Medical expert of the article
New publications
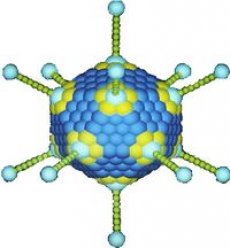
Oncogenic viruses (oncoviruses)
Last reviewed: 08.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
To explain the nature of cancer, two dominant theories have been proposed - mutation and viral. According to the first, cancer is the result of successive mutations of a number of genes in one cell, i.e. it is based on changes that occur at the gene level. This theory was formulated in its final form in 1974 by F. Burnet: a cancerous tumor is monoclonal - it originates from one initial somatic cell, mutations in which are caused by chemical, physical agents and viruses that damage DNA. In the population of such mutant cells, additional mutations accumulate, increasing the ability of cells to unlimited reproduction. However, the accumulation of mutations requires a certain amount of time, so cancer develops gradually, and the probability of the disease depends on age.
The viral-genetic theory of cancer was most clearly formulated by the Russian scientist L. A. Zilber: cancer is caused by oncogenic viruses, they integrate into the cell chromosome and create a cancerous phenotype. For some time, the full recognition of the viral-genetic theory was hindered by the fact that many oncogenic viruses have an RNA genome, so it was unclear how it integrates into the cell chromosome. After reverse transcriptase was discovered in such viruses, capable of reproducing DNA provirus from virion RNA, this obstacle disappeared and the viral-genetic theory received recognition along with the mutation theory.
A decisive contribution to understanding the nature of cancer was made by the discovery of a malignancy gene, the oncogene, in oncogenic viruses, and its precursor, which is present in the cells of humans, mammals, and birds, the proto-oncogene.
Proto-oncogenes are a family of genes that perform vital functions in a normal cell. They are necessary for regulating its growth and reproduction. The products of proto-oncogenes are various protein kinases that phosphorylate cellular signal proteins, as well as transcription factors. The latter are proteins - products of the proto-oncogenes c-myc, c-fos, c-jun, c-myh and cell suppressor genes.
There are two types of oncoviruses:
- Viruses containing an oncogene (one+ viruses).
- Viruses that do not contain an oncogene (one viruses).
- One+ viruses can lose the oncogene, but this does not disrupt their normal functioning. In other words, the virus itself does not need the oncogene.
The main difference between one+ and one" viruses is the following: the one+ virus, having penetrated the cell, does not cause its transformation into cancer or causes it very rarely. One" viruses, having penetrated the cell nucleus, transform it into cancer.
Thus, the transformation of a normal cell into a tumor cell occurs due to the fact that an oncogene, being introduced into the cell chromosome, endows it with a new quality that allows it to reproduce in the body uncontrollably, forming a clone of cancer cells. This mechanism of transformation of a normal cell into a cancer cell resembles the transduction of bacteria, in which a temperate phage, integrating into the chromosome of bacteria, endows them with new properties. This is all the more plausible since oncogenic viruses behave like transposons: they can integrate into a chromosome, move from one region to another, or move from one chromosome to another. The essence of the question is as follows: how does a proto-oncogene transform into an oncogene when it interacts with a virus? First of all, it is necessary to note the important fact that in viruses, due to the high rate of their reproduction, promoters work with much greater activity than promoters in eukaryotic cells. Therefore, when a one" virus integrates into a cell's chromosome next to one of the proto-oncogenes, it subordinates the work of this gene to its promoter. When leaving the chromosome, the viral genome snatches the proto-oncogene from it, the latter becomes a component of the viral genome and turns into an oncogene, and the virus from one - into a one+ virus. When integrating into the chromosome of another cell, such an onc" virus simultaneously transduces the oncogene into it with all the consequences. This is the most common mechanism for the formation of oncogenic (one+) viruses and the beginning of the transformation of a normal cell into a tumor cell. Other mechanisms for the transformation of a proto-oncogene into an oncogene are also possible:
- proto-oncogene translocation, which results in the proto-oncogene being adjacent to a strong viral promoter, which takes control of it;
- amplification of a proto-oncogene, as a result of which the number of its copies increases, as does the amount of the synthesized product;
- The transformation of a proto-oncogene into an oncogene occurs as a result of mutations caused by physical and chemical mutagens.
Thus, the main reasons for the transformation of a proto-oncogene into an oncogene are the following:
- Inclusion of a proto-oncogene into the viral genome and transformation of the latter into a one+ virus.
- The entry of a proto-oncogene under the control of a strong promoter either as a result of viral integration or as a result of translocation of a block of genes in the chromosome.
- Point mutations in the proto-oncogene.
Amplification of proto-oncogenes. The consequences of all these events can be:
- a change in the specificity or activity of the protein product of the oncogene, especially since very often the inclusion of a proto-oncogene in the viral genome is accompanied by mutations of the proto-oncogene;
- loss of cell-specific and temporal regulation of this product;
- an increase in the amount of synthesized protein product of the oncogene.
Oncogene products are also protein kinases and transcription factors, therefore, disturbances in the activity and specificity of protein kinases are considered as initial triggers for the transformation of a normal cell into a tumor cell. Since the protooncogene family consists of 20-30 genes, the oncogene family obviously includes no more than three dozen variants.
However, the malignancy of such cells depends not only on mutations of proto-oncogenes, but also on changes in the influence of the genetic environment on the work of genes as a whole, characteristic of a normal cell. This is the modern gene theory of cancer.
Thus, the primary cause of the transformation of a normal cell into a malignant one is mutations of a proto-oncogene or its falling under the control of a powerful viral promoter. Various external factors that induce the formation of tumors (chemicals, ionizing radiation, UV irradiation, viruses, etc.) act on the same target - proto-oncogenes. They are present in the chromosomes of the cells of each individual. Under the influence of these factors, one or another genetic mechanism is activated, which leads to a change in the function of the proto-oncogene, and this, in turn, gives rise to the degeneration of a normal cell into a malignant one.
A cancer cell carries foreign viral proteins or its own modified proteins. It is recognized by T-cytotoxic lymphocytes and destroyed with the participation of other mechanisms of the immune system. In addition to T-cytotoxic lymphocytes, cancer cells are recognized and destroyed by other killer cells: NK, Pit cells, B-killers, and K-cells, whose cytotoxic activity depends on antibodies. Polymorphonuclear leukocytes; macrophages; monocytes; platelets; mononuclear cells of lymphoid tissue lacking markers of T- and B-lymphocytes; T-lymphocytes with Fc-receptors for IgM can function as K-cells.
Interferons and some other biologically active compounds formed by immunocompetent cells have an antitumor effect. In particular, cancer cells are recognized and destroyed by a number of cytokines, especially tumor necrosis factor and lymphotoxin. They are related proteins with a wide range of biological activity. Tumor necrosis factor (TNF) is one of the main mediators of inflammatory and immune responses in the body. It is synthesized by various cells of the immune system, mainly macrophages, T-lymphocytes and Kupffer cells of the liver. TNFa was discovered in 1975 by E. Carswell and co-workers; it is a polypeptide with m. w. 17 kD. It has a complex pleiotropic effect: it induces the expression of MHC class II molecules in immunocompetent cells; stimulates the production of interleukins IL-1 and IL-6, prostaglandin PGE2 (it serves as a negative regulator of the TNF secretion mechanism); has a chemotactic effect on mature T-lymphocytes, etc. The most important physiological role of TNF is the modulation of cell growth in the body (growth-regulating and cytodifferentiating functions). In addition, it selectively suppresses the growth of malignant cells and causes their lysis. It is assumed that the growth-modulating activity of TNF can be used in the opposite direction, namely, to stimulate the growth of normal cells and suppress the growth of malignant cells.
Lymphotoxin, or TNF-beta, is a protein with a molecular weight of about 80 kDa, synthesized by some subpopulations of T-lymphocytes, and also has the ability to lyse target cells carrying foreign antigens. Other peptides, in particular peptides that are fragments of IgG molecules, such as tuftein (a cytophilic polypeptide isolated from the CH2 domain), Fab, Fc fragments, etc., also have the ability to activate the functions of NK cells, K cells, macrophages, and neutrophilic leukocytes. Antitumor immunity is ensured only through the constant interaction of all immunocompetent systems.
Most people do not get cancer not because they do not develop mutant cancer cells, but because the latter, having developed, are promptly recognized and destroyed by T-cytotoxic lymphocytes and other parts of the immune system before they have time to produce malignant offspring. In such people, antitumor immunity works reliably. On the contrary, in cancer patients, mutant cells are not promptly recognized or destroyed by the immune system, but multiply freely and uncontrollably. Therefore, cancer is a consequence of immunodeficiency. It is necessary to find out which part of the immune system suffers in order to outline more effective ways of combating the disease. In this regard, much attention is paid to the development of cancer biotherapy methods based on the complex and consistent use of modulators of biological and immunological reactivity, i.e. chemical substances synthesized by immunocompetent cells that are capable of modifying the reactions of the body's interaction with tumor cells and providing antitumor immunity. With the help of such modifiers of immunological reactivity, it becomes possible to influence both the immune system as a whole and selectively its individual mechanisms, including those controlling the formation of activation factors, proliferation, differentiation, synthesis of interleukins, tumor necrosis factors, lymphotoxins, interferons, etc., in order to eliminate the state of immunodeficiency in cancer and increase the effectiveness of its treatment. Cases of curing human myeloma with lymphokine-activated killers and interleukin-2 have already been described. The following directions have been outlined in experimental and clinical cancer immunotherapy.
- Introduction of activated immune system cells into tumor tissue.
- Use of lympho- or (and) monokines.
- The use of immunomodulators of bacterial origin (the most effective are LPS and peptidoglycan derivatives) and the products induced by them, in particular TNF.
- Use of antitumor antibodies, including monoclonal ones.
- Combined use of different directions, for example the first and second.
The prospects for using modulators of immunological reactivity for cancer biotherapy are extremely broad.


 [
[