Medical expert of the article
New publications
Upper extremity neuropathy
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

The innervation of the hand is carried out by a whole system of peripheral, that is, located outside the brain and spinal cord, nerves. Their diseases of non-inflammatory genesis (caused by various degenerative and dystrophic processes) are called neuropathy. It is not a separate disease, but is part of a symptom complex of various pathological conditions, therefore, to determine the treatment tactics, it is not enough to establish the fact of the presence of pathology, but it is also necessary to identify the cause of its development. Neuropathy of the upper limbs is not as common as lower limbs, since the legs are innervated by the longest, and therefore the most vulnerable nerve fibers. Degenerative-dystrophic changes in the peripheral nerves often begin with the lower limbs, later the nerves of the arms, trunk, face are involved, although sometimes the nerves of a specific part of the body are immediately affected, in our case - the arms.
Epidemiology
Statistics show that neuropathies of the upper extremities are not so rare. The most common type is the carpal tunnel syndrome, which affects people who, due to their work, are often forced to make flexion movements with the hand. Of all tunnel syndromes, 2/3 of complaints are about this localization. Many professions used to lead to the development of this pathology, and now they are supplemented by the widespread use of computers - both in professional activities and at home. As a result, from 1 to 3.8% of adults on the planet complain of its symptoms every year. There are three to ten women per man. The peak of manifestation is at the age of 40-60 years.

Another vulnerable area of the median nerve is located in the upper third of the forearm, degenerative-dystrophic changes in this part are called the round pronator syndrome. In addition to the above reasons, the development of this syndrome can be caused by the presence of a rare anomaly - the humeral process (Struther's ligament).
Quite often, the function of the ulnar nerve is impaired. This is also facilitated by compression injuries in everyday life, sports and at work.
Tunnel syndromes develop in more than 45% of people engaged in manual physical labor. And in this case, the overwhelming majority of lesions are right-sided (about 83%).
Causes upper extremity neuropathies
The overwhelming majority of isolated degenerative and dystrophic changes in the nerve fibers of the hand occur as a result of banal compression of one (mononeuropathy) or several nerves (polyneuropathy) innervating the upper limb. There are five such nerves: the muscular-cutaneous and axillary, regulating the work of the shoulder and part of the forearm, its upper and lower parts, respectively; the median, ulnar and radial, controlling the work of the hand from the shoulder to the fingers.
Different areas of nerves, located both shallowly under the skin and in the center of the hand, can be pinched. There can be many reasons for such an event – about two hundred.
Perhaps, most often, neuropathies of one of the above nerves or multiple ones arise due to an uncomfortable position in which the working hand is for a long time, monotonous movements performed by one or both hands. And if earlier the working hand of a person engaged in monotonous and heavy physical labor suffered, then with the advent of the computer era, office workers have joined the risk group. The compression nature of neuropathies in half of the cases of its occurrence is associated with professional activity. One of the most common pathologies is carpal tunnel syndrome (associated with compression of the median nerve at the place of its transition to the hand), which affects people who spend a lot of time daily at the computer, tailors, musicians, dentists and other specialists or athletes who perform multiple monotonous flexion movements of the hand.
Also, median nerve neuropathy is often caused by unusually high loads on the wrist, dislocations of the wrist joint and injuries to the forearm.

Cubital tunnel syndrome, associated with monotonous flexion movements in the elbow and compression of the ulnar nerve, is often encountered. The cause of this is the habit of constantly resting the elbow on a hard surface, including in everyday life, for example, when talking on the phone, or bending it while hanging, for example, putting the elbow out the window while driving a car or hanging it over the edge of a table, which again applies to office workers.
Neuropathy of the ulnar nerve manifests itself as Guyon's canal syndrome - in this regard, professions associated with vibration are dangerous; cycling, motorcycle racing; constant reliance on a cane (the innervation of the palmar muscles is affected).

Radial nerve neuropathy can occur due to incorrect arm positioning during prolonged sleep ("sleep paralysis"), in conductors, runners and people involved in activities that require frequent monotonous movements in the elbow bend, in case of fractures of the clavicle and shoulder joint, and the habit of carrying a heavy bag on the elbow bend.
The axillary or radial nerve is damaged by prolonged movement with crutches, etc.
In addition, neuropathies of the upper limbs can be caused by hand injuries - fractures, dislocations, leading to direct damage to nerve fibers, adjacent muscle or bone tissue, blood vessels (lack of nutrition due to circulatory disorders, compression between swollen tissues, injury from sharp edges of broken bones).
Operations involving the nerve in the process of scar tissue formation, development of ischemia, edema; prolonged intravenous infusions; inflammatory diseases - arthritis, bursitis, lymphadenitis, etc.; cervical osteochondrosis; tumors of both the nerve tissue itself, for example, interdigital neuroma, and localized near the nerve, often cause compression or ischemic neuropathy.
 [ 8 ]
[ 8 ]
Risk factors
Risk factors for its development include: frequent hypothermia, physical overexertion, contact with toxic substances, inflammatory complications of infectious diseases, systemic pathologies - endocrine, autoimmune, liver disease, renal failure, deficiency of B vitamins due to alimentary causes or gastrointestinal diseases, vaccinations, heredity, alcoholism, fluctuations in hormonal levels.
 [ 9 ]
[ 9 ]
Pathogenesis
The pathogenesis of peripheral nerve damage is varied, it is always based on a degenerative-dystrophic process caused by compression, metabolic, ischemic disorders, or started as a result of direct trauma (bruise, rupture, cut, puncture) of nerve fibers. The structure of peripheral nerves is similar to an electric wire - nerve cells (axons, neurites) are enclosed in a myelin sheath, resembling an insulator. According to pathogenesis, neuropathy is divided into axonal, when the axons (nerve cells) themselves are destroyed, and demyelinating, when the sheath is subject to destruction.
In cases of pinching, stretching, squeezing, and ruptures, the axon is usually damaged. With minor compression, the anatomical structure of the nerve is preserved, and it is restored fairly quickly and completely. In cases of severe injuries, complete regeneration of the nerve may be impossible even if the myelin sheath is intact.
In the second case, the myelin sheath, which acts as an insulator and conductor, is damaged. In the pathogenesis of demyelinating neuropathy, genetic predisposition, rheumatoid arthritis, various forms of diabetes, liver and kidney dysfunction, and hypothyroidism are considered. Isolated lesions of the nerves of the upper extremities in such pathologies are rare, however, this cannot be completely ruled out. Damage to a single nerve can be caused by tuberculosis, polyarthritis, poisoning with toxic substances, including alcohol and medications.
Symptoms upper extremity neuropathies
Peripheral nerve fibers are divided into motor, sensory and vegetative. Depending on which ones are predominantly affected by pathological changes, such symptoms will prevail in the clinical picture, although isolated damage to one type of fibers is almost never encountered, so various variants of the symptom complex are possible.
Motor neuropathy manifests itself as muscle weakness, lethargy, trembling even with minor physical exertion, convulsions, over time, muscle mass decreases, visually the limb becomes thinner. The patient often finds it difficult to raise his arms up, especially through the sides, his coordination of movements is impaired, it is impossible to hold objects with his fingers.
The first signs of sensory symptoms are tingling in the fingertips, numbness spreading upwards; a feeling that a thick glove is being worn on the hand; pain syndrome from mild discomfort to acute and burning pain (causalgia); loss of sensitivity in the direction from the periphery to the center (first the fingers, then the hand and higher).
Vegetative symptoms – pale skin, pigmentation, marbled skin; cold fingertips even in hot weather; hyper- or hypohidrosis; hair loss on the skin, thinning of the skin in areas with impaired innervation; thickening and delamination of the nails; ulceration of the skin.
Symptoms increase depending on the stage of the disease. Therefore, if any pain, numbness, loss of sensitivity and limitation of motor functions appear, even if there were no injuries, you need to see a doctor.
Damage to one nerve is called mononeuropathy. Types of damage to the nerves of the upper limb are manifested by the following symptoms:
- the musculocutaneous nerve controls the work of the front part of the arm above the elbow; if it is damaged, the functions of the shoulder and elbow joint are impaired;
- damage to the axillary nerve affects the innervation of the dorsal surface of the limb, shoulder abduction and extension of the shoulder joint are impaired;
- when the median nerve is damaged, motor skills and sensitivity are impaired along the entire length of the arm, but most often - the hand, thumb, index and middle fingers;
- neuropathy of the ulnar nerve is manifested by impaired movement of the hand, ring and middle fingers;
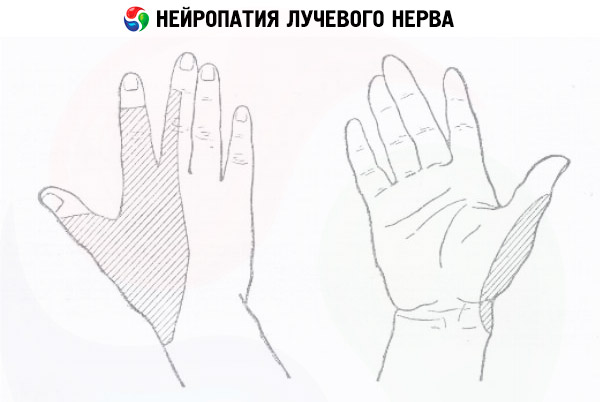
- Radial nerve neuropathy manifests itself as loss of sensitivity on the back of the hand, impaired finger motor skills, and also flexion in the elbow and wrist joints.
The first signs of the most common mononeuropathy of the median nerve - carpal tunnel syndrome are numbness and tingling in the tips of the thumb, index and middle fingers of the working hand in the morning, which passes after a couple of hours and does not remind of itself during the day. Even with such symptoms, you need to seek medical help, because later the hands will begin to go numb at night, and then during the day, it will become problematic to hold objects with the sore hand, it will increasingly lose functions.
The pain sensations are initially tingling or burning, appearing during a night's rest or in the morning. The patient has to wake up and lower the sore arm (the pain goes away from this). At first, one or two fingers hurt, then gradually the whole palm is involved in the process, and even the arm up to the elbow.
The motor skills of the hand are impaired, the fingers, and over time the hand itself, become weaker, and it becomes difficult to hold objects, especially small and thin ones.
In advanced stages of the disease, sensitivity decreases, the affected limb is constantly numb, later it stops feeling touches and even pricks with a sharp object. Atrophic processes occur in the muscles and skin.
Symptoms of ulnar neuropathy also begin with numbness and tingling, localized in the cubital fossa, along the back of the forearm and hand, capturing the ring finger and little finger. Painful sensations in the same localization and motor disorders increase, then loss of sensitivity and muscle hypotrophy - this is the sequence in which cubital tunnel syndrome develops.
With Guyon's canal syndrome, sensations are localized and increase from the palmar surface.
In mild degrees of neuropathy, there are no serious motor or sensory impairments yet, so the likelihood of recovery depends on timely seeking help.
Complications and consequences
As already mentioned, in the initial stages, the sensations of neuropathies are quite tolerable and if you do not pay attention to them, the condition begins to worsen. The muscles hypertrophy, the hand works worse and worse.
Without treatment, the process can end in irreversible muscle tissue atrophy. Visually, the limb decreases in volume, the hand is deformed and becomes similar to the palm of a primate - flat, with the thumb pressed against it.
Sometimes, with partial damage to the median nerve, and even more rarely, the ulnar nerve, causalgia syndrome develops. This is how injuries become complicated when, at the moment of wound scarring, the afferent receptors of nerve cells are irritated, which leads to intense, simply unbearable pain. Of course, in such a state it is impossible not to seek help. Causalgia appears approximately on the fifth day after the injury, and sometimes a little later, for example, after two weeks.
Axonal neuropathy is characterized by slow development and a long course. Without treatment, the process ends with complete atrophy of muscles deprived of innervation and loss of limb mobility (the hand "withers").
Demyelinating neuropathy is characterized by a fairly rapid development of the disease, with sensitivity being impaired and motor functions being lost.
Therefore, the earlier the treatment is started, the greater the chances of fully restoring functions. In advanced cases, the only treatment is often surgical and a complete cure does not always occur.
Diagnostics upper extremity neuropathies
At the first symptoms of discomfort – tingling, numbness, burning, pain, limited motor skills, muscle weakness – you should contact a medical facility.
When interviewing a patient, not only the symptoms that bother him are considered, but also professional risks, the presence of bad habits, previous injuries and the possibility of intoxication. The presence of chronic diseases, past infections, and genetic predisposition are taken into account.
Clinical blood and urine tests are prescribed, as well as blood tests for glucose levels, thyroid hormones, protein levels, and B vitamins. Blood and urine tests for toxic substances may be prescribed.
The nerve trunks are directly palpated, a biopsy of the nerve fibers is performed, and the depth of their damage is determined. A study of the cerebrospinal fluid, testing of nerve reflexes and reactions may be prescribed.
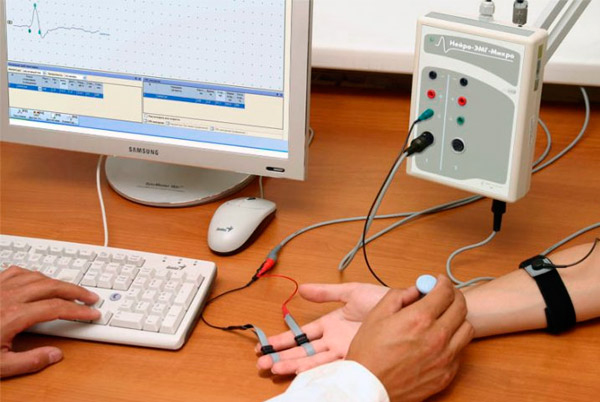
Instrumental diagnostics are carried out: electroneuromyography, radiography, ultrasound examination of the state of internal organs.
Consultations with doctors of other specialties, additional tests and examinations may be prescribed.
Differential diagnosis
Differential diagnostics is carried out based on the results of examination, laboratory and instrumental studies.
Often, with a long-term course of the disease, neuropathy can be determined even visually by the violation of symmetry and motor skills of the upper limbs. Laboratory diagnostics helps to understand the cause of nerve damage, to establish the presence of metabolic disorders, autoimmune processes, inflammations and infections. Specific tests allow to identify characteristic antibodies and antigens, the content of vitamins and proteins in the blood plasma.
Instrumental studies show a decrease in the speed of nerve impulses or its absence (atrophy), a decrease in the activity of muscle fibers.
Special diagnostic tests can reveal which nerve has been damaged. For example, in the case of motor neuropathy of the ulnar nerve, the patient cannot clench the affected hand into a fist because the ring finger and little finger do not bend. He also cannot fan out his fingers and then bring them together, press the hand to the surface of the table and scratch it with the little finger. Sensory reflexes partially or completely disappear on the ring finger and little finger, on the forearm and hand on the elbow side.
External signs of radial nerve neuropathy are a hanging wrist, problems with extension in the wrist and elbow joint, the thumb does not move away from the wrist, and the mobility of the index and middle fingers is impaired. Performing these and other tasks allows you to determine the location of the disorder.
Numbness of the fingers on the hand with compression neuropathy is differentiated from similar symptoms with compression of the spinal cord roots at the corresponding level, in which the filling of the pulse on the radial artery decreases.
Radial nerve neuropathy is differentiated from de Creven's disease, plexitis and other pathologies with similar symptoms. Usually, radiography, computed tomography and nuclear magnetic resonance imaging help to establish the diagnosis.
Who to contact?
Treatment upper extremity neuropathies
Depending on the origin of pathological changes in nerve fibers, treatment is primarily aimed at eliminating the etiologic factor - reducing nerve compression, correcting glucose or thyroid hormone levels, supporting metabolic therapy, restoring trophism and functions of the affected muscles. In case of compression neuropathy, special orthoses, bandages, and splints are used to limit pressure on the affected nerve during movement and at rest. If the cause is professional activity, habits, wearing a cane or crutches, then traumatic factors must be excluded for the duration of treatment.
For more information on treatment methods for upper limb neuropathy, read this article.
Prevention
Neuropathies of the upper limb in most cases have a compression nature and are caused by long monotonous positions of the hands or repetitions of the same movement. It is possible to prevent the development of a pathological process associated with nerve entrapment by observing a certain caution, periodically changing the position of the hands, doing warm-ups for them.
It is important to get rid of bad habits, engage in some kind of sport, monitor a healthy diet, and also monitor your health and promptly consult a doctor when alarming symptoms appear in order to detect a developing disease in time and prevent it from becoming chronic.
Forecast
Mild to moderate neuropathy of the upper extremities is treatable with conservative methods.
It is much more difficult to predict the outcome of an advanced disease; the chronic form will make itself known through periodic exacerbations. Even surgical treatment does not always lead to complete restoration of the sensory-motor functions of the hand.

