement - removal of the affected cartilage.
In arthrosis-arthritis of the hip joint and cartilage lesions of the femoral head, along with analgesia and physiotherapy, various types of surgical intervention may be used, including surgical replacement of the damaged joint with an artificial analog.
Osteoarthritis of the knee joint in cases of increasing wear and tear is an indication for the fitting of an artificial prosthesis.
Pins are often recommended for osteoarthritis of the ankle joint.
Arthroscopy, an intra-articular surgery involving several small punctures in the affected area, is one of the most popular minimally traumatic interventions. The intervention allows removal of cartilage elements and osteophytes that impede mobility.
To redistribute the load on the joint that has been deformed, surgical alignment of the joint axis is performed. This technique can temporarily improve the patient's condition, but does not completely eliminate the problem. Endoprosthesis remains the most effective treatment option in many cases.
Prevention
Preventive recommendations are as follows:
- Adhere to an active lifestyle, avoid both excessive overloading of joints and hypodynamia;
- Do exercises every morning, and if possible, systematically go swimming;
- Eat a good and proper diet, control body weight, consume enough calcium and collagen-containing foods;
- Wear comfortable clothes and shoes;
- Avoid monotonous monotonous movements, take more frequent physical breaks in work, prefer active rest to idle time.
If possible, you should not stand for long periods of time, lift too heavy objects, overload the musculoskeletal system in every possible way.
In the diet it is desirable to give up sweets and sugars, alcoholic beverages, too fatty, spicy and fried dishes, as well as large amounts of salt.
It is ideal to prepare a diet based on fish and seafood, dairy products and cereals, vegetable oils and nuts, vegetables, berries, fruits and plenty of greens. We should not forget about water: daily consumption of 1.5-2 liters of water significantly improves the condition and adaptive abilities of the musculoskeletal system.
Forecast
The prognosis for patients with arthritis is considered conditionally unfavorable. Cases of complete disability in this pathology are rare, since in most patients the disease is aggravated only periodically. Although those changes that have already occurred inside the joints are not subject to reverse development. It should be understood that timely referral to doctors, compliance with the recommended motor regimen and rehabilitation norms can prevent further progression of pathology. In addition, we should not forget that in arthrosis-arthritis, periods of relapses due to reactive intra-articular inflammation are interspersed with periods of quiescence, during which the problem practically ceases to bother, or bothers minimally.
The diagnosis of arthritis arthritis is associated with the need to reconsider your lifestyle, diet and physical activity. It is important to refuse sudden movements, carrying heavy loads, as well as other activities accompanied by excessive stress on the joints. Hypodynamia is also contraindicated: motor activity is mandatory, with a minimum load on the articular cartilage, with the predominant work of the periarticular muscle apparatus. Special exercises should first be performed under the supervision of a rehabilitation specialist, then at home. Depending on the localization of the lesion, the following exercises are recommended:
- Moderate walking on level terrain (approaches, half-hour walks);
- Swimming, aquagymnastics;
- Bike trainer;
- Bicycling on flat terrain (15 to 30 minutes daily);
- In the wintertime, skiing.
Other recommended rehabilitation methods include massage, physiotherapy, and spa treatment. In addition, if necessary, orthopedic correction means are used: supinators, elastic bandages and corsets.
In general, arthroso-arthritis does not pose a threat to the life of the patient. But in the absence of treatment, pathology can severely limit freedom of movement, worsen the quality of life. Early and complete therapy allows you to stop the progress of the disease.

